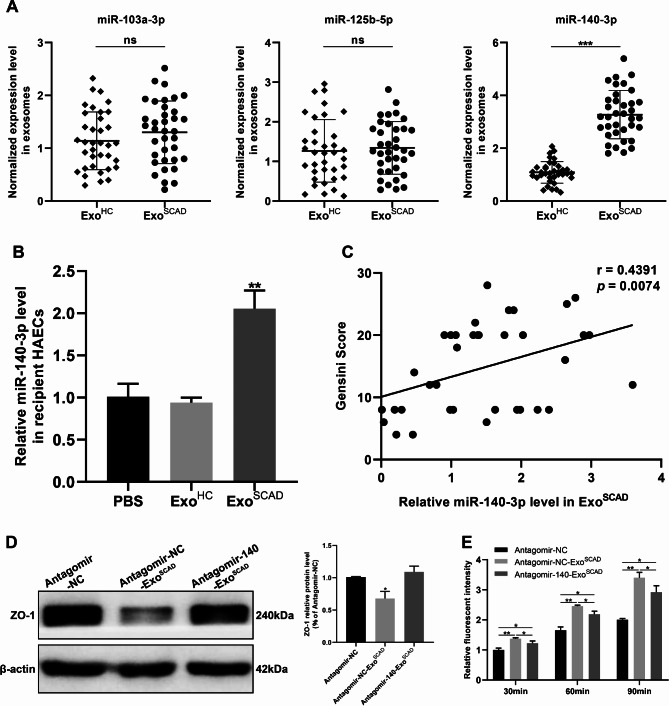
Fig. 4.
ExoSCAD inhibit ZO-1 expression to increase endothelial permeability via transferring highly expressed miR-140-3p into HAECs. (A) RT-qPCR analyses of miR-140-3p and miR-125b-5p expression in ExoSCAD and ExoHC. (B) RT-qPCR analyses of miR-140-3p expression in recipient HAECs after treatment with ExoSCAD, ExoHC or PBS. (C) Correlation of plasma exosomal miR-140-3p levels with Gensini scores in patients with SCAD. (D) Western blot analyses of ZO-1 expression in HAECs treated with antagomir-NC, antagomir-NC-ExoSCAD or antagomir-140-ExoSCAD. Representative blots (left panel) and quantification (right panel) of 3 replicated independent experiments. (E) Quantification of endothelial permeability by calculating the amount of rhodamine-dextran passing through the monolayer of HAECs after 30, 60, and 90 min, respectively (n = 3 per group). ExoHC: plasma exosomes of healthy controls; ExoSCAD: plasma exosomes of patients with stable coronary artery disease; HAECs: human aortic endothelial cells; agomir-140: miR-140-3p agomir; agomir-NC: agomir-140 negative control; antagomir-140: miR-140-3p antagomir; antagomir-NC: antagomir-140 negative control; antagomir-NC-ExoSCAD: ExoSCAD transfected with antagomir-NC; antagomir-140-ExoSCAD: ExoSCAD transfected with antagomir-140. *p < 0.05, **p < 0.01, ***p < 0.001. ns, no significance.