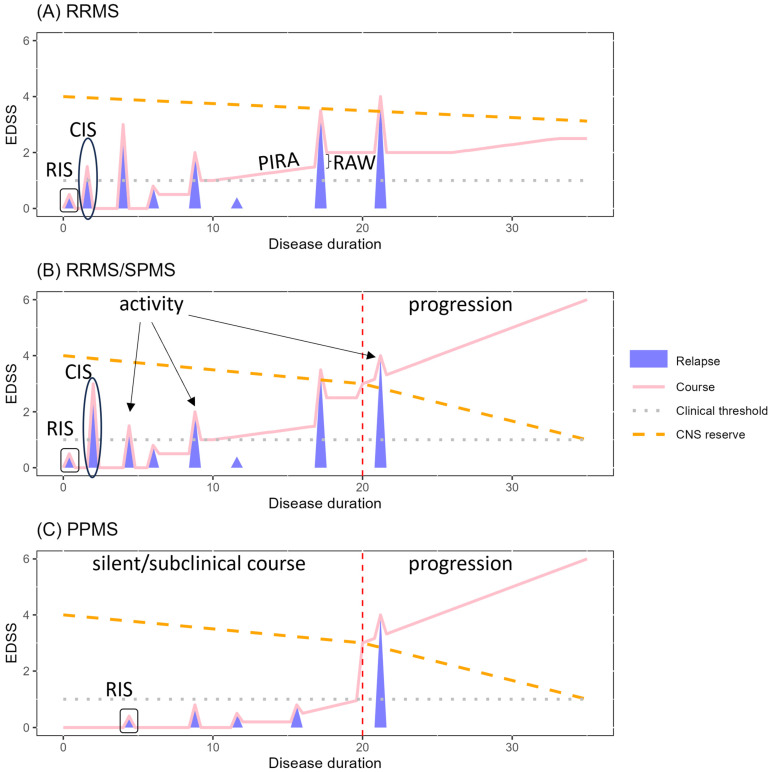
Figure 1.
Disease course and phenotypes. In these plots, the disease course (pink solid line) and disability measured by the Expanded Disability Status Scale (EDSS) score (y-axis) are depicted according to disease duration (x-axis) for (A) relapsing-remitting multiple sclerosis (RRMS), (B) secondary progressive MS (SPMS), and (C) primary progressive MS (PPMS). Disease activity and its progression determine the disease course. The relapsing-remitting course, occurring in most patients, is characterized by acute inflammatory demyelinating events (blue pyramids) resulting either in (i) new lesions on MRI below the clinical threshold (grey dotted line) and/or (ii) clinical relapses with (partially) reversible disability worsening. These alternate with periods of remission. Early in the disease, patients may recover completely, but with increasing disease duration and aging, relapse-associated worsening (RAW) might occur. Disability progression independent of relapse activity (PIRA) also occurs, sometimes already early in the disease. In progressive MS, patients suffer from progressive worsening, not necessarily linked to the occurrence of inflammatory disease activity. Secondary progressive MS can occur after a relapsing/remitting course, while 10–15% of patients develop a progressive phenotype from disease onset, so-called primary progressive MS. The neuroaxonal reserve (orange dashed line) decreases over time, due to aging, neuroinflammatory, and demyelinating processes. Once the compensatory mechanisms become insufficient, disability progresses. A clinically isolated syndrome (CIS) corresponds to the first clinical demyelinating event. In a radiologically isolated syndrome (RIS), white matter lesions compatible with MS are discovered on MRI but any history of related neurological symptoms is missing.