Abstract
Central memory CD8+ T cells (TCM) and effector memory CD8+ T cells (TEM) are found in humans and mice; however, their relative contributions to host immunity have only recently been examined in vivo. Further, the ability of TCM to treat an established tumor or infection has yet to be evaluated. To address the therapeutic potential of different tumor-reactive CD8+ T cell memory subsets, we used an established model for the in vitro generation of TCM and TEM by using IL-15 and IL-2, respectively. Adoptively transferred TCM exhibited a potent in vivo recall response when combined with tumor-antigen vaccination and exogenous IL-2, leading to the eradication of large established tumors. By contrast, TEM were far less effective on a per-cell basis. Microarray analysis revealed that the signature of highly in vivo effective antitumor T cells included the overexpression of genes responsible for trafficking to secondary lymphoid tissues. This gene expression profile correctly predicted the in vitro and in vivo lymphoid-homing attributes of tumor-reactive T cells. Furthermore, we found that homing to secondary lymphoid tissue is required for optimal tumor treatment. Our findings indicated that highly in vivo effective antitumor T cells were those that initially targeted secondary lymphoid tissue, rather than tumor sites, as had previously been postulated. Thus, tumor-reactive CD8+ T cell populations with the phenotypic and functional attributes of TCM may be superior to TEM/effector T cells for adoptive immunotherapies using concomitant tumor-antigen vaccination.
Keywords: IL-2, IL-15, homing, immunotherapy, vaccine
Adoptive cancer immunotherapy, the infusion of tumor-reactive T cells to patients, represents a promising approach for the treatment of advanced metastatic disease (1, 2). To date, cell types with effector T cell (TEFF) and effector memory CD8+ T cell (TEM) phenotype and function have been the cells targeted for transfer because of their strong lytic capacity and release of high levels of IFN-γ (3, 4). Although transfer of polyclonal tumor-reactive TEFF can cause an objective response rate approaching 50% (5), there are reasons to believe that transfer of cells with memory properties, including a heightened recall response and the ability to undergo self-renewal, may be superior mediators of an antitumor response (6, 7).
The T cell memory compartment can be subdivided into two populations, central memory CD8+ T cells (TCM) and TEM, on the basis of phenotypic markers, functional attributes, and migratory properties (7). CD62L and CCR7, two surface molecules necessary for cellular extravasation in high endothelial venules, are constitutively expressed by TCM, whereas these markers are significantly down-regulated on TEM. TCM have been shown to be superior to TEM in conferring protective immunity against viral or bacterial challenge (8, 9). However, the extent to which these results can be generalized has been questioned (10), and the potential of TCM to treat an established infection or cancer has not been evaluated.
To assess the in vivo role of different CD8+ T cell memory subsets, we used an established in vitro culture system by using IL-15 and IL-2 to generate TCM and TEM, respectively (8, 11–13). To generate tumor-reactive CD8+ T cells, we used cells from pmel-1 T cell receptor transgenic mice. Pmel-1 mice have CD8+ T cells that have specificity for a Db-restricted epitope corresponding to amino acid positions 25–33 of the nonmutated self/tumor antigen (Ag) gp100 (14). The two cell subtypes were verified by using global analysis of gene expression as well as phenotypic and functional characteristics. We found that adoptive cell transfer (ACT) of self/tumor-reactive CD8+ TCM was a superior mediator of tumor treatment compared with TEM.
Materials and Methods
Mice and Tumor Lines. Pmel-1 T cell receptor transgenic mice expressing CD8+ T cells with specificity for a Db-restricted epitope from the nonmutated self/tumor Ag gp10025–33 (14) were crossed with C57BL/6-thy1.1 transgenic and C57BL/6-Sell-/- mice (both from The Jackson Laboratory) to derive pmel-thy1.1 (deposited at The Jackson Laboratory, www.jax.org) and pmel-CD62L-/- (pmel CD62L knockout) mice (26), respectively. Female C57BL/6 and B6.129S2-Ltatm1Dch/J (both from The Jackson Laboratory) and β2-microglobulin (β2M)-deficient (β2M-/-) mice (Taconic Farms) were used as recipients in ACT experiments. B16 (H-2b), a spontaneous gp100+ murine melanoma, has been described (14). Experiments were conducted with the approval of the National Cancer Institute Animal Use and Care Committee.
TCM and TEM Generation and Adoptive Immunotherapy. Pmel-1 splenocytes were isolated and cultured in the presence of 1 μM human gp10025–33 (hgp10025–33) and complete medium containing 10 ng/ml of either recombinant human IL-2 (Chiron) to generate pmel TEM or recombinant human IL-15 (PeproTech, Rocky Hill, NJ) to generate pmel TCM (12). Mice (n = 5) were injected s.c. with 2–5 × 105 B16-F10 melanoma cells. Nine days later, mice were treated with i.v. ACT of pmel TCM or TEM. Where specified, transient lymphopenia was induced by sublethal irradiation (500 cGy) of tumor-bearing mice on the day of treatment. Vaccination was achieved with 2 × 107 plaqueforming units of a recombinant fowlpox virus encoding hgp100 (rFPhgp100) as described (Therion Biologics, Cambridge, MA) (14). Recombinant human IL-2 was administered by i.p. injection twice daily at 36 μg per dose for a total of six doses. Murine bone marrow (BM)-derived dendritic cells (DCs) were generated as described (15). The products of the perpendicular diameters (mean ± SEM) of tumors for tumor growth curves were measured in a blinded fashion with calipers. All experiments were repeated at least twice with similar results.
Microarray and Flow Cytometric Analysis of TCM and TEM. Pmel TCM and TEM were isolated to a purity of >95% by using a no-touch, negative selection CD8-enrichment column (Miltenyl Biotech, Auburn, CA). RNeasy column (Qiagen, Germantown, MD)-purified RNA was indirectly labeled with a single round of linear amplification with Amino Allyl MessageAmp reagents (Ambion, Austin, TX). Labeled samples were combined and hybridized overnight to 22,000-gene long-oligo arrays supplied by the National Cancer Institute (Frederick, MD). Data image files were obtained with a GenePix 4000B scanner (Axon Instruments, Union City, CA) and imported into genespring 6.2 software (Silicon Genetics, Redwood City, CA).
Ex Vivo Analysis of Adoptively Transferred Cells. All antibodies were purchased from BD Pharmingen except anti-human granzyme B-phycoerythrin (GB11) (Caltag, Burlingame, CA). FACS-calibur flow cytometer and cellquest software (BD BioSciences, Franklin Lakes, NJ) were used to analyze cells. Adoptively transferred cells in inguinal, axillary, and mesenteric lymph nodes (LNs) were analyzed by cytofluorometry for carboxyf luorescein diacetate succinimidyl ester (CFSE), thy1.1, and CD8. For immunohistochemical staining, inguinal LNs were snap-frozen, stored at -80°C, then sectioned at 7-μm cuts by using cryostat. Sections were Fc-blocked before staining with 10 μg/ml purified anti-PNAd (BD Pharmingen) followed by Cy5-conjugated secondary antibody (Caltag). Sections were mounted with a ProLong Antifade Kit (Molecular Probes) and allowed to stand at room temperature overnight. Images were obtained on a Nikon Eclipse confocal laser-scanning microscope (Bio-Rad). In vitro proliferation of pmel TEM and TCM was evaluated by labeling cells with 1 μM CFSE (Molecular Probes) and restimulating with 1 μM hgp10025–33-pulsed irradiated splenocytes in complete medium containing 2 ng/ml of recombinant human IL-2.
In Vitro Rolling Assay. Rolling of pmel TEM, pmel TCM, and CD8-enriched naïve cells was determined on 35-mm cell suspension plates (430588) (Corning) coated with GlyCAM-1 (a gift from S. D. Rosen, University of California, San Francisco), E-selectin (R & D Systems), or 1% BSA in PBS, held overnight at 4°C, and blocked with 1% BSA for 1 h at 4°C. Calcein-acetomethyl-labeled (Molecular Probes) T cells were injected at 1.5 dynes per cm2 into a parallel plate flow chamber (Glycotech, Gaithersburg, MD). Cells were digitally photographed (≈1 image per s) in four to six random fields (each field = 1.18 mm2) with excitation at 488 nm and emission at 513 nm, and nonmoving and moving cells were differentiated with the iplab software program (Scanalytics, Fairfax, VA) and compared by using the Student t test.
Results
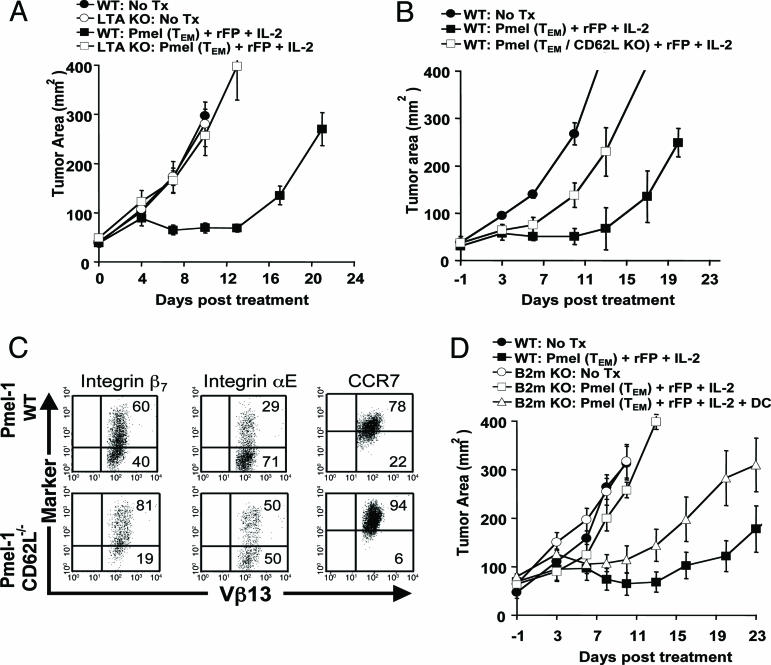
Trafficking to 2° Lymphoid Tissues Is Required for Optimal Antitumor Treatment. Altered peptide ligand (14, 15) vaccine-encoded tumor Ag presentation by professional Ag-presenting cells promotes optimal antitumor immunity (16). We therefore hypothesized that trafficking of adoptively transferred cells to 2° lymphoid organs could lead to an enhanced in vivo antitumor response. To evaluate the lymphoid trafficking requirements of adoptively transferred pmel cells, we compared the tripartite treatment regimen of cells, rFPhgp100 vaccination, and exogenous IL-2 in tumor-bearing C57BL/6 (WT) and lymphotoxin-α-/- (LTα-/-) mice. LTα-/- mice lack peripheral lymphoid structures, including LNs and mucosal Peyer's patches, and possess a disorganized splenic white pulp (17). To provide a treatment window, we intentionally transferred a noncurative dose (1 × 106) of pmel TEM. There was no statistical difference in tumor growth between untreated WT and LTα-/- mice (P = 0.8550) (Fig. 1A). As previously shown by our group, the combination of pmel TEM, vaccination, and IL-2 caused a pronounced delay in tumor growth in WT mice compared with untreated controls (P < 0.0001) (12, 14, 18). By contrast, the antitumor effect was completely abrogated in LTα-/- mice. There was no statistical difference in tumor growth between untreated LTα-/- mice and LTα-/- mice that received cells, vaccine, and IL-2 (P = 0.6200). Thus, 2° LNs were required in the tumor-bearing host for optimal tumor treatment.
Fig. 1.
Trafficking of tumor-reactive CD8+ T cells to 2° lymphoid tissues is required for antitumor treatment. (A)WT or L Tα-/- mice bearing 9-day s.c. B16 tumors were left untreated as controls (• and ○, respectively) or received 1 × 106 pmel TEM, rFPhgp 100 vaccination, and exogenous IL-2 (▪ and □, respectively). (B) CD62L expression by adoptively transferred tumor-reactive CD8+ T cells is required for optimal antitumor treatment. WT mice bearing 9-day s.c. B16 melanoma tumors were treated with nothing (•), pmel-CD62L-/- cells (□), or age-matched pmel-CD62L+/+ cells (▪) in combination with rFPhgp100 and exogenous IL-2. (C) Redundancy of lymphoid-homing molecules. Splenocytes from pmel-CD62L-/- or age-matched pmel-CD62L+/+ controls were stimulated with 1 μM hgp 10025–33 peptide and cultured under TEM conditions. Cells were cytofluorometrically analyzed on day 6 for the expression of integrin αE, integrin β7, and CCR7. Numbers represent the percentage of gated cells in each quadrant after gating on propidium iodide-negative and CD8+ lymphocytes. (D) Tumor treatment fails in β2M-/- hosts, but can be rescued by cotransfer of BM-derived DCs. WT or β2M-/- mice bearing 9-day B16 tumors were left untreated as controls (• and ○, respectively) or received 1 × 106 TEM pmel, rFPhgp100, and exogenous IL-2 (▪ and □, respectively) ± cotransfer of mature BM-derived DCs (▴).
To determine the influence of L-selectin (CD62L), a critical mediator of lymphocyte homing to 2° LNs (19), we adoptively transferred TEM from pmel-CD62L-/- or age-matched pmel-CD62L+/+ controls in combination with vaccine and IL-2 into tumor-bearing WT mice. Although treatment with either TEM pmel-CD62L-/- or pmel-CD62L+/+ cells resulted in delayed tumor growth compared with untreated controls (P = 0.0018 and < 0.001, respectively), pmel-CD62L+/+ cells conferred superior treatment efficacy compared with pmel-CD62L-/- cells (P = 0.0091) (Fig. 1B). Thus, CD62L was functionally important for antitumor T cell function in vivo. Phenotypic analysis revealed, however, that the overexpression of other LN-homing receptors might partially compensate for the lack of CD62L, including integrin β7, integrin αE, and CCR7 (Fig. 1C).
To test whether homing of adoptively transferred pmel-1 cells to LNs facilitated their interaction with resident professional Ag-presenting cells expressing the vaccine-encoded hgp10025–33, we compared the treatment efficacy of our tripartite regimen in tumor-bearing WT versus β2M-/- mice. Tumor growth was identical in untreated WT and β2M-/- controls (P = 0.963) (Fig. 1D). The tripartite regimen of cells, vaccine, and IL-2 was effective at delaying tumor growth in WT mice (P = 0.0034) but was not effective in the same experiment in mice incapable of presenting MHC class I-restricted Ags (untreated vs. treated β2M-/- mice P > 0.05). This lack of treatment effect could be partially rescued by the cotransfer of β2M-intact mature BM-derived DCs (P = 0.009 vs. no treatment). No rescue was observed when DCs were generated from β2M-/- mice (data not shown). Thus, we determined that trafficking of adoptively transferred tumor-reactive CD8+ T cells to organized 2° lymphoid tissues was necessary for optimal in vivo antitumor efficacy in a combined immunotherapy treatment regimen that includes tumor-Ag vaccination.
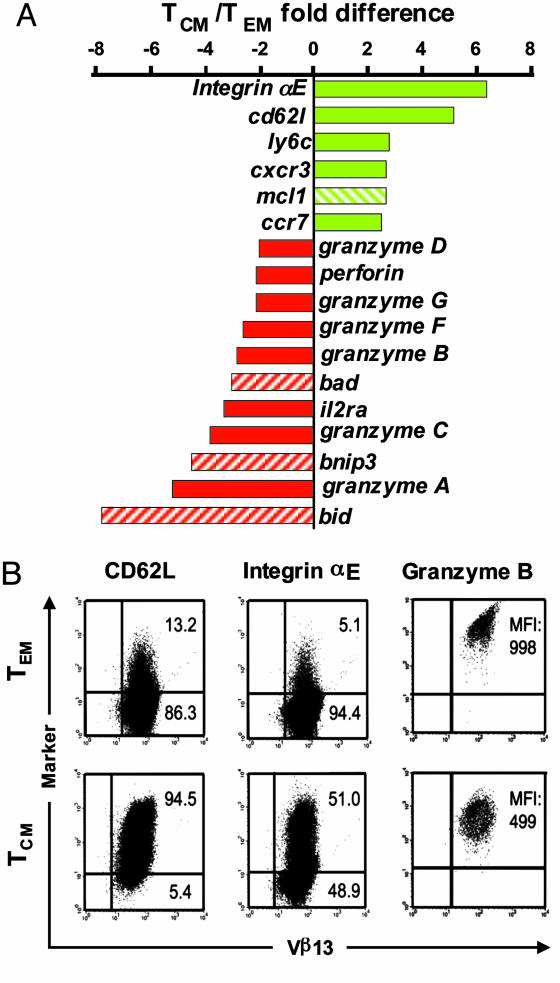
Gene Expression Profiling of CD8+ TCM vs. TEM. Because trafficking to 2° lymphoid tissues by adoptively transferred pmel cells facilitated their in vivo antitumor efficacy, we sought to create T cells with enhanced LN-homing attributes. Naïve, peptide-stimulated CD8+ T cells expanded in the presence of IL-15 give rise to in vitro differentiated TCM, whereas IL-2 caused the expansion of TEM that lost the expression of the LN-homing markers CD62L and CCR7 (8, 12, 13). To more fully characterize the attributes of these two cell populations, we performed microarray analysis (GEO accession nos. GSE2578 and GSM49518, www.ncbi.nlm.nih.gov/geo). A total of 476 of the 22,000 genes sampled were differentially expressed between pmel TCM and TEM. Remarkably, genes associated with homing to 2° lymphoid tissues, including integrin aE, cd62l, ly6c, cxcr3, and ccr7, were among those RNAs overexpressed by pmel TCM compared with TEM (Fig. 2A). Additionally, mcl1, an antiapoptosis molecule implicated in the maintenance of mature T lymphocytes, was also up-regulated by TCM (20). By contrast, genes associated with effector functions (granzyme A, B, C, D, F, G, H, and perforin) and proapoptotic signaling (Bid, Bnip3, and Bad) were among the most highly overexpressed in TEM (Fig. 2 A). Microarray results for CD62L, integrin αE, and intracellular granzyme B on pmel TCM and TEM were validated by cytofluorometry (Fig. 2B). Consistent with previously published FACS results, CD62L expression was notably higher in pmel TCM than in TEM (12). Integrins αE (Fig. 2B) and β7 (data not shown) were two additional lymphoid-homing molecules that were overexpressed on pmel TCM. Conversely, pmel TEM exhibited a higher level of granzyme B expression compared with pmel TCM (mean fluorescence intensity = 998 and 499, respectively). These data indicated that some of the most pronounced gene and protein expression differences between pmel TCM and TEM relate to the capacity to home to LNs and the acquisition of effector functions, respectively.
Fig. 2.
Gene expression profiling and FACS analysis of self/tumor-reactive CD8+ TCM vs. TEM. (A) A selected summary of microarray results. Shown in green are the genes involved in trafficking to 2° lymphoid organs; the hatched green bar indicates a gene (mcl1) that has antiapoptotic activity; shown in red are genes involved in effector functions; and hatched red bars indicate proapoptotic genes. (B) Cytofluorometric validation of microarray results of pmel TCM and TEM. Surface expression of CD62L and integrin αE are shown with the percentages of CD8+ lymphocytes in each quadrant or the mean fluorescence intensity (MFI) for intracellular granzyme B.
In Vitro and in Vivo LN-Homing Attributes of Tumor Ag-Specific TCM and TEM. To determine whether the gene and protein expression profiling results of pmel TCM and TEM were reflected in functional difference in tissue homing behavior, we evaluated the in vitro rolling of pmel TCM and TEM under physiologic shear flow conditions. We used substrates coated with glycam-1, a ligand for CD62L expressed in the high endothelial venules of peripheral LNs (19). Neither population of cells rolled on substrates coated with BSA, an irrelevant protein control (Fig. 3A). Both pmel TCM and CD8-enriched naïve pmel-1 cells, a lymphocyte population with optimal LN-homing attributes, rolled on glycam-1, whereas pmel TEM did not (P < 0.01) (Fig. 3 A and B). TEM reportedly display a characteristic pattern of surface chemokine and adhesion molecules required for homing to inflamed peripheral tissues (7). To test this capacity, we assayed rolling of in vitro-generated pmel TCM and TEM on substrates coated with E-selectin, a leukocyte adhesion molecule expressed on endothelial cells at inflammatory sites. Both cell types rolled on this substrate (Fig. 3A); however, a greater number of pmel TEM compared with TCM was found on E-selectin (P < 0.05). Therefore, pmel TEM possessed in vitro properties consistent with an enhanced propensity to traffic to inflamed peripheral tissues, whereas pmel TCM displayed enhanced LN-homing attributes.
Fig. 3.
LN-homing attributes of tumor Ag-specific CD8+ TCM vs. TEM. (A and B) Pmel TCM but not TEM roll efficiently on substrates coated with glycam-1, a ligand for CD62L. Calcein-acetomethyl-labeled pmel TCM, TEM, or CD8-enriched naïve cells were injected at 1.5 dynes per cm2 into a parallel plate flow chamber in which the bottom plate was coated with glycam-1, E-selectin, or BSA. After 4 min, rolling cells were photographed (four to six random fields per condition) and counted in a blinded fashion (mean ± SD). (C and D) In vivo LN homing of pmel TCM vs. TEM. CFSE-labeled, pmel-thy1.1 TCM and TEM were adoptively transferred into separate Thy1.2 WT mice, and LNs were extracted 24 h later. (C) Cryostat sections of inguinal LNs 24 h after ACT of 4 × 106 CFSE-labeled (green) pmel TCM (Lower) or TEM (Upper). High endothelial venules were identified by staining for PNAd followed by Cy5-conjugated secondary antibody (blue). (D) Cytofluorometric analysis for CFSE+CD8+ cells from homogenized peripheral LNs and Peyer's patches of recipient mice 24 h after ACT.
We next investigated the in vivo LN-homing properties of these two cell populations. We adoptively transferred CFSE-labeled pmel-thy1.1 TCM and TEM into thy1.2 C57BL/6 hosts. Twenty-four hours after ACT, we extracted peripheral LNs of recipient mice for immunohistochemical staining and FACS analysis. Grossly, immunohistochemical staining of inguinal LNs 24 h after ACT revealed a pronounced accumulation of adoptively transferred CFSE-labeled cells in animals that received pmel TCM, but not TEM (Fig. 3C). Cytofluorometric analyses of peripheral LNs was performed to quantitate these results, and multiple independent experiments confirmed that there was between 20 and 40 times the number of CFSE+CD8+ cells present in lymphoid tissues in animals that received pmel TCM compared with TEM (Fig. 3D). These results were not caused by differential CFSE dilution by pmel TEM because similar results were obtained by analysis for CD8+ Thy1.1+ cells (data not shown). These data demonstrated that gene expression profiling of pmel-1 cells expanded under TCM and TEM conditions accurately depicted the in vitro and in vivo LN-homing attributes of these two populations of tumor-reactive CD8+ T cells.
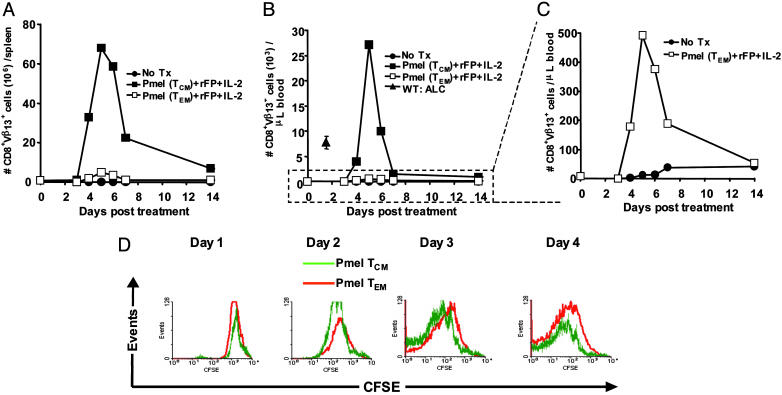
Enhanced in Vivo Recall Response and Tumor Treatment of TCM Compared with TEM. To determine the functionality of TCM and TEM in vivo, we adoptively transferred in vitro-differentiated pmel subsets into sublethally irradiated tumor-bearing WT mice in combination with vaccine and IL-2. The in vivo recall response of these two cell populations (as assessed by the enumeration of the absolute numbers of adoptively transferred pmel-1 cells in the spleens and blood of treated animals) revealed that there was a marked expansion of adoptively transferred TCM and TEM, peaking in both groups ≈5 days after transfer (Fig. 4A). Importantly, the magnitude of the response in the spleens of mice that received TCM was strikingly greater, peaking at levels four to 14 times higher than TEM in individual experiments. These results were not caused simply by the differential accumulation of TCM in the spleen because an analogous proliferation pattern was also observed in the blood, a nonlymphoid tissue (Fig. 4 B and C). Indeed, animals that received TCM experienced a true tumor-reactive CD8+ T cell lymphocytosis that was more than three times the absolute lymphocyte count of WT mice, a phenomenon not observed with TEM. The in vivo results were not caused merely by intrinsic differences in proliferative capacity of TCM over TEM, because there was a similar rate of CFSE dilution in these two cell populations in an ex vivo assay (Fig. 4D).
Fig. 4.
Enhanced in vivo recall response of tumor-Ag-specific CD8+ TCM over TEM. (A–C) Sublethally irradiated WT mice bearing 9-day established B16 tumors were left untreated as controls (•) or received the tripartite combination of rFPhgp100, exogenous IL-2, and 1 × 106 pmel TCM (▪)orTEM (□). Absolute numbers of adoptively transferred pmel-1 cells (identified by CD8+Vβ13+ lymphocytes) were enumerated in the spleens or blood of treated animals as a function of time. Each data point represents the average of at least two mice per group. For comparison, the mean absolute lymphocyte count (± SEM) of five nonirradiated tumor-bearing WT mice is shown (▴). (D) Comparison of the intrinsic proliferative capacity of restimulated pmel TCM vs. TEM. Pmel-thy1.1 cells expanded under TCM (light lines) or TEM (bold lines) conditions were CFSE-labeled, then restimulated with irradiated WT splenocytes pulsed with hgp10025–33 peptide in complete media containing IL-2. CFSE dilution was determined by daily FACS analysis after gating on CD8+thy1.1+ lymphocytes.
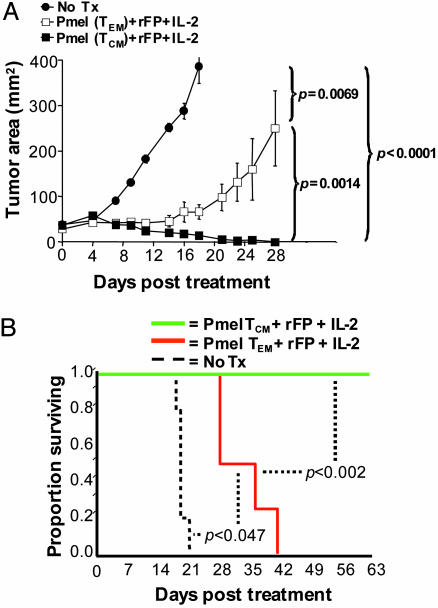
Pronounced lymphocytosis in melanoma patients treated with ACT after lymphodepletion has been correlated with antitumor efficacy (5). To determine whether the lymphocytosis observed in mice treated with TCM correlated with the antitumor effect, we treated sublethally irradiated mice bearing 9-day established B16 melanoma with ACT at a dose of pmel cells (1 × 106) previously established to be noncurative when TEM are used in combination with vaccine and IL-2. As previously shown, the suboptimal tripartite regimen using pmel TEM caused a pronounced delay without cures in tumor growth compared with untreated controls (P = 0.0069) (Fig. 5A). Treatment with TCM delayed tumor growth significantly compared with both untreated controls (P < 0.0001) and TEM-treated mice (P = 0.0014). In addition, a TCM-based regimen caused improved survival (P < 0.002) (Fig. 5B). Thus, ACT of a TCM population, in combination with tumor-Ag vaccination and exogenous IL-2, produced a more robust and therapeutically significant in vivo recall response compared with TEM.
Fig. 5.
Tumor-reactive CD8+ TCM are superior to TEM in the treatment of B16 melanoma. (A) Sublethally irradiated (5 Gy) WT mice bearing 9-day B16 tumors were left untreated as controls (•) or received rFPhgp100 vaccination, exogenous IL-2, and either pmel TCM (▪) or TEM (□). (B) Enhanced tumor regression in mice receiving pmel TCM correlated with statistically prolonged animal survival, compared with mice receiving TEM.
Discussion
Recent human trials for the adoptive immunotherapy of cancer have demonstrated a statistical correlation between the persistence of transferred tumor-reactive T cells and the therapeutic response that could objectively be achieved in ≈50% of the patients treated by using cells with TEM or effector T cell phenotype (21). Although preliminary work using viral Ags has suggested that TCM are superior mediators of a recall response to Ag challenge (8, 9), some have recently called these findings into question (10). In the present studies, we evaluated the role of TEM and TCM populations as mediators of an immune response to an established disease. We found that Ag-specific TCM mounted a heightened in vivo recall response compared with TEM, consistent with other reports (9, 22). Importantly, this enhanced response by TCM was associated with the complete eradication of a large, established B16 melanoma. As seen in other models, TEM can generate a 2° response but the relative efficiency of this response was less than that of TCM on a per-cell basis (9, 22).
Although TCM and TEM have been subdivided on the basis of their relative expression of lymphoid-homing molecules (7, 11), these two populations also possess other unique attributes. For example, TEM have been shown to develop effector functions more rapidly than TCM (7, 8). By contrast, TCM are able to release significant amounts of helper cytokines, such as IL-2 (7, 9, 12). In our own analysis of the differences between TCM and TEM by using oligo microarrays, we found that expression of genes associated with lymphoid homing were among the most highly overexpressed by TCM. The critical importance of homing to 2° LNs by adoptively transferred tumor-reactive T cells was established by experiments in which tumor therapy was completely abrogated in host mice with absent peripheral lymphoid tissues and a disrupted splenic structure. Further evidence that trafficking to LNs is required was provided by using tumor-reactive CD8+ T cells genetically deficient in CD62L.
T cell homing to 2° LNs was required to facilitate interaction with virally infected BM-derived Ag-presenting cells, as evidenced by the absence of tumor treatment in β2M-/- hosts and their rescue by cotransfer of WT BM-derived DCs. It is likely that the enhanced in vivo proliferative response of TCM was the result of increased access to vaccine-encoded Ag-expression in 2° LNs as both TCM and TEM exhibited similar intrinsic proliferative responses when Ag levels were normalized in vitro. These results indicated that, in addition to prevention, TCM can be a superior mediator of a therapeutic response, and this effect highly depended on the cells' homing to lymphoid tissues.
The approach of targeting T cell trafficking to LNs provides an alternative to attempts to cause the initial trafficking of adoptively transferred immune cells to tumors directly (23). These efforts have included the insertion of genes encoding chemokine receptors into lymphocytes to enhance their recruitment to tumor sites (24) and the genetic modification of the tumor microenvironment itself through the forced expression of LIGHT, a tumor necrosis factor superfamily member used to enhance the recruitment, retention, and activation of T cells (25). Thus, the alternative and perhaps complementary approach described here is the use of concomitant tumor-Ag vaccination that induces a massive clonal expansion and subsequent infiltration of numerous tissues by antitumor T cells (18) that obviates the requirement for immediate and specific targeting of the tumor site.
These results have implications for the design of human adoptive immunotherapy trials. In most currently used protocols, the cells generated for ACT acquire effector T cell/TEM phenotypic and functional attributes before transfer (4). Our data suggest that ACT of these populations may be suboptimal; although response rates approaching 50% can now be obtained with the transfer of very large numbers (up to 1 × 1011) of ex vivo-expanded T cells (5). The transfer of a more efficient antitumor TCM population might increase the proliferation and persistence of cells upon adoptive transfer in vivo. Our findings may have significant implications for the selection and the generation of optimal antitumor T cells for ACT in cancer patients. The generation of TCM may be accomplished by altering duration and nature of T cell culture conditions in human clinical trials.
Acknowledgments
C.A.K. dedicates this manuscript to Grandma Anne Anderson and her personal battle with cancer. We thank D. Surman, P. J. Spiess, Z. Yu, and Y. Lou for technical assistance.
Author contributions: C.A.K., L.G., S.T.H., S.A.R., T.A.W., and N.P.R. designed research; C.A.K., L.G., P.T.-P., K.K., A.R.C., S.E.F., D.C.P., and P.A.A. performed research; P.T.-P., K.K., A.R.C., and S.T.H. contributed new reagents/analytic tools; C.A.K., L.G., P.T.-P., K.K., A.R.C., S.T.H., S.A.R., T.A.W., and N.P.R. analyzed data; and C.A.K., L.G., S.T.H., S.A.R., T.A.W., and N.P.R. wrote the paper.
Abbreviations: Ag, antigen; hgp100, human gp100; rFPhgp100, recombinant fowlpox virus encoding hgp100; TEM, effector memory CD8+ T cells; TCM, central memory CD8+ T cells; LN, lymph node; ACT, adoptive cell transfer; DC, dendritic cell; CFSE, carboxyfluorescein diacetate succinimidyl ester; LTα, lymphotoxin-α; β2M, β2-microglobulin; BM, bone marrow.
References
- 1.Dudley, M. E. & Rosenberg, S. A. (2003) Nat. Rev. Cancer 3, 666-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klebanoff, C. A., Khong, H. T., Antony, P. A., Palmer, D. C. & Restifo, N. P. (2005) Trends Immunol. 26, 111-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yee, C., Thompson, J. A., Byrd, D., Riddell, S. R., Roche, P., Celis, E. & Greenberg, P. D. (2002) Proc. Natl. Acad. Sci. USA 99, 16168-16173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powell, D. J., Jr., Dudley, M. E., Robbins, P. F. & Rosenberg, S. A. (2005) Blood 105, 241-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dudley, M. E., Wunderlich, J. R., Yang, J. C., Sherry, R. M., Topalian, S. L., Restifo, N. P., Royal, R. E., Kammula, U., White, D. E., Mavroukakis, S. A., et al. (2005) J. Clin. Oncol. 23, 2346-2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaech, S. M., Wherry, E. J. & Ahmed, R. (2002) Nat. Rev. Immunol. 2, 251-262. [DOI] [PubMed] [Google Scholar]
- 7.Sallusto, F., Geginat, J. & Lanzavecchia, A. (2004) Annu. Rev. Immunol. 22, 745-763. [DOI] [PubMed] [Google Scholar]
- 8.Manjunath, N., Shankar, P., Wan, J., Weninger, W., Crowley, M. A., Hieshima, K., Springer, T. A., Fan, X., Shen, H., Lieberman, J., et al. (2001) J. Clin. Invest. 108, 871-878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wherry, E. J., Teichgraber, V., Becker, T. C., Masopust, D., Kaech, S. M., Antia, R., Von Andrian, U. H. & Ahmed, R. (2003) Nat. Immunol. 4, 225-234. [DOI] [PubMed] [Google Scholar]
- 10.Roberts, A. D. & Woodland, D. L. (2004) J. Immunol. 172, 6533-6537. [DOI] [PubMed] [Google Scholar]
- 11.Weninger, W., Crowley, M. A., Manjunath, N. & Von Andrian, U. H. (2001) J. Exp. Med. 194, 953-966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klebanoff, C. A., Finkelstein, S. E., Surman, D. R., Lichtman, M. K., Gattinoni, L., Theoret, M. R., Grewal, N., Spiess, P. J., Antony, P. A., Palmer, D. C., et al. (2004) Proc. Natl. Acad. Sci. USA 101, 1969-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyahara, N., Swanson, B. J., Takeda, K., Taube, C., Miyahara, S., Kodama, T., Dakhama, A., Ott, V. L. & Gelfand, E. W. (2004) Nat. Med. 10, 865-869. [DOI] [PubMed] [Google Scholar]
- 14.Overwijk, W. W., Theoret, M. R., Finkelstein, S. E., Surman, D. R., de Jong, L. A., Vyth-Dreese, F. A., Dellemijn, T. A., Antony, P. A., Spiess, P. J., Palmer, D. C., et al. (2003) J. Exp. Med. 198, 569-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lou, Y., Wang, G., Lizee, G., Kim, G. J., Finkelstein, S. E., Feng, C., Restifo, N. P. & Hwu, P. (2004) Cancer Res. 64, 6783-6790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bronte, V., Carroll, M. W., Goletz, T. J., Wang, M., Overwijk, W. W., Marincola, F., Rosenberg, S. A., Moss, B. & Restifo, N. P. (1997) Proc. Natl. Acad. Sci. USA 94, 3183-3188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Togni, P., Goellner, J., Ruddle, N. H., Streeter, P. R., Fick, A., Mariathasan, S., Smith, S. C., Carlson, R., Shornick, L. P., Strauss-Schoenberger, J., et al. (1994) Science 264, 703-707. [DOI] [PubMed] [Google Scholar]
- 18.Palmer, D. C., Balasubramaniam, S., Hanada, K., Wrzesinski, C., Yu, Z., Farid, S., Theoret, M. R., Hwang, L. N., Klebanoff, C. A., Gattinoni, L., et al. (2004) J. Immunol. 173, 7209-7216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosen, S. D. (2004) Annu. Rev. Immunol. 22, 129-156. [DOI] [PubMed] [Google Scholar]
- 20.Opferman, J. T., Letai, A., Beard, C., Sorcinelli, M. D., Ong, C. C. & Korsmeyer, S. J. (2003) Nature 426, 671-676. [DOI] [PubMed] [Google Scholar]
- 21.Robbins, P. F., Dudley, M. E., Wunderlich, J., El Gamil, M., Li, Y. F., Zhou, J., Huang, J., Powell, D. J., Jr. & Rosenberg, S. A. (2004) J. Immunol. 173, 7125-7130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bouneaud, C., Garcia, Z., Kourilsky, P. & Pannetier, C. (2005) J. Exp. Med. 201, 579-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho, W. Y., Blattman, J. N., Dossett, M. L., Yee, C. & Greenberg, P. D. (2003) Cancer Cell 3, 431-437. [DOI] [PubMed] [Google Scholar]
- 24.Kershaw, M. H., Wang, G., Westwood, J. A., Pachynski, R. K., Tiffany, H. L., Marincola, F. M., Wang, E., Young, H. A., Murphy, P. M. & Hwu, P. (2002) Hum. Gene Ther. 13, 1971-1980. [DOI] [PubMed] [Google Scholar]
- 25.Yu, P., Lee, Y., Liu, W., Chin, R. K., Wang, J., Wang, Y., Schietinger, A., Philip, M., Schreiber, H. & Fu, Y. X. (2004) Nat. Immunol. 5, 141-149. [DOI] [PubMed] [Google Scholar]
- 26.Gattinoni, L., Klebanoff, C. A., Palmer, D. C., Wrzesinski, C., Kerstann, K., Yu, Z., Finkelstein, S. E., Theoret, M. R., Rosenberg, S. A. & Restifo, N. P. (2005) J. Clin. Invest. 115, 1616-1626. [DOI] [PMC free article] [PubMed] [Google Scholar]