Dear Editors,
Here we report the case of a 37‐year‐old Caucasian male who experienced a burning sensation and thickening of the palms that arose every time he bathed or showered. This condition started one month before we became aware of it.
Medical history and physical examination revealed nothing specific; however, the thickening of the palms of the hands was quite suggestive. We then carried out a test in which the patient immersed his hands for five minutes in warm water. This caused the appearance of a strong thickening of the palms, reduction of the dermatoglyphic, whitish bumps, and a burning sensation as reported.
The clinical aspect and history led us to diagnose aquagenic‐palmoplantar‐keratoderma (APK).
APK is characterized by excessive wrinkling of the palms and eventually the soles, sometimes with a stinging sensation associated with plaques and papules, typically after water exposure in young adults. It is reported that patients have the first episode minutes after a bath or a shower, and the episode can be re‐triggered by immersion of the hands in water for 3–5 minutes (bucket sign). 1
Since it is not a congenital condition, some authors suggest calling it sporadic or pseudo aquagenic palmoplantar keratoderma (SAKP or PAKP). 2
Other atypical sites involved, apart from the palmoplantar site, could be the forehead, heel, and dorsal aspect of the hands, which are rarely unilateral. Finally, after the episode, most cases are resolved within 20 minutes.
PAPK has been reported to be associated with several conditions, including cystic fibrosis, rheumatological diseases, marasmus, atopic dermatitis, cancer, and drug reactions. Various tests to exclude potential underlying pathologies have been suggested. 3
Primary treatment is represented by topical antiperspirant, which often controls symptoms. It is also known that this condition can be self‐resolutive over the years.
In the medical literature, some authors assert that dermatoscopy is an essential technique for diagnosing this type of condition and that dermatoscopic characteristics may be crucial for workup. 4 We are not of this opinion: we believe that dermatoscopy, although applicable, in some circumstances may be an ancillary and sometimes superfluous examination.
Specifically, while the author of this article was performing the video dermatoscopy examination, the helping doctor had already made the diagnosis based on the clinical signs and bucket test positivity, indicating that this information is sufficient to provide a diagnosis, as in this case. 5
However, this does not mean that dermatoscopy does not provide clues, and it does show the affected epidermal structure in relation to the anatomopathologic changes in a highly suggestive and educative way, as we reported in this clinical case (Figure 1).
FIGURE 1.
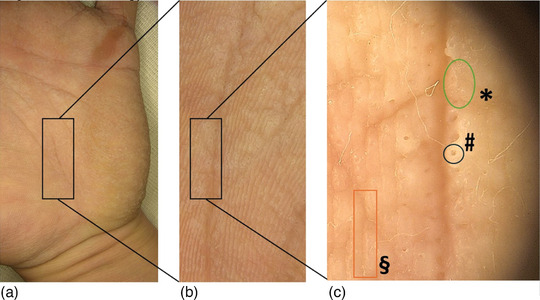
(a) Photo of part of the left palm; note the formation of papules, whitish patches and the general thickening of the dermatoglyphics. (b) Close‐up of the middle part of the palm. (c) Dermoscopy of the selected zone. In the green oval (*), localized hyperkeratosis caused by barrier dysfunction forms a whitish‐greyish papule. In the black circle (#), a highly dilated acrosyringium outlet is surrounded by hyperkeratosis due to hyper sweat tube distortion in the stratum corneum. In the red rectangle (§), the thickening of the skin crests almost obliterates the dermatoglyphics. Dermoscopy at 40 x magnification.
CONFLICT OF INTEREST STATEMENT
None.
REFERENCES
- 1. Yang K, Zhou C, Luke J. Aquagenic wrinkling of the palms: review of the literature. Clin Exp Dermatol. 2022;47(11):1910‐1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Atzori L, Ferreli C, Rongioletti F. Aquagenic (pseudo) keratoderma (aquagenic palmoplantar keratoderma, aquagenic wrinkling of palms). Clin Dermatol. 2021;39(2):256‐260. [DOI] [PubMed] [Google Scholar]
- 3. Uyar B. Aquagenic Syringeal Acrokeratoderma. Indian J Dermatol. 2014;59(6):632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dermoscopic features of aquagenic palmar keratoderma. J Am Acad Dermatol. 2016;74(5):AB105. [Google Scholar]
- 5. Sezer E, Erkek E, Duman D, Şahin S, Çetin E. Dermatoscopy as an Adjunctive Diagnostic Tool in Aquagenic Syringeal Acrokeratoderma. Dermatology. 2012;225(2):97‐99. [DOI] [PubMed] [Google Scholar]


