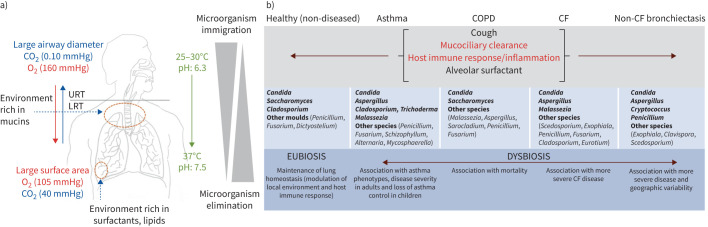
FIGURE 4.
A summary of the homeostatic mechanisms to maintain the lung mycobiome in health and its composition and clinical correlates in chronic respiratory disease. a) Bidirectional flux from the oropharyngeal area, or upper respiratory tract (URT), to the lower respiratory tract (LRT) with biotic (bronchial epithelial cells, respiratory cilia, diameter and cell surface exchanges) and abiotic (temperature, pH, O2/CO2 pressures, airway mucus rich in mucins, a lipid-rich surfactant) factors maintaining a relatively low airway fungal biomass (the mycobiome). The mycobiome maintains a dynamic balance between fungal immigration, driven by inhalation, salivary micro-aspiration and mucosal dispersion, and elimination, driven by cough, mucociliary clearance, innate and adaptive host immune response and antimicrobial activity of alveolar surfactant. This constant dynamic of flux ensures the mycobiome is transient and mobile, with intimate links to the external environment. In health, the lung mycobiome is in a eubiotic state. b) By contrast, dysbiosis of the lung mycobiome occurs across several chronic respiratory diseases including asthma, COPD, cystic fibrosis (CF) and non-CF bronchiectasis. Mechanisms of microbial clearance are differentially impaired based on the pathophysiology of the underlying disease and indicated as normal (black text) to abnormal (red text). In diseased lungs, the mycobiome is more long-lasting and exhibits change, contributing to disease progression.