FIGURE 4.
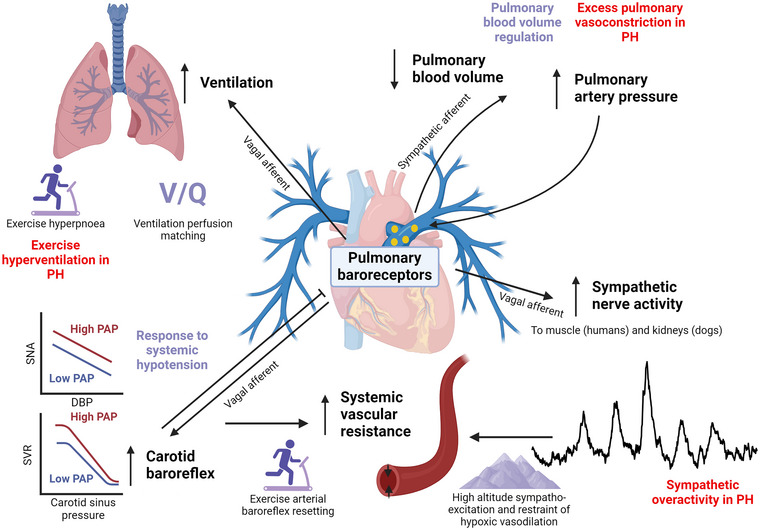
Summary of the known actions of pulmonary baroreceptors, their potential physiological function (purple) and significance in pulmonary hypertension (PH; red). Pulmonary baroreceptors increase their discharge in response to increases in pulmonary arterial pressure and distension. This produces a feed‐forward pulmo‐pulmonary reflex, probably mediated by sympathetic pulmonary arterial afferents, that increases pulmonary vasoconstriction and pressure and reduces pulmonary blood volume, which might have a role in regulating pulmonary blood volume but might also perpetuate pulmonary vasoconstriction in PH. Activation of the pulmonary baroreflex increases sympathetic nerve outflow (to skeletal muscle and kidneys) mediated by vagal pulmonary arterial afferents, which could be responsible, in part, for increased sympathetic activity at high altitude and for sympathetic overactivity in PH. Pulmonary baroreflex activation shifts the carotid baroreflex to higher blood pressure and sympathetic outflow (SNA), probably mediated by vagal afferents, which contributes to an increase in systemic vascular resistance (SVR) and arterial pressure. Conversely, carotid baroreflex activation inhibits the pulmonary baroreflex such that sympathetic outflow and systemic blood pressures are lower at a given pulmonary artery pressure. These interactions between pulmonary and systemic baroreflexes could have a role in cardiorespiratory exercise responses, responses to systemic hypotension and restraint of peripheral hypoxic vasodilatation at high altitudes. Finally, pulmonary baroreflex activation stimulates phrenic nerve activity and increases respiratory drive mediated by vagal afferents, which might have a role in the generation of exercise hyperpnoea and could optimize ventilation‐to‐perfusion matching () by increasing ventilation when pulmonary blood flow increases distension of pulmonary arteries. Created in BioRender. Plunkett, M. (2024) BioRender.com/i27k675.
