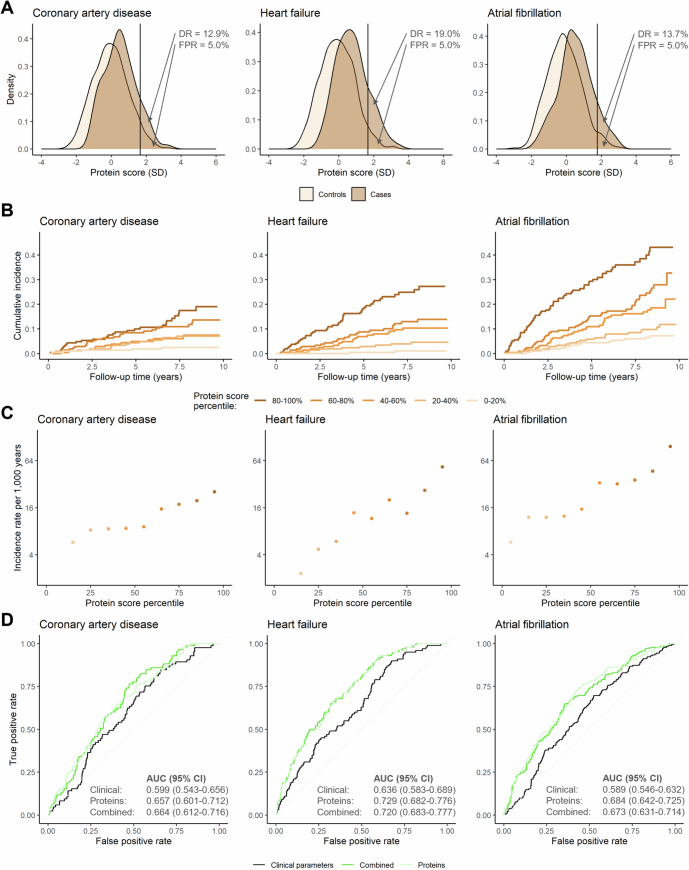
Extended Data Fig. 8. Risk (A–C) stratification and (D) prediction of incident coronary artery disease, heart failure, atrial fibrillation, and aortic stenosis by protein-based risk scores in the WHI-LLS.
The indicated plots depict (A) the distributions of protein-based risk scores in cases and controls; (B) the cumulative incidence of each outcome (calculated using the Kaplan–Meier method) by protein-based score quintiles; (C) incidence rate estimates according to protein-based score deciles on a logarithmically scaled Y axis; and (D) the accuracies of the clinical, proteomic, and combined risk scores in predicting the indicated outcomes (quantified using the area under the receiver-operating characteristic curve [AUC] with corresponding 95% confidence intervals [CIs]). For (A), the vertical lines indicate the protein-based risk score values corresponding to a false positive rate (FPR) of 5.0%; the detection rates (DRs) indicate the “exact” detection rates, calculated as the unadjusted proportions of cases with a positive test result at the corresponding protein-based risk score threshold. For (C), incidence rate estimates are not displayed if the incidence of the indicated outcome in a protein score percentile bin was zero. All analyses were performed in the Women’s Health Initiative Long Life Study (WHI-LLS; n = 1,083). During a median (interquartile range) follow-up of 8.3 (5.6-8.9) years, 85 participants in the WHI-LLS cohort experienced coronary artery disease events, 100 experienced heart failure, and 182 atrial fibrillation.