Abstract
Introduction
Children diagnosed with developmental coordination disorder (DCD) exhibit a range of challenges in both gross and fine motor skills, characterised by sluggish and awkward movements. Additionally, they experience deficits in balance and coordination. Without appropriate intervention, these difficulties may endure into adolescence and adulthood, impacting various facets of their daily lives, including learning, social interactions and recreational activities.
Methods and analysis
Employing a randomised controlled trial design, 60 children diagnosed with DCD will be randomly assigned to two groups. The experimental group will receive Baduanjin training in addition to health education, while the control group will undergo health education alone. Following an 8-week intervention period, assessments using motor assessment battery for children-second edition, ProKin 254 Balance Test System will be conducted to evaluate the impact of Baduanjin on the motor coordination and balance in children with DCD. Furthermore, functional near-infrared spectroscopy will be employed to capture haemodynamic data from the children’s brain movement-related cortex during functional activities. These data will be analysed to assess the level of cortical activation, strength of functional connectivity and their correlation with changes in motor function, with the goal of investigating the cerebral blood oxygenation mechanisms underlying the effectiveness of the Baduanjin intervention.
Ethics and dissemination
This study has been submitted for approval and has received ethical clearance from the Medical Ethics Committee of Shanghai Fourth People’s Hospital (2023080-001). The results of the study will be published in a peer-reviewed scientific journal.
Trial registration number
ChiCTR2300078980.
Keywords: Child, China, Clinical Trial, Rehabilitation medicine, Developmental neurology & neurodisability
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study is a clinical randomised controlled trial (RCT).
This study will explore the efficacy of Baduanjin training on motor function in children with developmental coordination disorder (DCD).
The functional near-infrared spectroscopy will be used to clarify the activation level and functional connectivity of the motor-related cortex in the brains of children with DCD before and after the Baduanjin intervention.
As a single-blind RCT, participants will be aware of the subgroups and participant expectations may introduce bias.
Background
Developmental coordination disorder (DCD) is a neurodevelopmental disorder that impairs children’s capacity to execute coordinated motor movements effectively.1 The prevalence of DCD in children varies, with estimates ranging from approximately 2%–20%. Presently, the most widely accepted international figures suggest a prevalence of 5%–6%.2 The fundamental symptoms of DCD primarily revolve around challenges in both gross and fine motor skills,3 usually manifested by slow, clumsy or inaccurate movement charts, deficits in balance and coordination and impairments in fine grasping, dressing, writing and other aspects of daily living and learning.4 5 Children exhibit symptoms during the preschool or school-age years, and if these symptoms remain untreated, they often persist into adulthood, significantly affecting adaptive behaviour and psychosocial well-being.6
Findings from systematic evaluation and meta-analyses have consistently demonstrated that motor skills training yields significant improvements in motor function among children with DCD.7 In the study conducted by Farhat et al, a task-oriented group motor skills training programme was implemented for children with DCD, focusing on fundamental gross motor skills, such as running, jumping, throwing and catching, as well as basic motor skills. The results indicated that an 8-week motor skills training regimen led to significant improvements in the children’s motor assessment battery for children scores, along with enhanced scores in three subscales: manual dexterity, coordination and balance.8 Baduanjin stands as a traditional healthcare exercise distinguished by its unique characteristics rooted in Chinese medicine. Research studies have consistently shown that engaging in regular Baduanjin exercises can be effective in improving various functions, including enhancing the body’s balance, neuromuscular coordination and other related aspects.9,11 In Yuen et al’s study, significant improvements in balance and mobility were observed in patients who had chronic stroke following an 8-week Baduanjin training programme.9 A meta-analysis of the results of a study on the improvement of motor function and balance in patients with Parkinson’s disease with Baduanjin showed that Baduanjin training significantly improved patients' balance function.10 Another meta-analysis11 on the improvement of physical functioning in older adults with Baduanjin also showed that Baduanjin training significantly improved balance and flexibility in older adults. Baduanjin exercises involve a series of movements encompassing flexion and extension of the shoulder, hip, knee and ankle joints. These movements alternate between a horse stance and an upright posture, incorporating shifts in the centre of gravity and occasional heel lifts. These actions induce static contraction of the muscles in the lower limbs, simultaneously stimulating proprioception and vibratory sensation. This comprehensive approach contributes to the effective enhancement of organismal balance function, neuromuscular coordination and motor control ability.12
Moreover, Baduanjin training has demonstrated effectiveness in enhancing activation levels and functional connectivity within specific brain regions. In studies focused on improving activation levels, Baduanjin training exhibited a significant increase in blood oxygen concentrations within the left dorsolateral prefrontal lobe and the right inferior frontal gyrus.13 Additionally, it activated brain regions linked to sensorimotor functions, such as the left postcentral gyrus.14 Regarding the enhancement of functional connectivity within brain regions, Baduanjin training exhibited a noteworthy increase in resting-state functional connectivity. Specifically, there was a significant augmentation in the connectivity between the right ventricle and the left ventral tegmental area with the right insula and right amygdala.15 Nonetheless, recent research has revealed that DCD is not attributable to organic, intellectual or psychological issues. Instead, it is associated with abnormalities in the brain regions responsible for processing motor information. Children diagnosed with DCD exhibit a distinct pattern of cortical activation compared with their neurotypical counterparts.16 Neuroimaging data have revealed notable deficiencies in the activation of functional networks within the prefrontal, parietal and cerebellar regions among children with DCD.17 Additionally, there are significant reductions in functional connectivity between the sensorimotor network and key regions, such as the posterior cingulate cortex, precuneus and posterior middle temporal gyrus.18 Hence, we hypothesise whether Baduanjin training can enhance both the activation levels and functional connectivity within the motor regions of the brain cortex in children with DCD, consequently leading to an improvement in the motor function of these children. Among the brain regions associated with motor function, the primary sensorimotor cortex (SMC(M1+S1), BA4)) is the main brain region involved in motor control19 20; the premotor and supplementary motor cortex (PMC+SMA, BA6) is an important component of the secondary motor area (M2) and plays a key role in the preparation, organisation, execution and regulation of movement.21 Besides, the prefrontal cortex (PFC) is also a crucial region that regulates the complex motor pathways in a holistic manner, including motor behaviours, executive functions and motor planning.22 23 To gain a deeper understanding of the neural mechanisms underlying the improvement of motor function through Baduanjin, it is imperative to investigate the activating effects of Baduanjin training on the motor-related cortex.
Functional near-infrared spectroscopy (fNIRS) is a non-invasive and portable technique for quantifying cortical haemodynamics, providing high temporal and spatial resolution.24 This allows for a comprehensive and quantitative temporal assessment of brain functions.25 In comparison with the stringent physical constraints of the MRI environment and the substantial occurrence of motion artefacts during electroencephalogram data collection, fNIRS exhibits greater resilience to motion artefacts and can be detected to a certain degree during actions.26 The technique indirectly captures regional cortical activation by real-time monitoring of signal changes in cortical oxyhaemoglobin (HbO) and deoxyhaemoglobin (HbR) concentrations during movements.27 28 There have been previous studies employing fNIRS to investigate neurophysiological mechanisms in children with DCD.26 27 29
This study will mark the first exploration of the effectiveness of a Baduanjin training programme for children meeting the Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5) diagnostic criteria for DCD. The primary objectives include investigating the impact of Baduanjin on motor function in children with DCD in comparison with health education. Motor coordination will serve as the primary indicator, while balance and activities of daily living will be considered the secondary indicators. Haemodynamic data from the motor-related cortex of children’s brains during functional tasks will be gathered using fNIRS. These data will be analysed to determine whether the Baduanjin intervention enhances motor function by improving activation and functional connectivity in the motor-related cortex of children with DCD. Additionally, the study aims to explore the cerebral blood oxygenation mechanisms that underlie the efficacy of the Baduanjin intervention.
Methods
Study design
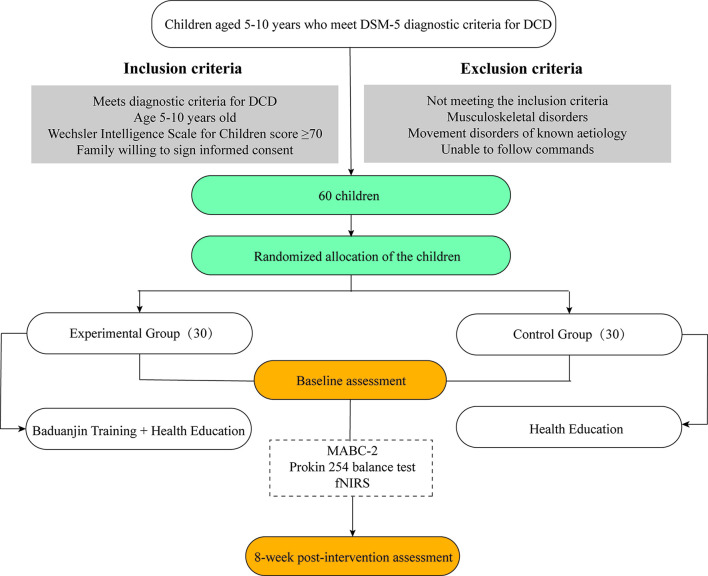
This study is a randomised controlled trial study registered in the Chinese Clinical Trial Registry (ChiCTR2300078980). The study period is 24 months (1 September 2023–1 September 2025). Participants are recruited and treated at the Department of Rehabilitation Medicine, Shanghai Fourth People’s Hospital affiliated to Tongji University, and recruited children with DCD will be randomly assigned to either the experimental group or the control group. The flowchart of the trial is shown in figure 1.
Figure 1. Flowchart of the trial. DCD, developmental coordination disorder; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth edition; fNIRS, functional near-infrared spectroscopy.
Participants
Inclusion criteria
Box 1. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5) diagnostic criteria.
DSM-5 diagnostic criteria.
Acquiring and execution of coordinated motor skills is far below the expected level for age, given opportunity for skill learning. (Children's motor performance is assessed using the motor assessment battery for children-second edition (MABC-2), and a standardised score of 7 or less on the MABC-2 test (with a percentile score of 16 or less) is required for a definitive diagnosis of developmental coordination disorder2).
Motor skill difficulties significantly interfere with activity of daily living and impact academic/school productivity, prevocational and vocational activities, and leisure and play. (Use the developmental childhood disabilities questionnaire to assess whether movement disorders have an impact on a child's daily life or academic performance31).
Onset is in the early developmental period.
Motor skill difficulties are not better explained by intellectual delay, visual impairment or other neurological conditions that affect movement.
The age range of participants considered in this study is between 5 and 10 years.
Children who possess average intelligence, as indicated by a Wechsler Intelligence Scale score of 70 or higher, are capable of actively participating in training.
The family has expressed their willingness to provide informed consent.
Exclusion criteria
Do not meet the above inclusion criteria.
Musculoskeletal disorders.
Movement disorders of known aetiology.
Unable to follow commands.
Shedding criteria
Failure to follow trial protocol treatment after start of trial.
Those who do not wish to remain in the trial.
Exclusion or termination criteria
Serious accidents or adverse reactions during the trial, such as falls, strains and exacerbation of symptoms, should terminate the study.
Serious complications or rapid deterioration during the trial should lead to termination of study treatment.
Participated in other forms of treatment during the trial.
Recruitment procedure
Create recruitment advertisements targeting children with DCD. Disseminate these adverts on the official platforms of Shanghai Fourth People’s Hospital and the Department of Rehabilitation Medicine of Shanghai Fourth People’s Hospital. Additionally, design user-friendly materials for display in the paediatric outpatient area. Parents of potential participants will initiate the screening process by completing the developmental childhood disabilities questionnaire and providing a medical history. This screening aims to exclude other conditions, such as neurological dysfunction, cognitive deficits or psychiatric disorders, which may contribute to motor skill deficits. Subsequently, children identified with unexplained motor skill deficits will undergo further evaluation using the motor assessment battery for children-second edition (MABC-2) standardised test to confirm a diagnosis of DCD. Additionally, the child’s IQ will be assessed using the Wechsler Intelligence Scale for Children to ensure eligibility criteria (IQ≥70). Clinical team members will communicate study details to eligible parents, either during outpatient clinic visits or via telephone, and extend invitations to complete a consent form (see online supplemental material). To maintain ethical standards, all members of the clinical and research teams involved in recruitment will undergo training in good clinical practice.
Randomisation, allocation concealment and blinding
After the baseline assessment, the eligible children with DCD will be randomly assigned to the Baduanjin exercise group or health education group in a 1:1 ratio by simple randomisation. The randomisation sequence will be generated by SAS 9.4 statistical software by an independent researcher who will not be involved in baseline data collection, clinical interventions, functional outcome assessment, data collection or statistical analysis. The allocation concealment will be maintained using sequentially numbered sealed envelopes. Clinicians will determine the availability of subjects to participate in the trial in strict accordance with the inclusion/exclusion criteria. All subjects who are suitable and willing to sign the informed consent form will be randomly assigned. The researcher in charge of subject recruitment will allocate eligible participants a sealed envelope containing the randomisation number, allocation and intervention details; the researcher responsible for recruiting subjects will not be aware of the group allocation, and the clinical intervener will be aware of the subject’s group through the envelope. We cannot blind participants, exercise coaches or intervention supervisors to the assigned treatment, but outcome assessors and statisticians will be blinded to group allocation.
Sample size
Sample size was calculated based on improvements in MABC-2 scores because of the main outcome indicator to assess the improvement of motor function in children with DCD. After reviewing the literature,31 the preintervention MABC-2 score was 58.0±8.7 and postintervention was 65.5±9.9, which was brought into the G-power 3.1.9 software to calculate an effect value of 0.80, and at α=0.05, the test efficacy 1−β = 0.8; the two groups were allocated in a 1:1 ratio, calculated to obtain a sample size of at least 26 participants in each group. Considering the 15% dropout rate, a total of 60 participants are necessary, with 30 participants in each group.
Intervention
Control group
The intervention for children in the control group will be health education, and subjects will participate in a 45 min health education session every 2 weeks for 8 weeks, totalling four sessions. Children in the control group will be kept in the same routine during the trial period and will not be involved in any planned training activities. The health education will be conducted by a rehabilitation doctor who will teach the aetiology, pathogenesis, clinical manifestations and family intervention methods of DCD.
Experimental group
The intervention for children in the experimental group will be Baduanjin training+health education intervention, and the content of Baduanjin training is given as follows.
Two hands hold up the heaven.
Drawing the bow to shoot the eagle.
Separate heaven and earth.
Wise owl gazes backwards.
Sway the head and shake the tail.
Two hands hold the feet.
Clench the fists and glare fiercely.
Bouncing on the toes.9
Each exercise will be divided into three phases: 10 min of preparation, 30 min of training and 10 min of finishing and relaxation, 1 time per day and 5 times per week for 8 weeks, for a total of 40 times (box 2).
Box 2. Baduanjin intervention process.
Preparatory activity (10 min)—under the guidance of the rehabilitation therapist, perform whole body joint activities, stretch the body and warm up fully.
Baduanjin training (30 min)—essentials of Baduanjin movements: during practice, the body, breathing and mind should harmoniously coordinate. Maintain a natural body posture with standardised movements. Breathe evenly, avoiding forceful inhalation, and synchronise breathing with body movements. Keep the mind focused and the spirit concentrated. Aim for precision, skill and consistency in movements, gradually achieving the organic integration of movement, breathing and mental focus. Cultivate mental relaxation and tranquillity, facilitating a fluidity in body movements. Throughout the exercise, prioritise flexible and powerful movements, grounded in the relaxation of all body muscles, combining gentleness with strength and coherence.
Tidy up and relax (5 min)—the child stands still, relaxes the whole body, breathes evenly and is in a natural state, continuing until the body is comfortable.
Before commencing the trial, a training session will be conducted, during which the researcher will provide personalised, on-site instruction to each child. The interventionist of this trial is the postgraduate student of rehabilitation majoring in Chengdu Sport University, School of Sports and Health, class of 2017, who has been engaged in group therapy of Baduanjin in children’s rehabilitation, has a solid theoretical foundation and technical skills of Baduanjin, has rich experience in teaching and is able to control the training intensity to ensure the safety of the movement. Encouragement will be extended to parents to participate in this session, fostering a better understanding of Baduanjin movements and enabling them to supervise their children’s practice at home. Subsequent to the instruction, another researcher will conduct an assessment to confirm that each child has mastered every movement of Baduanjin. Each child’s parents will receive a prerecorded teaching video and a notebook during the training session, with the expectation that they will guide or assist their children in practising Baduanjin exercises at home. The 8-week trial period will then commence, both at home and in the hospital. Children in the trial group will attend the hospital two times a week for Baduanjin training, while their parents will supervise the remaining three sessions at home. Parents will record these sessions and share them with researchers via WeChat. Record sheets will be completed after each session, and researchers will routinely check the children’s daily record books to ensure compliance with home practice requirements.
Measurements
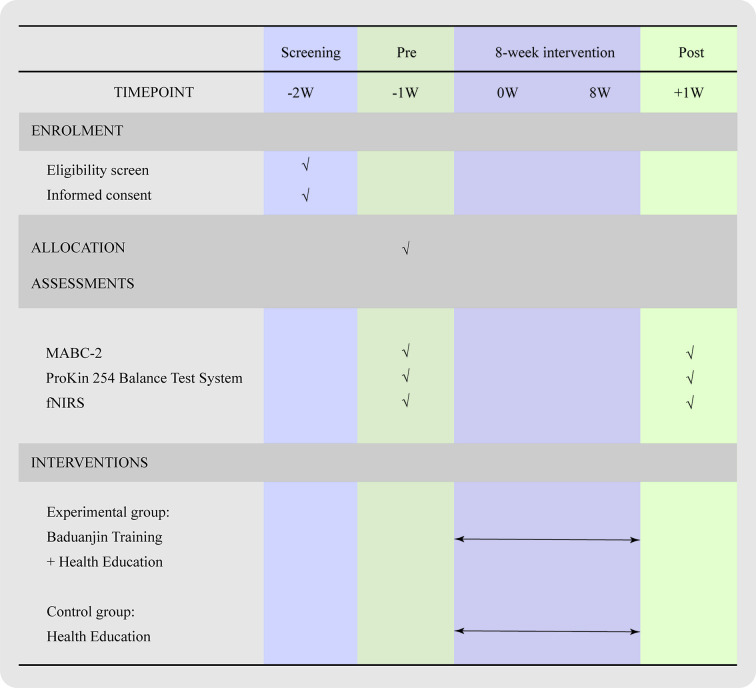
All assessments will be carried out by an assessor who will have no knowledge of baseline and post-treatment group assignments (the schedule is shown in figure 2). The assessor will be trained in testing procedures prior to the start of the study.
Figure 2. Schedule of enrolment, assessments and interventions. fNIRS, functional near-infrared spectroscopy; MABC-2, motor assessment battery for children-second edition.
Main outcome indicators
Motor Assessment Battery for Children-Second Edition
Children’s motor coordination will be evaluated using the MABC-2 test, which is based on the Chinese norms and includes three main sections: manual dexterity, aiming and catching, and balance. These components capture fundamental aspects of children’s motor coordination during their growth and development. The MABC-2 test provides a comprehensive evaluation, encompassing all aspects of children’s motor coordination.32 The study includes three distinct age groups: 3–6 years old, 7–10 years old and 11–16 years old, each with eight items. Raw scores obtained will be transformed into standardised scores ranging from 1 to 19, using the standard score conversion table provided in the MABC-2 User Manual.
Secondary outcome indicators
ProKin 254 Balance Test System
The ProKin 254 Balance Test System (ProKin 254, TecnoBody Company, Italy) will be used to test static balance as well as dynamic postural stability. The static balance index employs both movement length and movement ellipse area, representing the total distance and area of the centre of pressure moved by the patient while at rest. This reflects the extent of swaying in the patient’s centre of gravity, with a larger value indicating poorer static postural stability.33 The dynamic balance index is the total offset index, referring to the angle formed by the patient’s overall offset position and the vertical centerline. A larger value indicates inferior dynamic postural stability. The index for active postural control ability is the stability limit value, calculated as the ratio of the total distance tilted by the patient in all directions to the ideal distance determined by the system based on the patient’s height and weight. A higher value signifies better active postural control ability and improved balance function.
Neuroimaging assessment
fNIRS measures cortical activity during functional tasks through the use of a sensing cap. Given that the MABC-2 is a standardised test comprehensively evaluating all aspects of children’s motor coordination, task activities within the MABC-2 test will be used to represent activities assessing children’s motor functioning in both groups. As the MABC-2 test items vary for different age groups (3–6 years old and 7–10 years old), to ensure task consistency, items overlapping in the three major modules of the MABC-2—namely, tracing the trajectory, throwing the bag with one hand and balancing with one leg—will be selected. These activities represent fine manual dexterity, hand–eye coordination and balance aspects for the children. In this experiment, NirSmart-6000A equipment (Danyang Huichuang Medical Equipment Co., Ltd., China) was used to continuously measure and record the concentration changes of brain oxygenated haemoglobin (HbO) and deoxyhaemoglobin (HbR) during the task. The system consists of a near-infrared light source (light emitting diodes) and avalanche photodiodes as detectors, with wavelengths of 730 nm and 850 nm, respectively, and a sampling rate of 11 Hz. The experiment uses 23 light sources and 15 detectors to form 49 effective channels, the average distance between the source and the detector is 3 cm (range 2.7–3.3 cm), with reference to the international 10/20 system for positioning. Regions of interest (ROI) will be chosen from the bilateral SMC (BA4) region, PMC+SMA (BA6) region and PFC region.
Data processing
fNIRS data preprocessing
The NirSpark software (HuiChuang, China) package was used to preprocess fNIRS signals.34 The low-pass filter based on the canonical haemodynamic response function will be used to reduce/remove high-frequency noise, with a cut-off frequency of 0.15 Hz. The wavelet minimum description length algorithm will be used to remove artefacts caused by respiration, heartbeat, vasodilation and other motion-related disturbances.35 For data output, the raw optical density data will be converted into relative change curves of HbO and HbR using modified Beer–Lambert’s law.36 Given that HbO exhibits a higher signal-to-noise ratio than HbR, demonstrates better correlation with blood oxygen-level-dependent signals and is more sensitive to changes in cerebral blood flow, we will use HbO to assess the participants' brain activation status.23 37
fNIRS data analysis
After data preprocessing, the ∆HbO obtained from the three tests for each task will be stacked and averaged to obtain the time-series variation of each channel under each task for each subject. Data will be averaged for all channels in each brain region and then averaged for all subjects. General linear model analysis will be performed using the NirSpark toolkit to obtain the activation coefficient β value of the ROI representing the magnitude of neuronal activation of cortical neurons under this channel in the subject’s task condition.38
Brain functional connectivity analysis
Functional connectivity between different channels refers to the synchronised activation of various channels during a specific task, providing insight into the functional synchrony and coordination between distinct brain regions. This is assessed by calculating the correlation coefficient of ΔHbO time series between two channels, a method known as correlation analysis. In this study, Pearson’s correlation analysis will be employed to compute the correlation coefficient (r) between channels, serving as an indicator of functional connectivity. The correlation coefficient ranges from −1 to 1, with a higher absolute value indicating stronger functional connectivity between channels. A correlation coefficient |r|≥0.7 is considered strong, 0.5≤|r|<0.7 is deemed moderate and 0.3≤|r|<0.5 is considered weak. Channel pairs with moderate or strong correlations are defined as having functional connectivity.
Statistical methods
Analyses will be conducted using IBM SPSS 25.0 statistical software. For normally distributed measures, results will be presented as (Mean±SD), while skewed measures will be represented as M (P25 and P75). Two independent samples t-test will be applied for normally distributed measures that meet variance χ2 criteria, and the Wilcoxon rank-sum test will be used for those not meeting these criteria. Within-group comparisons before and after the intervention will be performed using the paired t-test or Wilcoxon paired rank-sum test. The χ2 test will be employed for count data. Correlations between the HbO β values in the ROIs that exhibit significant changes before and after the intervention and corresponding functional scores on the MABC-2 scale will be analysed.
The data will be analysed employing an intention-to-treat analysis strategy, which includes individuals who drop out of treatment but have completed the outcome indicators in the analysis.
Withdrawal and adverse events
Each group of children may experience dropouts from the trial. The investigator will be obligated to document withdrawal information, including the reason and time of withdrawal. Simultaneously, researchers will record adverse events during the trial, noting the type, frequency, management and outcomes of adverse events in the form of a common reporting format.
Adherence analysis
The degree of adherence can be judged according to criteria specified in the clinical study protocol, and those who meet this criterion are said to have a high level of adherence; otherwise, they have a low level of adherence.
Trial adherence=number of trials the subject has undergone/total number of trials the subject should have undergone×100%.
Data management
The study report form (SRF) will be completed by the study subjects and outcome evaluators. Each enrolled subject is required to fill out the SRF, which includes an activity log sheet, relevant outcome indicator test scales and an adverse event record sheet, among other components. On completion, the project manager will review the SRF, and the data entry clerk will then organise the data and manage the original forms uniformly. To maintain confidentiality, subjects' names will not be included in the SRF; instead, only the phonetic abbreviation and assigned trial number will be used. Any relevant study summaries, articles and public publications will use only initials and numbers as necessary.
Ethics and dissemination
This study has been submitted for approval and has received ethical clearance from the Medical Ethics Committee of Shanghai Fourth People’s Hospital (2023080–001) and registered on the website of China Clinical Trial Registry (http://www.chictr.org.cn, identification number ChiCTR2300078980). Parents of participating children will sign an informed consent form after thoroughly comprehending the study protocol, its significance and potential benefits and risks. To foster positive and compliant participation, children involved in the trial will receive free-of-charge treatment throughout the study duration. The study will adhere to the guidelines outlined in the Data Protection Act and the Declaration of Helsinki. Access to all participant data, related documents and questionnaires—particularly those containing identifying information—will be restricted solely to the research team. Patient-identifiable data related to the study will be securely deleted or destroyed within 6 months after the study concludes. Researchers are strictly prohibited from disclosing patient data in any form to individuals not directly involved in the study. The results of the study will be published in a peer-reviewed scientific journal.
Patient and public involvement statement
This trial is currently in the recruitment phase. No participant has been involved in the trial. The patients are not involved in the design, or conduct, or reporting of our research.
Discussion
DCD is prevalent worldwide, and motor skill impairments significantly impact children’s daily activities and psychosocial well-being. This protocol employs a randomised controlled design to intervene with children diagnosed with DCD using the traditional Chinese health-improving exercise method of Baduanjin. The anticipated outcome of this study is an improvement in the motor function of children with DCD, consequently enhancing their self-care abilities and social adaptation. Thus, this programme holds promise as an exercise intervention, offering new perspectives for the rehabilitation of children with DCD.
Furthermore, this study will employ an innovative approach by using fNIRS to capture haemodynamic data from the motor-related cortex in children with DCD during functional tasks, such as manual dexterity, balance and coordination. The analysis will encompass the evaluation of cortical activation levels and the strength of functional connectivity. These metrics will be correlated with changes in motor function, providing a comprehensive assessment of the efficacy of Baduanjin exercise in improving the motor function of children with DCD. This approach aims to explore the cerebral blood oxygenation mechanisms that underlie the effectiveness of Baduanjin exercise, covering both peripheral manifestations and central features.
Hence, the key advantages of this study can be summarised as follows. (1) Investigating the impact of Baduanjin exercise on the motor function of children with DCD, aiming to identify a novel approach for DCD rehabilitation intervention. (2) Using fNIRS to assess the activation of the cortex related to brain motor function during functional activities in children with DCD, providing insights into the cerebral blood oxygenation mechanisms underlying the effectiveness of Baduanjin exercise.
supplementary material
Footnotes
Funding: The author disclosed receipt of the following financial support for the publication of this article: This work was supported by the Scientific Research Project of Traditional Chinese Medicine of Shanghai Hongkou District Health and Wellness Committee (grant number HKOGYOY-ZY-2023-24); the Research Launch Project of The Fourth People's Hospital Affiliated to Tongji University (grant number sykyqd02001).
prepub: Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-084061).
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Correction notice: This article has been corrected since it was published. The co-corresponding author has been added.
Contributor Information
Jiaxin Gao, Email: gjx@stu.cdutcm.edu.cn.
Xiaohua Ke, Email: kxh22@tongji.edu.cn.
Dunbing Huang, Email: huang1915@tongji.edu.cn.
Yangxin Wu, Email: wyxzjj27@163.com.
Xiaqing Xu, Email: xiaqingxu62@gmail.com.
Hongfei Ren, Email: 17689400552@163.com.
Anren Zhang, Email: anren0124@tongji.edu.cn.
Wei Song, Email: songwei94@tongji.edu.cn.
References
- 1.Lyu Z, Huang M, Kang B, et al. Interpretation on physical therapy management of children with developmental coordination disorder: an evidence-based clinical practice guideline from the Academy of Pediatric Physical Therapy of the American Physical Therapy Association in 2020. Chin J Appl Clin Pediatr. 2021;36:1710–5. doi: 10.3760/cma.j.cn101070-20210603-00633. [DOI] [PubMed] [Google Scholar]
- 2.Blank R, Barnett AL, Cairney J, et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev Med Child Neurol. 2019;61:242–85. doi: 10.1111/dmcn.14132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smits-Engelsman B, Verbecque E. Pediatric care for children with developmental coordination disorder, can we do better? Biomed J. 2022;45:250–64. doi: 10.1016/j.bj.2021.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dionne E, Bolduc M-È, Majnemer A, et al. Academic Challenges in Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. Phys Occup Ther Pediatr. 2023;43:34–57. doi: 10.1080/01942638.2022.2073801. [DOI] [PubMed] [Google Scholar]
- 5.Van der Linde BW, van Netten JJ, Otten B, et al. Activities of Daily Living in Children With Developmental Coordination Disorder: Performance, Learning, and Participation. Phys Ther. 2015;95:1496–506. doi: 10.2522/ptj.20140211. [DOI] [PubMed] [Google Scholar]
- 6.Harrowell I, Hollén L, Lingam R, et al. Mental health outcomes of developmental coordination disorder in late adolescence. Dev Med Child Neurol. 2017;59:973–9. doi: 10.1111/dmcn.13469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu JJ, Burnett AF, Sit CH. Motor Skill Interventions in Children With Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2018;99:2076–99. doi: 10.1016/j.apmr.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Farhat F, Hsairi I, Baati H, et al. The effect of a motor skills training program in the improvement of practiced and non-practiced tasks performance in children with developmental coordination disorder (DCD) Hum Mov Sci. 2016;46:10–22. doi: 10.1016/j.humov.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Yuen M, Ouyang HX, Miller T, et al. Baduanjin Qigong Improves Balance, Leg Strength, and Mobility in Individuals With Chronic Stroke: A Randomized Controlled Study. Neurorehabil Neural Repair. 2021;35:444–56. doi: 10.1177/15459683211005020. [DOI] [PubMed] [Google Scholar]
- 10.Lai J, Cai Y, Yang L, et al. Effects of Baduanjin exercise on motor function, balance and gait in Parkinson’s disease: a systematic review and meta-analysis. BMJ Open. 2022;12:e067280. doi: 10.1136/bmjopen-2022-067280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin H, Wan M, Ye Y, et al. Effects of Baduanjin exercise on the physical function of middle-aged and elderly people: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther . 2023;23:38. doi: 10.1186/s12906-023-03866-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye Y, Zhao F, Sun S, et al. The effect of Baduanjin exercise on health-related physical fitness of college students: A randomized controlled trial. Front Public Health. 2022;10:965544. doi: 10.3389/fpubh.2022.965544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yao L, Sun G, Wang J, et al. Effects of Baduanjin imagery and exercise on cognitive function in the elderly: A functional near-infrared spectroscopy study. Front Public Health. 2022;10:968642. doi: 10.3389/fpubh.2022.968642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuan X, Zhong X, Wang C, et al. Temporo-Parietal cortex activation during motor imagery in older adults: A case study of Baduanjin. Brain Cogn. 2023;173:106103. doi: 10.1016/j.bandc.2023.106103. [DOI] [PubMed] [Google Scholar]
- 15.Liu J, Tao J, Xia R, et al. Mind-Body Exercise Modulates Locus Coeruleus and Ventral Tegmental Area Functional Connectivity in Individuals With Mild Cognitive Impairment. Front Aging Neurosci. 2021;13:646807. doi: 10.3389/fnagi.2021.646807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cavalcante Neto JL, Steenbergen B, Zamunér AR, et al. Wii training versus non-Wii task-specific training on motor learning in children with developmental coordination disorder: A randomized controlled trial. Ann Phys Rehabil Med. 2021;64:101390. doi: 10.1016/j.rehab.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Wilson PH, Smits-Engelsman B, Caeyenberghs K, et al. Cognitive and neuroimaging findings in developmental coordination disorder: new insights from a systematic review of recent research. Dev Med Child Neurol. 2017;59:1117–29. doi: 10.1111/dmcn.13530. [DOI] [PubMed] [Google Scholar]
- 18.Rinat S, Izadi-Najafabadi S, Zwicker JG. Children with developmental coordination disorder show altered functional connectivity compared to peers. Neuroimage Clin. 2020;27:102309. doi: 10.1016/j.nicl.2020.102309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zang Z, Song T, Li J, et al. Severity-dependent functional connectome and the association with glucose metabolism in the sensorimotor cortex of Parkinson’s disease. Front Neurosci. 2023;17:1104886. doi: 10.3389/fnins.2023.1104886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y, Wang W-W, Hua X-Y, et al. Patterns of cortical reorganization in facial synkinesis: a task functional magnetic resonance imaging study. Neural Regen Res. 2018;13:1637–42. doi: 10.4103/1673-5374.235304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xia W, Dai R, Xu X, et al. Cortical mapping of active and passive upper limb training in stroke patients and healthy people: A functional near-infrared spectroscopy study. Brain Res. 2022;1788:147935. doi: 10.1016/j.brainres.2022.147935. [DOI] [PubMed] [Google Scholar]
- 22.Price AE, Sholler DJ, Stutz SJ, et al. Endogenous Serotonin 5-HT(2A) and 5-HT(2C) Receptors Associate in the Medial Prefrontal Cortex. ACS Chem Neurosci. 2019;10:3241–8. doi: 10.1021/acschemneuro.8b00669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deng J, Lei T, Du X. Effects of sensory integration training on balance function and executive function in children with autism spectrum disorder: evidence from Footscan and fNIRS. Front Psychol. 2023;14:1269462. doi: 10.3389/fpsyg.2023.1269462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karunakaran KD, Peng K, Berry D, et al. NIRS measures in pain and analgesia: Fundamentals, features, and function. Neurosci Biobehav Rev. 2021;120:335–53. doi: 10.1016/j.neubiorev.2020.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Wilcox T, Biondi M. fNIRS in the developmental sciences. Wiley Interdiscip Rev Cogn Sci. 2015;6:263–83. doi: 10.1002/wcs.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caçola P, Getchell N, Srinivasan D, et al. Cortical activity in fine-motor tasks in children with Developmental Coordination Disorder: A preliminary fNIRS study. Int J Dev Neurosci. 2018;65:83–90. doi: 10.1016/j.ijdevneu.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Zhao W, Hui M, Zhang X, et al. The Relationship between Motor Coordination and Imitation: An fNIRS Study. Brain Sci. 2021;11:1052. doi: 10.3390/brainsci11081052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han YMY, Chan MMY, Shea CKS, et al. Neurophysiological and behavioral effects of multisession prefrontal tDCS and concurrent cognitive remediation training in patients with autism spectrum disorder (ASD): A double-blind, randomized controlled fNIRS study. Brain Stimul. 2022;15:414–25. doi: 10.1016/j.brs.2022.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Joshi S, Weedon BD, Esser P, et al. Neuroergonomic assessment of developmental coordination disorder. Sci Rep. 2022;12:10239. doi: 10.1038/s41598-022-13966-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Psychiatric Association Diagnostic stat. man. ment. disord. DSM-5. 2013. https://psychiatryonline.org/dsm Available.
- 31.Cavalcante Neto JL, Steenbergen B, Tudella E. Motor intervention with and without Nintendo Wii for children with developmental coordination disorder: protocol for a randomized clinical trial. Trials. 2019;20:794. doi: 10.1186/s13063-019-3930-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ke L, Du W, Wang Y, et al. The Movement ABC-2 Test in China: Comparison with UK norms for 3-10 year olds. Res Dev Disabil. 2020;105:103742. doi: 10.1016/j.ridd.2020.103742. [DOI] [PubMed] [Google Scholar]
- 33.Chen Z, Shen Z, Ye X, et al. Association between Foot Posture Asymmetry and Static Stability in Patients with Knee Osteoarthritis: A Case-Control Study. Biomed Res Int. 2020;2020:1–8. doi: 10.1155/2020/1890917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang S, Peng C, Yang Y, et al. Resting-state brain networks in neonatal hypoxic-ischemic brain damage: a functional near-infrared spectroscopy study. Neurophotonics. 2021;8:025007. doi: 10.1117/1.NPh.8.2.025007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ye JC, Tak S, Jang KE, et al. NIRS-SPM: statistical parametric mapping for near-infrared spectroscopy. Neuroimage. 2009;44:428–47. doi: 10.1016/j.neuroimage.2008.08.036. [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi M, Hori E, Takamoto K, et al. Brain cortical mapping by simultaneous recording of functional near infrared spectroscopy and electroencephalograms from the whole brain during right median nerve stimulation. Brain Topogr. 2009;22:197–214. doi: 10.1007/s10548-009-0109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strangman G, Culver JP, Thompson JH, et al. A quantitative comparison of simultaneous BOLD fMRI and NIRS recordings during functional brain activation. Neuroimage. 2002;17:719–31. doi: 10.1006/nimg.2002.1227. [DOI] [PubMed] [Google Scholar]
- 38.Kim HY, Kim EJ, You JSH. Adaptive locomotor network activation during randomized walking speeds using functional near-infrared spectroscopy. Technol Health Care. 2017;25:93–8. doi: 10.3233/THC-171310. [DOI] [PubMed] [Google Scholar]
- 39.Schoemaker MM, Reinders-Messelink AJ, Kloet AJ. Coördinatievragenlijst voor Ouders (CVO) - translation of DCD-questionnaire By Wilson (2007) 2008