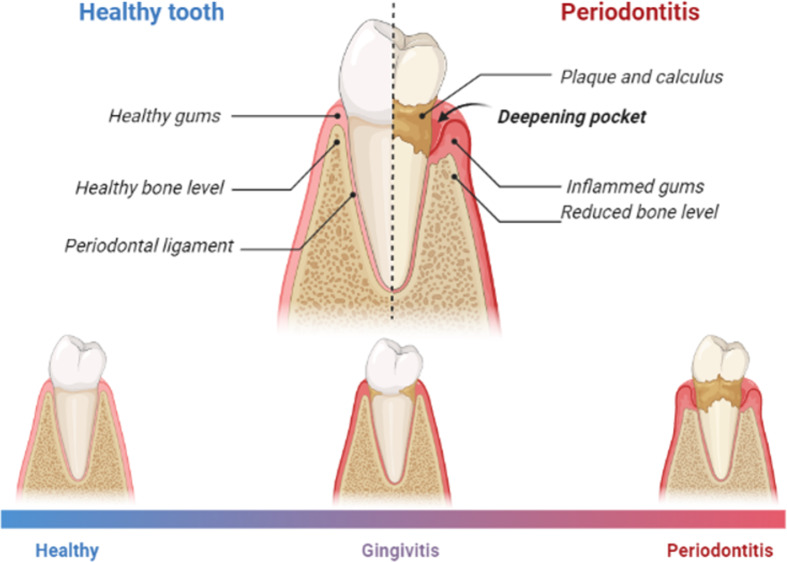
Figure 1.
A diagram showing differences between healthy teeth and teeth with gingivitis and periodontitis. Gingivitis is a reversible inflammation confined to the gingival tissues. The teeth in the oral cavity are supported by a ligament known as the periodontal ligament which attached the teeth to the gingiva and surrounding alveolar bone. The space between the tooth and the gingival tissues is known as the gingival sulcus, and this is where most of the dental plaque accumulates, triggering an inflammatory response. What differentiates gingivitis from periodontitis is that the latter is an irreversible destruction to the periodontal supporting tissues, including the alveolar bone, periodontal ligament, and cementum, which consequently results in tooth loss (Kinane et al., 2017, Tatakis and Kumar, 2005). As sources of inflammation, periodontal diseases contribute to the overall inflammatory burden experienced by individuals (Khoury et al., 2020). Initially, the gingival response to the biofilm is presented in the form of redness, edema, and bleeding. Oral polymorphonuclear neutrophils are then recruited to the sites of inflammation. In a healthy periodontium, oral neutrophils are usually found at the junctional epithelium and base of the sulcus (Khoury et al., 2020) to protect the periodontal tissues by providing a barrier between the junctional epithelium and pathogens within the dental plaque. However, as bacterial counts increase, so does the oral neutrophils count which enhance their activity (Khoury et al., 2020). Any deviation from PMN’s normal production, recruitment, function, or activity can lead to damage in periodontal tissues, and consequently tooth loss. (Prepared using Biorender.com).