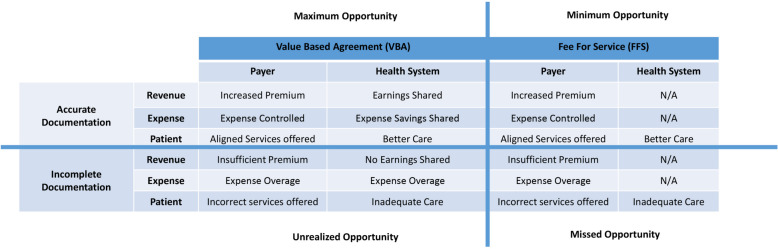
Fig. 3.
Relationship between value-based versus traditional fee for service approaches to risk adjustable conditions. This matrix depicts the perspectives of pertinent stakeholders (payer, health system, patients) in value-based versus fee for service systems, showing the impact of accurate versus incomplete documentation. Only the value-based system aligns all three stakeholders with documentation and better delivery of health care. The consequences of incomplete documentation of chronic health conditions start with, but are not limited to, inadequate health care for the patient. Not shown are the four tiers of a value-based payment shared savings system: maximum opportunity (where all stakeholders derive benefit with shared incentives); minimum opportunity (where the payer derives benefit, but the patient and health system are excluded from shared payment incentives); missed opportunity (where requisite metrics are not achieved and the stakeholders do not benefit); and unrealized opportunity (where all stakeholders could benefit due to shared incentives, but documentation remains suboptimal)