Abstract
A 36-year-old female with a remote history of spontaneous pneumothorax treated with talc pleurodesis presented with a large anterior mediastinal synovial sarcoma. The mass developed within a residual asymptomatic mediastinal space during a 2-year period. The patient underwent complete surgical resection and adjuvant chemoradiotherapy, which provide the best chance for survival. Although the cause of these tumors is unclear, this report may further delineate the natural history of this rare pathologic process.
Synovial sarcomas are rare soft tissue tumors that arise from immature mesenchymal stem cells and make up 5% to 10% of all soft tissue tumors.1 About 80% of these tumors arise in the extremities of young adults, with only a small subset developing in the thoracic cavity. A review of the National Cancer Database identified 101 cases of mediastinal synovial sarcoma (MSS) in the United States between 2004 and 2012.2 The natural history of mediastinal synovial tumors is poorly understood with nonspecific treatment guidelines often extrapolated from the treatment of synovial sarcomas in the extremities. Here we report a case of MSS in a patient who previously underwent talc pleurodesis for nonresolving spontaneous pneumothorax 14 years earlier.
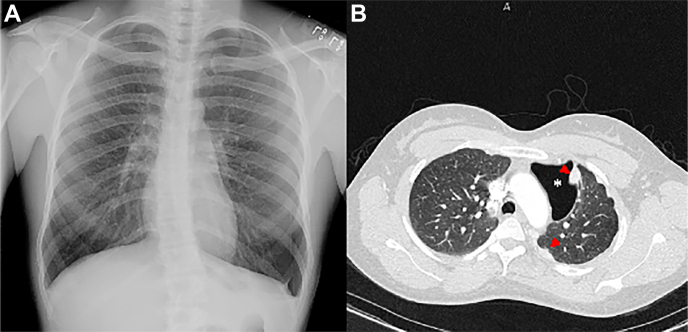
The patient, a 36-year-old woman, previously presented with a nonresolving spontaneous left pneumothorax that was treated with thoracoscopic talc pleurodesis (4-5 g). No pleuropulmonary masses or blebs were visualized (Figure 1A). Eight years later, an asymptomatic space was identified within the anterior mediastinum on a chest radiograph. A subsequent computed tomography scan performed 4 years later during pregnancy revealed a similar space in the anterior mediastinum with multiple nodular pleural plaques consistent with prior talc treatment (Figure 1B).
Figure 1.
(A) Chest radiograph at initial presentation demonstrating a moderate-size pneumothorax. (B) Computed tomography scan 12 years after initial presentation demonstrating large loculated anterior pneumothorax (asterisk) and multiple pleural nodules (arrowheads).
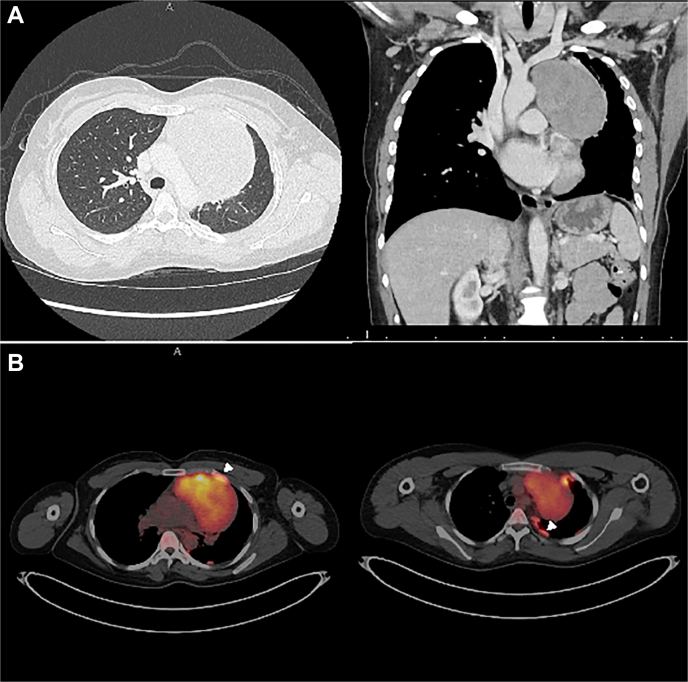
Fourteen years after her initial episode, the patient presented to the emergency department with a 2-month history of chest pain and episodes of syncope. Imaging showed a large anterior mediastinal mass with high uptake and multiple pleural plaques occupying the previously identified space (Figure 2). Biopsy confirmed MSS, and the patient received 1 dose of neoadjuvant chemotherapy before undergoing resection through a left trap-door incision (ifosfamide-mesna, doxorubicin). The tumor was adherent to the pericardium, requiring resection of the left phrenic nerve. Multiple pleural plaques were present and identified as benign talcomas on frozen section.
Figure 2.
(A) Computed tomography scan of cross-section and coronal views of mediastinal mass. (B) Positron emission tomography/computed tomography scan demonstrating uptake avidity within mediastinal mass (standard uptake value, 4.4). Arrowheads demonstrate uptake avidity within pleural plaques.
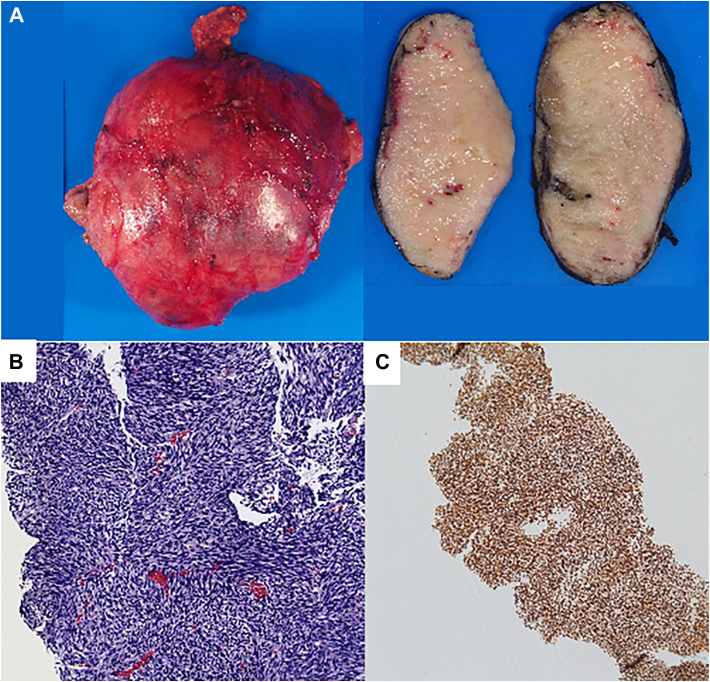
Histopathologic evaluation confirmed a 12.5 × 11.3 × 5.3-cm stage ypT3N0 synovial sarcoma (Figure 3) with monomorphic spindle cell, high nucleus-cytoplasmic ratio, and positive SS18-SSX1 fusion, which confirmed the diagnosis of synovial sarcoma. The medial resection margin was positive. Both a surgical site infection and a clostridium difficile colitis infection developed and were treated. At 8 weeks postoperatively, the patient started adjuvant radiation (total of 59.4 Gy) for local disease control and subsequently 6 cycles of adjuvant chemotherapy (mesna, doxorubicin, and ifosfamide). She remains clinically well 6 months postoperatively.
Figure 3.
(A) Macroscopic view of the well-circumscribed mediastinal mass. (B) Hematoxylin and eosin staining demonstrating dense fascicles of monomorphic spindle cells. (C) Positive TLE1 immunohistochemical staining consistent with synovial sarcoma.
Comment
This report describes a synovial sarcoma developing within the contours of a chronic anterior mediastinal space 14 years after talc pleurodesis (Figure 1, Figure 2). Serial imaging in our patient demonstrated that the mass developed during a 2-year period, shedding light on the natural history of this rare entity. Synovial sarcomas developing within the thoracic cavity are often reported in the literature as either MSS or pleuropulmonary synovial sarcoma (PPSS).3 The distinction between these entities is vague with significant overlap. PPSS often refers to tumors that originate in or directly invade the pulmonary parenchyma, whereas MSS originates in and is isolated to the mediastinum. MSS has only recently been described, and the first reports were published within the past 3 decades. Patients often present between the ages of 30 and 38 years, and tumors are on average between 11 and 13 cm. More than 95% of synovial sarcomas are characterized by a pathognomonic oncogenic fusion of the SS18-SSX proteins, leading to overexpression and downregulation of several oncogenes implicated in cancer development.1 Although prognosis remains poor, it is largely dependent on size as well as on local and metastatic spread. Curative treatment is dependent on complete surgical excision as well as on adjuvant chemoradiotherapy.1,2 Unlike their analogues in the extremities, which have been reported to have an approximately 2-year delay between onset and diagnosis, the natural history of MSS is not well understood as patients often present with nonspecific symptoms attributable to mass effect.
Some thoracic synovial sarcomas, primarily PPSS, can manifest as spontaneous pneumothorax. Previous case reports identified patients with underlying occult PPSS in the blebectomy specimen after treatment of nonresolving spontaneous pneumothorax.4,5 Petrosyan and Bergeron6 described a patient who underwent a talc pleurodesis and blebectomy and was diagnosed 2 years later with a large ipsilateral PPSS requiring pneumonectomy. Our patient was treated with talc pleurodesis, and no underlying mass or emphysematous changes were found during the initial operation. Given these findings and the aggressive nature of these tumors, it is unlikely that an underlying malignant neoplasm led to the development of an MSS 14 years earlier. Nevertheless, we do not know whether our patient’s tumor originated from the visceral or parietal pleura or the mediastinum.
Synovial sarcomas are known mimickers of sarcomatoid mesothelioma and can often be distinguished only by genetic testing.7 Whereas asbestos exposure is a known cause of mesothelioma, the role of talcum powder as a possible carcinogen has been a historical concern. Talc has been used as a pleurodesis agent since the 1930s and was once suspected of causing cervical and ovarian cancers. However, it was later discovered that asbestos contamination in feminine hygiene products was the likely culprit. Today, large prospective studies have demonstrated no causal relationship between talcum powder and cancer, and medical-grade asbestos-free talc is now widely used as an effective pleurodesis agent.8 There are no data to suggest talc as a risk factor for synovial sarcoma.7
In conclusion, this case highlights the rare nature of these tumors and may further elucidate the development and treatment of synovial sarcoma within chronically treated spaces. After multimodal therapy with surgical resection and chemoradiotherapy, our patient remains well and disease free. Although the pathogenesis of MSS remains unclear and more research is needed to further identify the underlying causes, this report may further elucidate the natural history of this rare entity.
Acknowledgments
Funding Sources
The authors have no funding sources to disclose.
Disclosures
The authors have no conflicts of interest to disclose.
Patient Consent
Obtained.
References
- 1.Stacchiotti S., Van Tine B.A. Synovial sarcoma: current concepts and future perspectives. J Clin Oncol. 2018;36:180–187. doi: 10.1200/JCO.2017.75.1941. [DOI] [PubMed] [Google Scholar]
- 2.Engelhardt K.E., DeCamp M.M., Yang A.D., Bilimoria K.Y., Odell D.D. Treatment approaches and outcomes for primary mediastinal sarcoma: analysis of 976 patients. Ann Thorac Surg. 2018;106:333–339. doi: 10.1016/j.athoracsur.2018.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lan T., Chen H., Xiong B., et al. Primary pleuropulmonary and mediastinal synovial sarcoma: a clinicopathologic and molecular study of 26 genetically confirmed cases in the largest institution of southwest China. Diagn Pathol. 2016;11:62. doi: 10.1186/s13000-016-0513-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel P.B., Sankrith M., Cedeno-Rodriguez A. Pediatric pleuropulmonary synovial sarcoma: a case report in a recurrent spontaneous pneumothorax. Respir Med Case Rep. 2022;36 doi: 10.1016/j.rmcr.2022.101622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cummings N.M., Desai S., Thway K., et al. Cystic primary pulmonary synovial sarcoma presenting as recurrent pneumothorax: report of 4 cases. Am J Surg Pathol. 2010;34:1176–1179. doi: 10.1097/PAS.0b013e3181e85c87. [DOI] [PubMed] [Google Scholar]
- 6.Petrosyan A., Bergeron P. Extensive surgical treatment of primary pulmonary synovial sarcoma after recurrent pneumothorax. Ann Thorac Surg. 2015;100:1893–1895. doi: 10.1016/j.athoracsur.2014.12.092. [DOI] [PubMed] [Google Scholar]
- 7.Kerger B.D., James R.C., Galbraith D.A. Tumors that mimic asbestos-related mesothelioma: time to consider a genetics-based tumor registry? Front Genet. 2014;5:151. doi: 10.3389/fgene.2014.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Brien K.M., Tworoger S.S., Harris H.R., et al. Association of powder use in the genital area with risk of ovarian cancer. JAMA. 2020;323:49–59. doi: 10.1001/jama.2019.20079. [DOI] [PMC free article] [PubMed] [Google Scholar]