Abstract
ABSTRACT
Objective
To assess service availability and readiness of health facilities to provide maternal and newborn care in the Kilimanjaro region, northern Tanzania: a study conducted between August to October 2022.
Design
The study used a cross-sectional design by adopting WHO Service Availability and Readiness Assessment tool to assess basic maternal, newborn and child health services delivery in the health facilities of the Kilimanjaro region.
Setting
The study was conducted in seven districts of Kilimanjaro region at health facilities with a labour ward and where delivery and maternal services for women and neonatal care were offered.
Participants
The study included all district hospitals, two selected health centres and two dispensaries within every district with high utilisation of delivery services as well as the regional hospital of Kilimanjaro region making a total of 37 health facilities that were assessed.
Primary outcome
Basic emergency obstetric and newborn care (BEmONC) service availability, BEmONC service readiness, comprehensive emergency obstetric and newborn care (CEmONC) service availability and CEmONC service readiness.
Results
A total of 37 facilities were enrolled that included 14 dispensaries, 14 health centres, 8 district hospitals and 1 regional hospital. The study highlights that majority of the signal functions are available in all levels of health facilities with overall readiness scores in BEmONC and CEmONC being 83% and 98.87%, respectively. However, the study reports that 40.5% of health facilities do not conduct death reviews. Similarly, on-job trainings regarding maternal and newborn healthcare was low, with only 29.8% of all healthcare workers in the region received training for the past 2 years.
Conclusion
Despite progress, challenges persist in delivering tailored maternal and newborn healthcare services in Kilimanjaro region. The study revealed strong readiness in essential care functions, but shortcomings in maternal and neonatal death reviews and training, emphasise the need for improved practices to further enhance maternal and newborn health outcomes.
Keywords: Maternal medicine, REPRODUCTIVE MEDICINE, PAEDIATRICS, Cross-Sectional Studies
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The study offered valuable insights into maternal and newborn health service availability and readiness.
Cross-sectional design restricts establishment of causal relationship between variables.
The study’s sample was confined to public health facilities limiting its generalisability to other healthcare settings.
Introduction
Providing tailored maternal and newborn healthcare services remains a significant challenge in Africa.1 The scarcity of essential resources contributes to the difficulties in reducing maternal and neonatal mortality rates (NMRs).1 2 Absence of high-quality healthcare services in healthcare facilities, inadequacies in referral systems and the lack of healthcare-seeking behaviours among pregnant women are factors that serve as poor indicators for progress in lowering the rates of maternal and NMRs.1
The Sustainable Development Goal 3.1, which seeks to lower maternal mortality rates to 70 per 100 000 and NMRs to 20 per 1000 live births by 2030, is still a challenge in many countries in Africa.2 Though countries are making progress towards achieving this goal, some areas such as Sub-Saharan Africa still remain a distant prospect in achieving it.1 In 2020, Sub-Saharan Africa accounted for 70% of global maternal deaths, totalling 545 maternal deaths, and 43% of NMRs, equivalent to 27 deaths per 1000 live births.3 4 According to Tanzania Demographic Health Survey data of 2015, maternal and NMRs were reported to be 556 per 100 000 live births and 25 per 1000 live births, respectively5 which were still high implying that achieving the SDG target in these countries is possible but requires exceptional dedication and additional efforts.
The importance of care during the day of birth cannot be overstated, as maternal and newborn deaths during this period are critical.6 7 Access to high-quality care is pivotal, and it involves the provision of essential life-saving interventions.7 Antenatal care services play a crucial role in preventing and managing various health conditions during pregnancy such as hypertensive disorders, syphilis, tetanus and Malaria which affects mothers and newborns.7 It also serves as a means to promote proper health behaviours such as timely initiation of breastfeeding, postnatal care and planning for optimal pregnancy spacing.7 8
Furthermore, the availability of emergency obstetric and newborn care (EmONC) services in each health facility is a key strategy in lowering maternal and newborn deaths.7 The strategy aims to equip health facilities to deal with major causes of direct obstetric emergencies in a timely manner that accounts for most maternal and newborn deaths.9 The UN recommends at least one comprehensive EmONC (CEmONC) facility and four basic EmONC (BEmONC) facilities per 500 000 population1 to enhance maternal and newborn health by ensuring timely access to essential emergency care services and as of 2015 40% of all the regions in Tanzania had attained or exceeded the recommended number of four BEmONC facilities and 76% of all the regions had at least one CEmONC facility per 500 000 population;10 however, their ability to carry out essential emergency care services was still inadequate.8
Tanzania’s government has launched a number of programmes aimed at lowering maternal and newborn mortality as a result of the country’s recognition of the critical need of improving maternal and newborn health, as in 1975 the extended programme of immunisation was initiated and in 2016–2020 the national roadmap strategic plan to Improve Reproductive, Maternal, Newborn, Child and Adolescent Health was initiated.11
Despite these considerable strides in healthcare, challenges persist in meeting the UN’s process indicators for obstetric care in Tanzania. These challenges revolve around the availability of basic medical equipment and an adequate supply of healthcare personnel. While there are an adequate number of CEmONC facilities in place, their distribution remains uneven, and some of these facilities offer BEmONC services that fall short of the required standards.8 To address these concerns and gain a comprehensive understanding of the state of maternal and newborn healthcare services, this study aims to assess the service availability and readiness of maternal and newborn healthcare services in the Kilimanjaro region, Northern Tanzania.
Methods
Study design
This was a facility-based cross-sectional survey which was conducted from August to October 2022 in the Kilimanjaro region, northern Tanzania.
Study Area
The study was conducted in seven districts within the Kilimanjaro region, specifically at health facilities equipped with labour wards and providing delivery, maternal and neonatal care services. The region’s population as of 2022 was 1 861 934 accounting for 3.01% of the country’s total population.12
Sampling
The study employed a purposive sampling technique to assess maternal and neonatal healthcare services in the Kilimanjaro region. A total of 37 health facilities were included in the study, comprising one regional hospital, two selected health centres and two dispensaries from each district with high utilisation of delivery services, along with all district hospitals that is one district hospital for each district except for Moshi DC which has two district designated hospital (DDH). The selection of these facilities was based on recommendations from regional and district medical offices, with a focus on facilities serving a high number of mothers.
The sampling frame exclusively included public health facilities providing basic maternal, newborn and child healthcare across the region where as of 2021 the region had 1 regional hospital, 8 district hospitals, 31 health centres and 205 dispensaries. This approach ensured that the study covered all types of facilities mandated by the government to offer these services. Public facilities were chosen due to their widespread utilisation by the general community, making them a reflection of the overall health of the population in the country.1 This comprehensive sampling strategy allowed for a thorough assessment of maternal and newborn healthcare services in the Kilimanjaro region.
Tanzanian Healthcare System
Tanzania’s healthcare system has four levels. The first level comprises dispensaries serving 4000 to 10 000 people, referring to second level which is health centres serving 50 000 people which in turn refer cases to third level which are district hospitals serving approximately 250 000 people. The fourth level consists of regional or referral hospitals.13
In accordance to the National Road Map Strategic Plan to improve Reproductive, Maternal, Newborn, Child and Adolescent Health also known as ‘One plan III’, all dispensaries and health centres are required to provide delivery services, including BEmONC services while all districts, regional and tertiary or referral hospitals are required to provide CEmONC services.10 Furthermore, Facilities providing childbirth services in Tanzania are expected to have a multi-disciplinary Maternal Deaths Surveillance and Response committee to review all maternal deaths.14
Additionally, in accordance with the government’s national cost-sharing policy guidelines, children under the age of 5 years and pregnant women are eligible for exemptions from user charges for basic services.15
Data collection tool
The study used the WHO Service Availability and Readiness Assessment (SARA) tool to gather data on health facilities. This tool effectively addressed data gaps related to the availability and readiness of facilities to offer Maternal, Newborn and Child healthcare services. The WHO’s SARA tool is globally recognised and reliable for assessing health facilities and service delivery. For this study, the tool was adopted to focus specifically on maternal and newborn healthcare services, dividing into three main sections: (1) health facility information, (2) basic delivery services and (3) EmONC.
The data collected using the tool resolved around two primary domains: (1) availability, which assessed the physical presence of delivery services and (2) readiness, which measured the capacity to provide these services. Readiness was determined by evaluating the presence of key items, such as trained staff, guidelines, equipment, diagnostic tools and essential medicines and commodities. This adopted SARA tool served as a comprehensive and standardised approach to assess and improve maternal and newborn healthcare services.
Study variables
Dependent variables
The dependent variables were Service availability and Service readiness to provide BEmONC and CEmONC where service availability and service readiness were defined as follows:
Service availability refers to the physical presence of maternal and neonatal health services or the reach of the health facilities that can provide BEmONC and CEmONC services while Service readiness refers to the capacity of health facilities to provide or deliver BEmONC and CEmONC services.
BEmONC services availability was measured based on whether the following seven signal functions had ever been carried out by providers as part of their work within the facility at least once during the past 3 months: ‘parental administration of antibiotic’, ‘parental administration of oxytocin’, ‘parental administration of anticonvulsants’, ‘assisted vaginal delivery’, ‘manual removal of placenta’, ‘manual removal of retained products of conception’ and ‘neonatal resuscitation’.
BEmONC services readiness was assessed from all 14 dispensaries and 14 health centres and was measured based on the availability and functioning of supportive items categorised into three domains (groups): the first domain was staff training which had two indicators—the presence of guidelines and at least one staff who had received any formal or structured in-service training related to the services offered in the last 24 months preceding the assessment.
The second domain was diagnostic equipment which had 11 indicators, which were the presence of ‘emergency transport’, ‘sterilisation equipment’, ‘examination light’, ‘delivery pack’, ‘suction apparatus’, ‘manual vacuum extractor’, ‘vacuum aspirator or D&C kit’, ‘neonatal bag and mask’, ‘delivery bed’, ‘partograph’ and ‘gloves.’
The third domain was basic medicine and commodities which had 11 indicators containing essential medicines for delivery and newborn, which were, ‘injectable antibiotic’, ‘injectable uterotonic’, ‘injectable magnesium sulfate’, ‘injectable diazepam’, ‘intravenous fluids’, ‘skin disinfectant’, ‘antibiotic eye ointment’, ‘4% chlorhexidine’, ‘injectable gentamicin’, ‘injectable ceftriaxone’ and ‘amoxicillin suspension’.
The BEmONC service readiness was obtained as a composite score by adding the presence of each indicator, with equal weight given to each of the domains and each of the indicators within the domains. As the expected target is 100%, each domain accounted for 33.3% (100%/3) of the total score. The proportion of each indicator within the domain equalled 33.3% divided by the number of indicators in that domain.
The BEmONC service readiness score for each facility was calculated by adding the proportions. Given that the readiness score is a relative measurement, then facilities that scored 50% or more were considered to be ready or willing to provide BEmONC services than those who scored less than 50% in BEmONC readiness score.
CEmONC services availability was measured based on whether the nine signal functions of the CEmONC services (seven BEmONC functions plus caesarean section and blood transfusion) had ever been carried out by the providers.
CEmONC services readiness was assessed from all eight district hospitals and one regional hospital and was measured based on the availability and functioning of supportive items categorised into four domains (groups): the first domain was staff training which had four indicators—the presence of guidelines for CEmONC, staff trained in CEmONC, staff trained in surgery and staff trained in anaesthesia.
The second domain was equipment which had four indicators, that were the presence of ‘anaesthesia equipment’, ‘resuscitation table’, ‘incubator’, ‘and ‘oxygen’. The third domain was diagnostics which had two indicators, that were the presence of ‘blood typing’, and ‘cross-match testing’
The fourth domain was medicines and commodities which had five indicators containing essential medicines for delivery and newborn, that were, ‘Blood supply sufficiency’, ‘Blood supply safety’, ‘Lidocaine 5%’, ‘injectable epinephrine’ and ‘atropine’.
The CEmONC service readiness was obtained as a composite score by adding the presence of each indicator, with equal weight given to each of the domains and each of the indicators within the domains. As the expected target is 100%, each domain accounted for 25% (100%/4) of the total score. The proportion of each indicator within the domain was equal to 25% divided by the number of indicators in that domain. The CEmONC service readiness score for each facility was then calculated by adding the proportions. Given that the readiness score is a relative measurement, then facilities that scored 50% or more were considered to be ready or willing to provide CEmONC services than those who scored less than 50% in CEmONC readiness score.
Independent variables
All of our independent variables were categorical variables and they included: facility type categorised into dispensary, health centre, district hospital and regional hospital and for the purpose of comparison dispensaries were designated as the reference category; Facility Infrastructure which was the physical infrastructure and resources available at the facility including equipments and diagnostics, medicines and commodities, staff and guidelines, signal functions and training of healthcare workers to provide maternal and neonatal health services.
Data collection methods
Data collection involved observation and interviews. Health facility assessments focused on service availability, equipment functionality and the presence of supplies, medicines and commodities. Facility in-charges were interviewed to supplement data and involved the observation of all the items that were asked together with assessing if they are functional or not.
Trained medical students conducted the surveys, evaluating facilities’ readiness to provide Maternal Newborn and Child Health services in line with established guidelines.
Data analysis
Data analysis used the statistical package for social sciences and Microsoft Excel. Initially, data completeness was ensured, followed by coding. The coded data were entered into an electronic database. The analysis focused on service availability, examining the physical presence of services and service readiness, assessing the availability of essential inputs (tracer items) where tracer items referred to the availability and functioning of supportive items categorised into four domains which are (1) staff training, (2) equipments, (3) diagnostics and (4) medicine and commodities.
Descriptive statistics were computed, mean scores were calculated for each area and tracer items received equal weight. Results were summarised and presented through frequency distributions and charts, offering a comprehensive view of the status of maternal and neonatal healthcare services based on the components of service availability and readiness.
Patient and Public Involvement
Patients or public were not involved in this study
Results
General characteristics of the health facilities
The study included a total of 37 facilities of which 28 were from both dispensaries and health centres, 8 from district hospitals and 1 regional hospital. More than 40% of the surveyed facilities do not regularly review maternal or newborn deaths that occur within the facility. More than half of the facilities do not charge routine user fees for Antenatal Care (ANC) services, maternity services and child-immunisation services as summarised in table 1.
Table 1. General characteristics of the health facilities n=37.
| Variable | Frequency N (%) |
| Type of facility | |
| Dispensaries | 14 (37.8) |
| Health centres | 14 (37.8) |
| District hospitals | 8 (21.6) |
| Regional hospital | 1 (2.8) |
| Duty schedule for 24 hours | |
| Yes | 36 (97.3) |
| No | 1 (2.7) |
| Maternal/newborn deaths review | |
| Yes | 22 (59.5) |
| No | 15 (40.5) |
| Routine user fees for ANC services | |
| Yes | 4 (10.8) |
| No | 33 (89.2) |
| Routine user fees for maternity services | |
| Yes | 6 (18.9) |
| No | 31 (81.1) |
| Routine user fees for child-immunisation services | |
| Yes | 5 (13.5) |
| No | 32 (86.5) |
Availability of equipments and medicines/commodities for basic delivery services n= 37
Majority of the equipments and medicines for basic delivery services were available at all levels of health facilities; however, emergency transport, examination light, manual vacuum extractor and vacuum aspirator which are crucial in saving the lives of a pregnant woman and newborn babies were missing especially in dispensaries and health centres as summarised in online supplemental table 1.
Availability of BEmONC and CEmONC provided by health facilities
Majority of the signal functions were available in all level of health facilities with slight underreporting experienced in dispensaries as summarised in online supplemental table 2).
BEmONC service readiness score per indicator
Majority of the indicators which are necessary for provision of maternal and neonatal health services were available, especially in regional and district hospitals however there was underreporting of equipments and supplies, especially in dispensaries as shown in table 2.
Table 2. Indicators of readiness to provide basic emergency obstetric and newborn care services by facility-wise n=37.
| Indicators | Dispensaries (n=14)n (%) | Health centres (n=14) n (%) | District hospital (n=8) n (%) | Regional hospital (n=1) n (%) |
| Staff and guideline | ||||
| Presence of guidelines | 13 (92.9) | 13 (92.9) | 7 (87.5) | 1 (100) |
| Availability of trained staff in BEmONC at any career stage | 13 (92.9) | 10 (71.4) | 8 (100) | 1 (100) |
| Equipment and supplies | ||||
| Emergency transport | 2 (14.3) | 8 (57.1) | 8 (100) | 1 (100) |
| Sterilisation equipment | 10 (71.4) | 12 (85.7) | 8 (100) | 1 (100) |
| Examination light | 2 (14.3) | 11 (78.5) | 8 (100) | 1 (100) |
| Delivery pack | 13 (92.9) | 14 (100) | 8 (100) | 1 (100) |
| Suction apparatus | 11 (78.5) | 13 (92.9) | 8 (100) | 1 (100) |
| Manual vacuum extractor | 2 (14.3) | 4 (28.6) | 5 (62.5) | 1 (100) |
| Vacuum aspirator or Dilation and Curettage (D&C) kit | 3 (21.4) | 5 (35.7) | 6 (75.0) | 1 (100) |
| Neonatal bag and mask | 12 (85.7) | 14 (100) | 8 (100) | 1 (100) |
| Delivery bed | 10 (71.4) | 9 (64.3) | 3 (37.5) | 1 (100) |
| Partograph | 12 (85.7) | 14 (100) | 8 (100) | 1 (100) |
| Gloves | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
| Medicine and commoditiesEssential medicines for delivery | ||||
| Inj. antibiotic | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
| Inj. uterotonic | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
| Inj. magnesium sulphate | 13 (92.9) | 14 (100) | 8 (100) | 1 (100) |
| Inj. diazepam | 12 (85.7) | 14 (100) | 8 (100) | 1 (100) |
| Intravenous fluids | 13 (92.9) | 14 (100) | 8 (100) | 1 (100) |
| Skin disinfectant | 12 (85.7) | 14 (100) | 8 (100) | 1 (100) |
| Essential medicines for newborns | ||||
| Antibiotic eye ointment | 11 (78.5) | 13 (92.9) | 8 (100) | 1 (100) |
| 4% chlorhexidine | 2 (14.3) | 1 (7.1) | 2 (25.0) | 1 (100) |
| Inj. gentamicin | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
| Inj. ceftriaxone | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
| Amoxicillin suspension | 14 (100) | 14 (100) | 8 (100) | 1 (100) |
BEmONCbasic emergency obstetric and newborn care
Facility readiness to provide BEmONC services
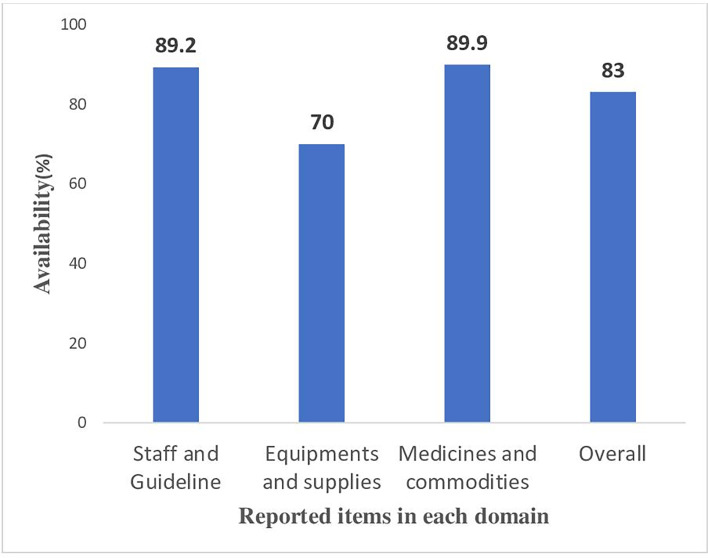
Figure 1 displays the readiness score for three domains and the comprehensive index reflecting the facility’s readiness to offer BEmONC. In each domain, the average readiness score surpassed 50%, as per WHO-SARA manual indicators, resulting in an overall mean readiness score of 83%. Additionally, almost all health facilities achieved an overall readiness score of at least 50%, indicating their readiness to deliver BEmONC services as illustrated in the readiness score per domain in figure 1 below.
Figure 1. Percentage score of the three domains of readiness to provide basic emergency obstetric and newborn care services.
CEmONC service readiness score
Availability of important supportive items for offering CEmONC services
Overall, the majority of the tracer items were available in both regional and district hospitals with overall readiness score of 98.87%; however, there was underreporting of staff trained in anaesthesia. Anaesthesia equipment and incubators in district hospitals as summarised in table 3.
Table 3. Indicators of readiness to provide comprehensive emergency obstetric and newborn care services n=9.
| Tracer item for CEmONC | Regional hospital(n=1)n (%) | District hospitals (n=8)n (%) |
| Staff and guideline | ||
| Trained staff in CEmONC at any career stage | 1 (100) | 8 (100) |
| Guideline CEmONC | 1 (100) | 8 (100) |
| Trained staff surgery | 1 (100) | 8 (100) |
| Trained staff anaesthesia | 1 (100) | 7 (87.5) |
| Equipments | ||
| Anaesthesia equipment | 1 (100) | 7 (87.5) |
| Resuscitation table | 1 (100) | 8 (100) |
| Incubator | 1 (100) | 7 (87.5) |
| Oxygen | 1 (100) | 8 (100) |
| Diagnostics | ||
| Blood typing | 1 (100) | 8 (100) |
| Cross match | 1 (100) | 8 (100) |
| Medicines and commodities | ||
| Blood supply sufficiency | 1 (100) | 8 (100) |
| Blood supply safety | 1 (100) | 8 (100) |
| Injectable epinephrine | 1 (100) | 8 (100) |
CEmONCcomprehensive emergency obstetric and newborn care
The level of staff who received training regarding maternal and neonatal health within the past 2 years
The level of staff who received training within the past 2 years was very low as only 29.8% of staff received training regarding BEmONC and CEmONC, 54.1% on ANC and 32.4% received training on Integrated Management of Neonatal and Childhood Illness (IMNCI) guidelines in the management of the sick neonate as indicated in file designated image.
Discussion
This study has found that, generally, all health facilities are moving in a positive direction in the provision of basic and comprehensive maternal and newborn care. However, a major finding has underscored the urgent need to address inadequate service readiness, particularly at lower level facilities such as dispensaries and health centres. Our study has pinpointed these facilities often lack the essential equipment and supplies required to deliver basic maternal and newborn care services effectively. A similar pattern emerged in district hospitals, where the provision of comprehensive maternal and newborn care services faces urgent challenges.
This study has shown that the availability of parenteral administration of anticonvulsants (magnesium sulphate), antibiotics as well as removal of retained products of conception are still challenging in the dispensaries. As a result, the provision of BEmONC services is compromised in these low-level facilities, which serve most of the population in the Kilimanjaro region. Similar findings have been reported in another low-resource setting in Papua New Guinea, where more than half of the participating lower level facilities could not provide the BEmONC services.16 It is crucial to address the deficiencies in BEmONC services, as these are critical components in managing significant perinatal conditions such as neonatal sepsis and eclampsia/pre-eclampsia, which are leading causes of maternal and neonatal death.17 Despite an improvement in BEmONC availability at low-level facilities from the year 2015 to 2020, as reported by the government, with readiness score increasing from 13% to 51% in dispensaries and from 28% to 76% in health centres, much emphasis is still needed at low-level health facilities to strengthen obstetric and newborn health service provision. This research found variable readiness for BEmONC provision among different types of facilities, as low-level facilities (dispensaries/health centres) continue to show alarmingly low scores. Strengthening the quality of services at these facilities becomes a pressing need.
Tracer items, which represent essential components of healthcare services, were assessed in the regional and district hospitals. We found that all tracer items were present in the regional hospital. However, some district hospitals needed more staff trained in anaesthesia, anaesthesia equipment and incubators. These findings are consistent with a study conducted in Unguja, where only one out of the five surveyed hospitals had anaesthesia equipment, and more incubators were needed in the district hospitals. The same study in Unguja also reported that caesarean sections were only performed in the regional hospital, with the lack of anaesthetists cited as the reason for non-performance in district hospitals.1 The shortage of anaesthesia staff and equipment may be attributed to a shortage of anaesthesia workforce at different levels of care in the country.18 Caesarean section is an essential component of CEmONC, and it is directly linked to the prevention of maternal and neonatal mortality by addressing direct obstetric complications.19 Adequate availability of trained staff and functioning anaesthesia equipment is necessary to ensure the provision of caesarean sections and manage obstetric emergencies effectively.
While service availability and readiness offer insights into the level of services provided, the actual quality of maternal and newborn care remains poorly understood. Thorough reviews of maternal and neonatal deaths can provide valuable information on the underlying causes, potential gaps in care and areas for improvement. Moreover, evaluating the training received by care providers within the past 6 months to 2 years can reveal their preparedness and competency in managing maternal and neonatal health issues effectively. On one hand, our study shows that most health facilities do not conduct regular maternal and newborn health reviews, a practice that is crucial for identifying and addressing gaps in care. As only 59.5% of all the facilities were reported to conduct the reviews per recommended guidelines, there is a clear need for improvement in this area. These findings are consistent with other studies whereby a study that assessed the conduct of maternal and perinatal death reviews in Uganda showed that only 34.8% of healthcare workers had ever participated in the death reviews. This may be attributed to health workers not being aware of the death review process, ineffective formation and training of death review committee members and inadequate support supervision.20 Also, blame culture may account for low death reviews where the reviews end up blaming health workers instead of trying to understand the cause and how to avoid it in the future.21 On the other hand, our findings show that training regarding maternal and newborn healthcare is still inadequate, a factor that significantly impacts the quality of care provided. As only 29.8%, 54.1% and 32.4% of all birth attendants in all 37 health facilities received training within the past 2 years regarding BEmONC and CEmONC, ANC and IMNCI respectively, there is a clear need for improvement in this area. These findings are consistent with other studies, which showed that only 32.1% of health workers had correct knowledge of MNC, 57.7% of major components of ANC, 39.4% of danger signs of pregnancy, and 54% of postnatal health problems22 and in another study done in Ethiopia, only 37.7% and 32.8% of Obstetric care providers were knowledgeable and had skills to manage the third stage of labour respectively.23 The low level of training might be attributed to less priority in healthcare budget allocation or misallocation of budget aimed at improving the knowledge and skills of birth attendants to tackle maternal and neonatal emergencies.
Strength and limitations
This study was done in all levels of the health facilities within the Kilimanjaro region from representatives of dispensaries and health facilities, all districts hospitals and a regional hospital. The sample size and scope limit the generalisability of the results for the dispensaries and health facilities as were confined to some public health facilities in the region, which may only be representative of some healthcare facilities in Tanzania. Although the study reports on the availability of BEmONC and CEmONC, the findings are limited by the lack of information on whether the reported items were fully functional or valid during the study period. Without this additional context, the findings on the availability of these critical services may not accurately reflect the actual capacity of the healthcare facilities surveyed. Despite these limitations, the study still provides valuable insights into the availability and readiness of maternal and neonatal health services in the Kilimanjaro region’s public health facilities. For instance, it highlights the need for improved infrastructure and equipment in some facilities. Future studies should employ longitudinal designs and expand the sample to improve generalisability and further enhance our understanding of these factors and their impact on maternal and neonatal health outcomes. The findings from this study remain relevant and valuable for policymakers and healthcare professionals seeking to improve maternal and newborn healthcare in the region.
Conclusion
The study identifies significant areas for improvement in the readiness of health facilities to provide maternal and newborn care services in the Kilimanjaro region. It highlights challenges such as the lack of critical delivery equipment in dispensaries and health centres, including emergency transport, examination lights and manual vacuum extractors. While BEmONC services generally showed high readiness, CEmONC services, particularly in district hospitals, lagged due to deficiencies in anaesthesia equipment and trained staff.
Recommendation
The Ministry of Health should take a prominent role in coordinating support from partners to enhance public health facility capacities. This includes expanding public–private partnerships, implementing maternal and child-health programmes, mobile health solutions and community emergency services. Addressing resource access gaps through streamlined procedures and rigorous training programmes for healthcare providers is crucial. Additionally, instituting a robust auditing mechanism for maternal and neonatal death reviews will ensure ongoing improvements in care quality. These strategic recommendations aim to improve healthcare accessibility, quality and safety for mothers and newborns in the Kilimanjaro region.
supplementary material
Acknowledgements
We would like to give our sincere gratitude to the director’s office at Kilimanjaro Clinical Research Institute and Kilimanjaro Christian Medical University College for the guidance, advice and support throughout the period of the study. We would also like to thank the Regional Administration secretary-Health Department, Regional nurse office and council-level authorities who granted us information regarding health facilities which serve a high number of pregnant women in the region.
Footnotes
Funding: This study was funded by the Kilimanjaro Clinical Research Institute (KCRI).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-086275).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by Kilimanjaro Christian Medical University College’s Ethical Review Committee (CRERC), certificate number UG 90/2022 Participants gave informed consent to participate in the study before taking part.
Collaborators: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Agathon Avelin Kimario, Email: agathonavelin19@gmail.com.
Ashraf Mahmoud, Email: ashyhms@gmail.com.
Jonaviva A Thomas, Email: anthonyjonaviva@gmail.com.
Benardine P Mallilah, Email: bmallilah@gmail.com.
Pendo S Mlay, Email: pendo.mlay@kcmuco.ac.tz.
Gaudensia Olomi, Email: olomigaudensia@yahoo.com.
Blandina Mmbaga, Email: b.mmbaga@kcri.ac.tz.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Bakar RR, Manongi RN, Mmbaga BT. Health Facility Capacity to Provide Maternal and Newborn Healthcare Services in Unguja. GJHS. 2019;11:120. doi: 10.5539/gjhs.v11n10p120. [DOI] [Google Scholar]
- 2.Targets of other sustainable development goals directly linked to health. [20-Oct-2023]. https://www.who.int/europe/about-us/our-work/sustainable-development-goals/targets-of-other-sustainable-development-goals-directly-linked-to-health Available. Accessed.
- 3.UNICEF, Organizzazione mondiale della sanita, Nazioni Unite. Population Fund, World Bank Group, Nazione Unite. Department of Economic and Social Affairs Trends in Maternal Mortality 2000 to 2020. 2000
- 4.UN Inter-agency Group for Child Mortality Estimation Levels & trends in child mortality: report. 2022
- 5.Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF . Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015-16. Dar Es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC; 2016. [Google Scholar]
- 6.Defar A, Getachew T, Taye G, et al. Quality antenatal care services delivery at health facilities of Ethiopia, assessment of the structure/input of care setting. BMC Health Serv Res. 2020;20:485. doi: 10.1186/s12913-020-05372-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andriantsimietry SH, Rakotomanga R, Rakotovao JP, et al. Service Availability and Readiness Assessment of Maternal, Newborn and Child Health Services at Public Health Facilities in Madagascar. Afr J Reprod Health. 2016;20:149–58. doi: 10.29063/ajrh2016/v20i3.19. [DOI] [PubMed] [Google Scholar]
- 8.Thobias B, Msengwa AS, Mbago MC. Spatial clustering of maternal health services utilization and its associated factors in Tanzania: Evidence from 2015/2016 Tanzania Demographic Health Survey. Tanz J Hlth Res. 2022;23 https://www.ajol.info/index.php/thrb/article/view/203945 Available. [Google Scholar]
- 9.Alemayehu M, Yakob B, Khuzwayo N. Quality of emergency obstetric and newborn care services in Wolaita Zone, Southern Ethiopia. BMC Pregnancy Childbirth. 2022;22:686. doi: 10.1186/s12884-022-05019-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muganyizi P. Availability, Coverage and Geographical Distribution of Emergency Obstetric and Neonatal Care Services in Tanzania Mainland. JGO. 2017;5:1. doi: 10.11648/j.jgo.20170501.11. [DOI] [Google Scholar]
- 11.Ministry of Health The national road map strategic plan to improve reproductive, maternal, newborn, child and adolescent health in tanzania - one plan ii. 2016
- 12.National bureau of statistics - 2022 population and housing census - administrative units population distribution and age and sex distribution reports. [20-Oct-2023]. https://www.nbs.go.tz/index.php/en/census-surveys/population-and-housing-census/852-2022-population-and-housing-census-administrative-units-population-distribution-and-age-sex-reports Available. Accessed.
- 13.Kwesigabo G, Mwangu MA, Kakoko DC, et al. Tanzania’s health system and workforce crisis. J Public Health Pol. 2012;33:S35–44. doi: 10.1057/jphp.2012.55. [DOI] [PubMed] [Google Scholar]
- 14.Said A, Pembe AB, Massawe S, et al. Maternal death surveillance and response in Tanzania: comprehensiveness of narrative summaries and action points from maternal death reviews. BMC Health Serv Res. 2021;21:52. doi: 10.1186/s12913-020-06036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mubyazi G, Massaga J, Kamugisha M, et al. User charges in public health facilities in Tanzania: effect on revenues, quality of services and people’s health-seeking behaviour for malaria illnesses in Korogwe district. Health Serv Manage Res. 2006;19:23–35. doi: 10.1258/095148406775322061. [DOI] [PubMed] [Google Scholar]
- 16.Hou X, Khan MM, Pulford J, et al. Readiness of health facilities to provide emergency obstetric care in Papua New Guinea: evidence from a cross-sectional survey. BMJ Open. 2022;12:e050150. doi: 10.1136/bmjopen-2021-050150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baharuddin M, Amelia D, Suhowatsky S, et al. Maternal death reviews: A retrospective case series of 90 hospital‐based maternal deaths in 11 hospitals in Indonesia. Intl J Gynecology & Obste. 2019;144:59–64. doi: 10.1002/ijgo.12736. [DOI] [PubMed] [Google Scholar]
- 18.Nyberger K, Jumbam DT, Dahm J, et al. The Situation of Safe Surgery and Anaesthesia in Tanzania: A Systematic Review. World J Surg. 2019;43:24–35. doi: 10.1007/s00268-018-4767-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cavallaro FL, Pembe AB, Campbell O, et al. Caesarean section provision and readiness in Tanzania: analysis of cross-sectional surveys of women and health facilities over time. BMJ Open. 2018;8:e024216. doi: 10.1136/bmjopen-2018-024216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agaro C, Beyeza-Kashesya J, Waiswa P, et al. The conduct of maternal and perinatal death reviews in Oyam District, Uganda: a descriptive cross-sectional study. BMC Womens Health. 2016;16:38. doi: 10.1186/s12905-016-0315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rousseva C, Kammath V, Tancred T, et al. Health workers’ views on audit in maternal and newborn healthcare in LMICs: a qualitative evidence synthesis. Trop Med Int Health. 2020;25:525–39. doi: 10.1111/tmi.13377. [DOI] [PubMed] [Google Scholar]
- 22.Acharya D, Paudel R, Gautam K, et al. Knowledge of Maternal and Newborn Care Among Primary Level Health Workers in Kapilvastu District of Nepal. Ann Med Health Sci Res. 2016;6:27–32. doi: 10.4103/2141-9248.180266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tenaw Z, Yohannes Z, Amano A. Obstetric care providers’ knowledge, practice and associated factors towards active management of third stage of labor in Sidama Zone, South Ethiopia. BMC Pregnancy Childbirth. 2017;17:292. doi: 10.1186/s12884-017-1480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]