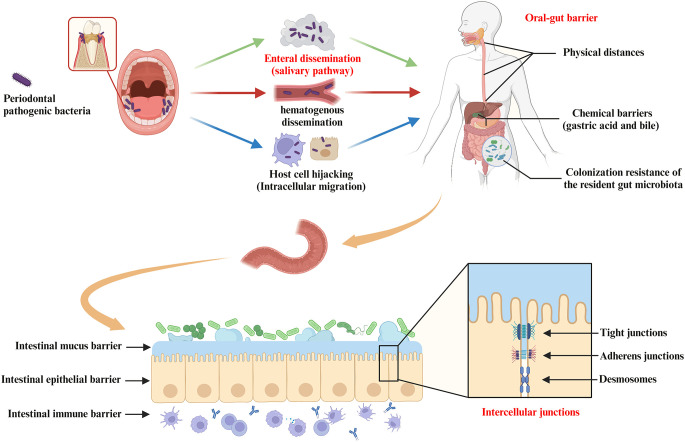
Figure 3.
Pathways of oral bacterial translocation to the gut and host barrier systems limiting oral-gut microbial translocation. Intestinal translocation of periodontal pathogenic bacteria is pathogenically important in the progression of systemic diseases mediated by the oral-gut axis. Possible routes of oral microbiota translocation to the gut include (i) migration by enteral dissemination (salivary route), (ii) colonization of the gut by hematogenous dissemination, and (iii) hijacking of host cells as a vehicle for migration to the gut. First, the oral-gut barrier is one of the important strategies for the host to maintain microbial homeostasis in order to limit microbial translocation between the oral cavity and the gut. The oral-gut barrier includes physical distances and chemical barriers (e.g. gastric acid and bile), as well as colonization resistance of the resident gut microbiota to the intestinal migration of oral microbes with pathogenic potential. If oral bacteria break through the oral-gut barrier to reach the lumen, the barrier function of the intestinal wall is still able to separate the host from adjacent microbiota. The intestinal barrier consists of (i) the intestinal mucus barrier composed of mucin and antimicrobial peptides (AMPs) overlying IEC, (ii) the intestinal epithelial barrier composed of IEC and intercellular junctions (e.g. tight junctions, adherens junctions and desmosomes), and (iii) the intestinal immune barrier composed of innate and adaptive immune cells (gut-associated lymphoid tissue).