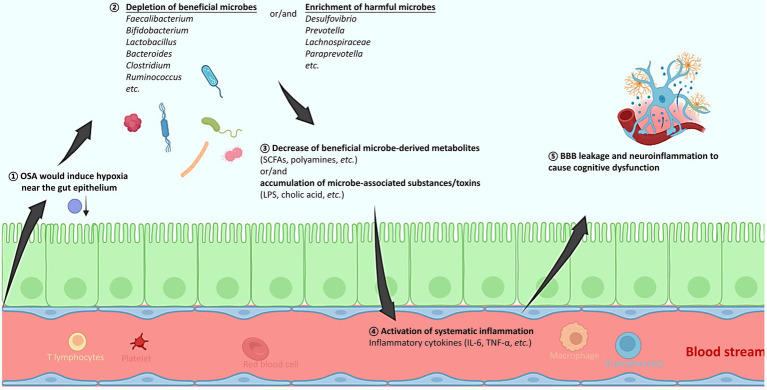
Figure 1.
A schematic diagram explaining how obstructive sleep apnea (OSA) would alter the gut microbiota, activate systematic inflammation, and consequently induce brain tissue injury and cognitive dysfunction. (1) The OSA-induced hypoxia might alter the oxygen concentration near the gut epithelium. (2) The depleted oxygen radiation thus favors the increased abundance of obligate and facultative anaerobes, resulting in the gut microbiota change that is mostly featured with an increased ratio of Firmicutes to Bacteroides (F/B). Specifically, producers of beneficial metabolites such as SCFAs and polyamines decrease, while microbial members with pathogenic potentials increase. (3) The gut microbiota composition change further leads to accumulation of microbial toxins, and/or decrease of a wide spectrum of beneficial metabolites. (4) The gut barrier function might be compromised, and levels of various inflammatory cytokines are elevated, resulting in a systematic inflammation. (5) The inflammatory cytokines can breach the BBB, activate microglial cells, cause neuroinflammation, and consequently result in cognitive deficits. OSA, obstructive sleep apnea; SCFAs, short chain fatty acids; LPS, lipopolysaccharide; IL-6, interleukin-6; TNF-α, tumor necrosis factor-α; BBB, blood brain barrier.