Abstract
Men who have sex with men are a target group for HIV prevention and control. HIV testing is part of a broader combination prevention strategy. This study aimed to analyze the predictors for adherence to HIV infection testing among Brazilian men who have sex with men. A cross-sectional study was conducted with 1438 participants, online selected for convenience in all regions of Brazil. Binary logistic regression analysis was used to identify independent predictors of HIV testing in the study population. Adherence to the HIV test was high (80.1%). Had condomless anal intercourse in the last 12 months (Adjusted Odds Ratio [AOR]: 1,659; 95% Confidence Interval [CI]:1,12 − 2,43; p = 0,010), knew one place to seek HIV testing (AOR 6,158 [IC95%: 4,27 − 8,86]; p < 0,001), Received counselling on HIV testing by a health professional (AOR 3,389 [IC95%: 2,28 − 5,02]; p < 0,001), Have been diagnosed with STI (AOR 2,266 [IC95%: 1,41 − 3,62]; p < 0,001) and Knew someone living with HIV (AOR 1,86 [IC95%: 1,29 − 2,67]; p < 0,001) were independently associated with higher chances of HIV testing.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-21018-2.
Keywords: HIV infections, HIV Testing, Sexual and gender minorities, Primary prevention
Background
The epidemic of Human Immunodeficiency Virus (HIV) infection still being a global public health problem that affects different groups unequally. It presents a growing trend among Men who have Sex with Men (MSM), a group that accounts for 17% of new cases in the world [1]. The disproportionate prevalence of concentrated cases is also observed in Brazil, rising from 12.1% in 2009 [2] to 18.4% in 2018 [3].
Despite the global trend of increasing cases of HIV among MSM [4], the risk of infection may be even greater in low- and middle-income countries due to the stigma, and social inequalities that impair accessing the prevention services [5–7]. Thus, integrating MSM into prevention care results in epidemiological, virological, immunological, and clinical benefits. Affordable HIV testing is core to timely diagnosis and treatment, improving outcomes and reducing transmission [8].
Increasing screening indicators, awareness and adherence to HIV testing among sexually active MSM are urgent needs and have a leading role in the epidemiological control of the infection. So, it should be performed annually for asymptomatic people and every three or six months for those higher-risk cases [9]. In Brazil, public health actions implemented by the Unified Health System (in Portuguese: Sistema Único de Saúde - SUS) have improved the coverage and frequency of testing: expansion of testing services and the free provision of rapid, serological and self-testing for HIV [10]. Substantial advances in the HIV testing cascade are evident. Worldwide, there has been an increase in demand for HIV testing services. In 2022, 89% of people living with HIV knew their HIV status [9]. HIV testing is the core strategy for prevention, linking positive cases to supportive services and environments, reducing transmission and ongoing morbidity for all key populations.
Despite advances, there still exists a considerable global proportion of people who have never been tested or are unaware of their serological status, increasing the chances of immunological deterioration and secondary transmission. These facts constitute pivotal gaps for achieving the 95-95-95 target proposed by the Joint United Nations Program on HIV/AIDS (UNAIDS), which advocates the epidemiological control of HIV until 2030 [11].
So, understanding the barriers or facilitators to HIV testing among MSM is essential to increase awareness of risky practices, access to prevention centres, adherence and testing frequency [12]. The current evidence related to indicators and factors associated with testing is still limited, requiring further investigations for supporting interventions favourable to awareness, adherence and access to prevention services. Based on it, we proposed this investigation to evaluate the predictors for adherence to HIV testing among Brazilian MSM.
Method
Study design, participants and data collection
This is an analytical cross-sectional study conducted with MSM from all regions of Brazil. To participate, MSM had to be 18 years old or more, identify as a man, have Brazilian nationality, have access to the internet, and have had at least one sexual relationship with another man in their lifetime. The exclusion criterion was not answering the question about HIV testing (“Have you ever been tested for HIV in your life?”).
Data were collected from April to May 2020 through an online questionnaire created and stored on the SurveyMonkey platform. Different methods were used to recruit participants. Initially, the questionnaire link was shared on social media platforms such as Instagram, Facebook, Twitter, WhatsApp groups, and Telegram. It contained text information along with the link, requesting that it be shared with other MSM, thus reaching MSM who were not in the virtual environments where the link was shared. The questionnaire link was also shared on dating apps for MSM. All regions of Brazil were reached through this recruitment strategy.
Convenience sampling was used to collect data online. A total of 1830 participants accessed the questionnaire. After filtering the database with those who met the criteria and completed the survey, the final sample was composed of 1438 MSM.
Questionnaire and variables
The survey included gathering sociodemographic information, sexual behaviour, and HIV prevention data. All the participants accessed and signed the ethical consent form by the link before starting the questionnaire. The questionnaire was developed by the authors for this study and is available in Appendix 1.
Having been tested for HIV at least one time in life was considered as the outcome. It was evaluated dichotomously (yes/no) through the question “Have you ever been tested for HIV?”.
The independent variables were the following: age group; gender; sexual orientation; years of study; skin color (self-declared); work situation; income; marital status; fixed sexual partnership; alcohol use; tobacco use; Brazil region; Number of sexual partners in the last three months; Number of sexual partners in the last year; age of onset of sexual life; More frequent sexual practice; Anal intercourse without a condom in the last year; Condom use in all sexual relations; Use of male condom in the last sexual intercourse; use of lubricating gel during sexual intercourse; knows a place to perform an HIV test; received advice from a health professional about HIV testing; received advice from a friend about HIV testing; received free male condom in the last 12 months; read information on the internet about HIV prevention in the last 12 months; read information in printed material about prevention in the last 12 months; had a diagnosis of Sexually Transmitted Infection (STI); know person living with HIV; being a sex worker and use of HIV Pre-Exposure Prophylaxis (PrEP).
Statistical analysis
Data were analyzed using binary logistic regression to determine the impact of independent variables on HIV testing adherence. Independent variables with a statistical significance of p < 0.2 were included in the regression model using the enter method. The Pearson’s chi-square test was used in bivariate analysis. Odds ratios, Crude Odds Ratio (COR) and Adjusted Odds Ratio (AOR) were calculated with a 95% Confidence Interval and a significance level of 5% (α = 0.05) using Jamovi software (version 2.3) [13].
Ethics approval and consent to participate
This study followed all the guidelines of the Declaration of Helsinki. It was approved by the Ethics in Research Committee of the Ribeirão Preto College of Nursing, following the recommendations of the National Health Council Resolution 466/12. Consent to participate in the study was given in electronic signature by all participants before data collection. They signed the Informed Consent Form. It is a document with specific information about the research containing the main objectives, possible risks and benefits, and information about confidentiality, privacy, and information about the research coordinators. The anonymity of all participants was preserved.
Results
A total of 1438 (100%) people participated in this study. The majority of them had white skin colour (656; 45.6%), were in the range of 18 to 28 years old (915; 63.6%), had more than 11 years of education (1156; 80.4%), and self-reported as gays (1190; 82.8%). A high proportion of them had already been tested for HIV (1152; 80.1%). Having benn tested for HIV was associated with the age group (p < 0.001), years of education (p < 0.001), work situation (p < 0.001), monthly family income (p < 0.001), marital status (p = 0.005), gender (p < 0.001) and sexual orientation (p < 0.001).
Regarding sex behaviour, Table 1 shows there was a considerable association between having a previous HIV testing and the most frequent sexual practice (p < 0.001), having condomless anal intercourse in the last 12 months (p < 0.001), knowing a place to get an HIV test (p < 0.001), and have received information about HIV test from a health professional (< 0.001) or from a friend (p < 0.001).
Table 1.
Characterization of men who have sex with men and the association of independent variables with HIV testing (n = 1438). Brazil, 2020
| Variables | HIV test | ||||
|---|---|---|---|---|---|
| Yes 1152 (80,1) |
No 286 (19,9) |
Total 1438 (100) |
P* | ||
| Age group | |||||
| 18–28 | 667 (72,9) | 248(27,1) | 915 (100) | < 0,001 | |
| 29–39 | 406 (93,1) | 30 (6,9) | 436 (100) | ||
| 40 + | 79 (90,8) | 8 (9,2) | 87 (100) | ||
| Gender | |||||
| Cisgender Man | 1031 (81,6) | 232 (18,4) | 1263 (100) | < 0,001 | |
| Transgender man | 100 (68,0) | 47 (32,0) | 147 (100) | ||
| Intergender | 21 (75,0) | 7 (25,0) | 28 (100) | ||
| Sexual orientation | |||||
| Gay | 983 (82,6) | 207 (17,4) | 1190 (100) | < 0,001 | |
| Bisexual | 117 (68,4) | 54 (31,9) | 171 (100) | ||
| Other | 52 (67,5) | 25 (32,5) | 77 (100) | ||
| Schooling | |||||
| < 11 years | 162 (57,4) | 120 (42,6) | 282 (100) | < 0,001 | |
| > 11 years | 990 (85,6) | 166 (14,4) | 1156(100) | ||
| Skin Colour | |||||
| White | 545 (83,1) | 11 (16,9) | 656 (100) | 0,075 | |
| Black | 131 (75,3) | 43 (24,7) | 174 (100) | ||
| Pardon | 447 (78,8) | 120 (21,2) | 567 (100) | ||
| Yellow | 13 (72,2) | 5 (27,8) | 18 (100) | ||
| Did not want to declare | 11 (64,7) | 6 (35,3) | 17 (100) | ||
| Work situation | |||||
| Formal work | 602 (87,2) | 88 (12,8) | 690 (100) | < 0,001 | |
| Informal work | 161 (82,6) | 34 (17,4) | 195 (100) | ||
| Unemployed | 142 (68,9%) | 64 (31,1%) | 206 (100) | ||
| Retired/ pensioner | 3 (75,0) | 1 (25,0) | 4 (70,0) | ||
| Student | 244 (71,1) | 99 (28,9) | 343 (100) | ||
| Income | |||||
| < 1 MW | 100 (62,9) | 59 (37,1) | 159 (100) | < 0,001 | |
| 1–2 MW | 371 (78,4) | 102 (21,6) | 473 (100) | ||
| 3–4 MW | 288 (82,1) | 63 (17,9) | 351 (100) | ||
| 5–6 MW | 157 (86,7) | 24 (13,3) | 181 (100) | ||
| > 7 MW | 203 (90,2) | 22 (9,8) | 225 (100) | ||
| No income | 33 (67,3) | 16 (32,7) | 49 (100) | ||
| Marital status | |||||
| Single | 948 (78,7) | 257 (21,3) | 1205 (100) | 0,005 | |
| Married | 51 (83,6%) | 10(16,4%) | 61(100) | ||
| Stable union | 153 (89,0) | 19 (11,0) | 172 (100) | ||
| Alcohol consumption | |||||
| Yes | 890 (81,4) | 204 (18,6) | 1094 (100) | 0,035 | |
| No | 262 (76,2) | 82 (23,8) | 344 (100) | ||
| Tobacco use | |||||
| Yes | 226 (46,0) | 46 (16,9) | 272(100) | 0,172 | |
| No | 926(79,4) | 240(20,6) | 1166(100) | ||
| Brazilian Region | |||||
| North | 29 (69,0) | 13 (31,0) | 42 (100) | 0,010 | |
| Northeast | 485 (77,4) | 142(22,6) | 627 (100) | ||
| Midwest | 88 (78,6) | 24 (21,4) | 112 (100) | ||
| Southeast | 420 (82,7) | 88 (17,3) | 508 (100) | ||
| South | 130 (87,2) | 19 (12,8) | 149 (100) | ||
| Number of partners in the last three months | |||||
| 1–5 | 990 (78,2) | 276 (21,8) | 1266 (100) | < 0,001 | |
| 6–10 | 110 (94,8) | 6 (5,2) | 116 (100) | ||
| 11 + | 52 (92,9) | 4 (7,1) | 56 (100) | ||
| Number of partners in the last year | |||||
| 1–7 | 729 (76,2) | 22 (23,8) | 957 (100) | < 0,001 | |
| 8–15 | 225 (83,6) | 44 (16,4) | 269 (100) | ||
| 16 + | 198 (93,4) | 14 (6,6) | 212 (100) | ||
| Multiple partners | |||||
| Yes | 537 (75,8%) | 171 (24,2) | 708 (100) | < 0,001 | |
| No | 615 (84,2) | 115 (15,8) | 730 (100) | ||
| Age that began sexual activities (in Years) | |||||
| 10–19 | 922 (79,1) | 243 (29,9) | 1165 (100) | 0,160 | |
| 20–29 | 221 (84,4) | 41 (15,6) | 262 (100) | ||
| 30 + | 9 (81,8) | 2 (18,2) | 11 (100) | ||
| Most frequent sexual practice | |||||
| Oral | 267 (73,6%) | 96 (26,4%) | 363 (100,0%) | < 0,001 | |
| Receptive anal | 407 (79,6%) | 104 (20,4%) | 511 (100,0%) | ||
| Anal insertiva | 398 (85,8%) | 66 (14,2%) | 464 (100,0%) | ||
| Observer | 8 (66,7%) | 4 (33,3%) | 12 (100,0%) | ||
| Other | 72 (81,8%) | 16 (18,2%) | 88 (100,0%) | ||
| Had condomless anal intercourse in the last year | |||||
| Yes | 838 (83,3) | 168 (16,7) | 1006 (100) | < 0,001 | |
| No | 314 (72,7) | 118 (27,3) | 432 (100) | ||
| Used a condom in every sexual intercourse | |||||
| Yes | 171 (79,2) | 45 (20,8) | 216 (100) | 0,706 | |
| No | 981 (80,3) | 241 (19,7) | 1222 (100) | ||
| Used male condom in the last sexual intercourse | |||||
| Yes | 548 (81,2) | 135 (18,8) | 719 (100) | 0,290 | |
| No | 586 (79,0) | 151 (21,0) | 719 (100) | ||
| Had lubricating gel during sexual intercourse | |||||
| Yes | 970 (82,9) | 200 (17,1) | 1170 (100) | < 0,001 | |
| No | 182 (67,9) | 86 (32,1) | 268 (100) | ||
| Knew one place to seek HIV testing | |||||
| Yes | 947 (86,8) | 107 (10,2) | 1054 (100) | < 0,001 | |
| No | 205 (53,4) | 179 (46,6) | 384 (100) | ||
| Received counseling on HIV testing by a health professional | |||||
| Yes | 666 (92,6) | 53 (7,4) | 719 (100) | < 0,001 | |
| No | 486 (67,6) | 233 (32,4) | 719 (100) | ||
| Received counselling on HIV testing by a friend | |||||
| Yes | 583 (84,6) | 106 (15,4) | 689 (100) | < 0,001 | |
| No | 569 (76,0) | 180 (24,0) | 749 (100) | ||
| Received male condom for free in the last 12 months | |||||
| Yes | 720 (82,5) | 153 (17,5) | 873 (100) | 0,005 | |
| No | 432 (76,5) | 133 (23,5) | 565(100) | ||
| Read on the internet about HIV prevention in the last 12 months | |||||
| Yes | 977 (81,1) | 228 (18,9) | 1205 (100) | 0,037 | |
| No | 175 (75,1) | 58 (24,9) | 233 (100) | ||
| Read printed material on HIV prevention in the last 12 months | |||||
| Yes | 596 (80,0) | 149 (20,0) | 745 (100) | 0,913 | |
| No | 556 (80,2) | 137 (19,8) | 693 (100) | ||
| Had a STI diagnosis | |||||
| Yes | 483 (93,4) | 34 (6,6) | 517 (100) | < 0,001 | |
| No | 669 (72,6) | 252 (27,4) | 921 (100) | ||
| Knew someone living with HIV | |||||
| Yes | 759 (89,2) | 92 (10,8) | 851 (100) | < 0,001 | |
| No | 393 (67,0) | 194 (33,0) | 587 (100) | ||
| Sex worker | |||||
| Yes | 19 (70,4) | 8 (29,6) | 27 (100) | 0,201 | |
| No | 1133 (80,3) | 278 (19,7) | 1411 (100) | ||
| PrEP user | |||||
| Yes | 76 (93,8) | 5 (6,2) | 81 (100) | < 0,001 | |
| No | 1076 (79,3) | 281 (20,7) | 1357 (100) | ||
*P value
Moreover, having received male condoms for free in the last 12 months (p = 0.005), had already been diagnosed with an STI (p < 0.001), knew someone living with HIV (p < 0.001) and being a PrEP user (p < 0.001) had a statistically significant association with having already been tested for HIV.
Table 2 shows the logistic regression results. Had condomless anal intercourse in the last 12 months (AOR 1,659; 95% Confidence Interval [CI]:1,12 − 2,43; p = 0,010), Knew one place to seek HIV testing (AOR 6,158 [IC95%: 4,27 − 8,86]; p < 0,001), Received counselling on HIV testing by a health professional (AOR 3,389 [IC95%: 2,28 − 5,02]; p < 0,001), Have been diagnosed with STI (AOR 2,266 [IC95%: 1,41 − 3,62]; p < 0,001) and Knew someone living with HIV (AOR 1,86 [IC95%: 1,29 − 2,67]; p < 0,001) were independently associated with higher chances of HIV testing.
Table 2.
Adjusted model of factors associated with HIV testing among men who have sex with men living in Brazil, 2020
| Variables | Crude Odds [95% IC*] |
p † | Adjusted Odds [95% IC*] | p † | |||
|---|---|---|---|---|---|---|---|
| Schooling | |||||||
| < 11 years | 0,226 [0,17 − 0,30] | < 0,001 | 0,421 [0,27 − 0,64] | < 0,001 | |||
| > 11 years | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Skin Colour | |||||||
| White | 0,982 [0,11 − 8,49] | 0,987 | 0,322 [0,02–4,60] | 0,403 | |||
| Black | 0,609 [0,06 − 5,36] | 0,655 | 0,242 [0,01–3,55] | 0,301 | |||
| Pardon | 0,745 [0,08 − 6,44] | 0,789 | 0,311 [0,02–4,40] | 0,388 | |||
| Yellow | 0,520 [0,04–5,63] | 0,591 | 0,244 [0,01–5,01] | 0,360 | |||
| Did not want to declare | 0,367 [0,03–3,91] | 0,406 | 0,208 [0,00–4,31] | 0,310 | |||
| Other | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Gender | |||||||
| Cisgender Man | 1,48 [0,62 − 3,53] | 0,374 | 1,145 [0,34 − 3,82] | 0,825 | |||
| Non-binary | 0,46 [0,28 − 1,78] | 0,466 | 0,654 [0,18 − 2,30] | 0,509 | |||
| Other | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Region of Brazil | |||||||
| North | 0,326 [0,14 − 0,73] | 0,007 | 0,221 [0,07 − 0,68] | 0,009 | |||
| Northeast | 0,499[0,29 − 0,83] | 0,008 | 0,729 [0,37 − 1,42] | 0,357 | |||
| Midwest | 0,536 [0,27 − 1,03] | 0,064 | 0,996 [0,41 − 2,37] | 0,992 | |||
| Southeast | 0,698 [0,40 − 11,18] | 0,186 | 0,905 [0,45 − 1,78] | 0,774 | |||
| South | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Number of partners in the last three months | |||||||
| 8–15 | 5,11 [2,22 − 11,75] | < 0,001 | 2,093 [0,71 − 6,12] | 0,178 | |||
| 16+ | 3,62 [1,30 − 10,11] | 1,802 [0,33 − 9,56] | 0,489 | ||||
| 1–7 | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Number of partners in the last year | |||||||
| 8–15 | 1,60 [1,12 − 2,28] | < 0,01 | 1,070 [0,66 − 1,72] | 0,779 | |||
| 16+ | 4,42 [2,52 − 7,76] | < 0,001 | 2,196 [0,95 − 5,07 | 0,066 | |||
| 1–7 | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Sexual orientation | |||||||
| Gay | 2,28 [1,38 − 3,76] | 0,001 | 0,652 [0,40 − 1,04] | 0,077 | |||
| Bisexual | 1,04 [0,58 − 1,85] | 0,889 | 0,921 [0,46 − 1,84] | 0,817 | |||
| Other | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Age group (full years) | |||||||
| 18–28 | 0,272 [0,13 − 0,57] | < 0,001 | 0,354 [0,13 − 0,93] | 0,037 | |||
| 29–39 | 1,370 [0,60 − 3,10] | 0,449 | 0,934 [0,34 − 2,54] | 0,894 | |||
| 40 + | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Work situation | |||||||
| Formal work | 2,776 [2,00–3,84] | < 0,001 | 1,164 [0,73 − 1,84] | 0,520 | |||
| Informal work | 1,921 [1,24 − 2,98] | 0,003 | 1,07 [0,59 − 1,93] | 0,809 | |||
| Unemployed | 0,900 [0,61 − 1,31] | 0,584 | 0,713 [0,42 − 1,20] | 0,209 | |||
| Retired/ pensioner | 1,217 [0,12 − 11,84] | 0,866 | 0,146 [0,00–6,96] | 0,329 | |||
| Student | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Monthly family income | |||||||
| < 1 MW | 0,822 [0,41 − 1,62] | 0,571 | 0,936 [0,37 − 2,32] | 0,886 | |||
| 1–2 MW | 1,764 [0,93 − 3,33] | 0,080 | 1,448 [0,61 − 3,38] | 0,394 | |||
| 3–4 MW | 2,216 [1,15 − 4,27] | 0,017 | 1,177 [0,47 − 2,89] | 0,722 | |||
| 5–6 MW | 3,172 [1,52 − 6,62] | 0,002 | 1,283[0,46 − 3,52] | 0,629 | |||
| 7 + MW | 4,47 [2,13 − 9,39] | < 0,001 | 2,133 [0,78 − 5,76] | 0,136 | |||
| No income | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Marital status | |||||||
| Single | 0,458 [0,27 − 0,75] | 0,002 | 0,799 [0,40 − 1,56] | 0,514 | |||
| Married | 0,633 [0,27 − 1,45] | 0,280 | 0,419 [0,15 − 1,16] | 0,096 | |||
| Stable union | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Had steady partner | |||||||
| Yes | 1,80 [1,36 − 2,39] | < 0,001 | 1,384 [0,88 − 2,15] | 0,150 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Alcohol comsumption | |||||||
| Yes | 1,37 [1,02 − 1,83] | 0,036 | 0,853 [0,56 − 1,28] | 0,443 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Tobacco consumption | |||||||
| Yes | 1,27 [0,90 − 1,80] | 0,173 | 0,875 [0,54 − 1,40] | 0,580 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Most frequent sexual practice | |||||||
| Oral | 0,618 [0,34 − 1,11] | 0,110 | 0,474[0,21 − 1,04] | 0,063 | |||
| Receptive anal | 0,870 [0,48 − 1,56] | 0,639 | 0,631 [0,28 − 1,37] | 0,248 | |||
| Anal insertiva | 1,340 [0,73 − 2,44] | 0,340 | 0,740 [0,33 − 1,64] | 0,460 | |||
| Observer | 0,444 [0,11 − 1,66] | 0,227 | 1,103 [0,20 − 5,99] | 0,910 | |||
| Other | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Had condomless anal intercourse in the last 12 months | |||||||
| Yes | 1,187 [1,43 − 2,45] | < 0,001 | 1,659 [1,12 − 2,43] | 0,010 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Had lubricating gel during sexual intercourse | |||||||
| Yes | 2,29 [1,70 − 3,09] | < 0,001 | 1,245 [0,82 − 1,87] | 0,296 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Knew one place to seek HIV testing | |||||||
| Yes | 7,73 [5,82 − 10,26] | < 0,001 | 6,158 [4,27 − 8,86] | < 0,001 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Received counselling on HIV testing by a health professional | |||||||
| Yes | 6,02 [4,37 − 8,30] | < 0,001 | 3,389 [2,28 − 5,02] | < 0,001 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Received counseling about HIV testing by a friend | |||||||
| Yes | 1,74 [1,33 − 2,27] | < 0,001 | 1,109 [0,77 − 1,58] | 0,569 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Received male condom for free in the last 12 months | |||||||
| Yes | 1,45 [1,12 − 1,88] | 0,005 | 0,954 [0,66 − 1,36] | 0,798 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Read on the internet about HIV prevention in the last 12 months | |||||||
| Yes | 1,42 [1,02 − 1,98] | 0,037 | 0,868 [0,54 − 1,37] | 0,544 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Have been diagnosed with STI | |||||||
| Yes | 5,35 [3,67 − 7,80] | < 0,001 | 2,266 [1,41 − 3,62] | < 0,001 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Knew someone living with HIV | |||||||
| Yes | 4,07 [3,09 − 5,37] | < 0,001 | 1,86 [1,29 − 2,67] | < 0,001 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| PrEP user | |||||||
| Yes | 3,97 [1,59 − 9,90] | 0,003 | 2,316 [0,69 − 7,73] | 0,173 | |||
| No | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
| Age that began sexual activities (in Years) | |||||||
| 10–19 | 0,843 [0,18 − 3,93] | 0,828 | 2,005 [0,19–20,57] | 0,558 | |||
| 20–29 | 1,198 [0,25 − 5,75] | 0,821 | 1,877 [0,18–19,45] | 0,598 | |||
| 30+ | Ref. ‡ | Ref. ‡ | Ref. ‡ | Ref. ‡ | |||
*95% Confidence Interval; † P value; ‡Reference category
Moreover, the Receiver Operator Characteristic (ROC) Curve, in Fig. 1, was presented to demonstrate the quality of the model’s fit. It was evidenced that the model’s accuracy was 0.893 and sensitivity was 0.947. Thus, the results show that the model performed well in estimating the likelihood of adherence to HIV testing. The results were obtained using Jamovi software (version 2.3).
Fig. 1.
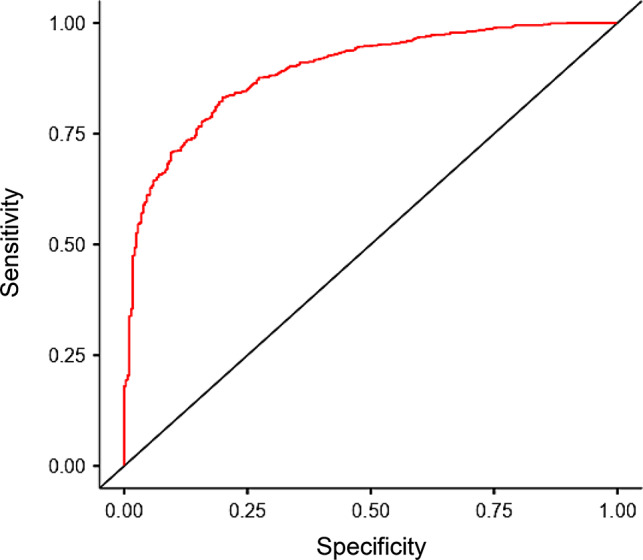
ROC curve of the adjusted model
Discussion
We investigated the impact of sociodemographic and behavioural factors on HIV testing among MSM across Brazil. Notwithstanding the advancements in the expansion of health services, the attainment of the 95-95-95 objective for HIV prevention continues to present a significant challenge. The proportion of MSM who have never undergone testing (19.9%) in this study is comparable to that observed in the Netherlands [12], suggesting a potential deficit in demand for testing services, even in countries with disparate levels of social and economic advancement.
Our findings indicated that the following factors were independently associated with an increased likelihood of HIV testing: Those who had engaged in unprotected anal intercourse in the previous 12 months; those who were aware of a single location where they could access HIV testing; those who had received counselling on HIV testing from a healthcare professional; those who had been diagnosed with an STI and knew someone who was living with HIV. These findings are consistent with those of other research studies. Unprotected anal intercourse without the use of PrEP is a common occurrence in both national and international studies. Nevertheless, the potential for HIV infection exposure may serve as a motivating factor for these men to seek testing services and ascertain their HIV status. Indeed, other research has identified high rates of unprotected anal sex (76.9%) among MSM, and this behaviour is associated with other risk factors, such as the use of psychoactive substances [14]. A study conducted by Chinese researchers yielded similar findings [15].
Another noteworthy observation was that MSM aware of a testing facility were likelier to undergo testing. This is a crucial finding because an absence of knowledge about HIV testing sites has been documented in international literature as a significant barrier to testing adherence, ultimately leading to lower adherence to combination prevention strategies. However, the lack of awareness about testing locations may be even more impactful for immigrants [16]. These findings highlight the necessity for HIV tests to be made accessible to MSM through strategies that effectively reach this demographic, such as the distribution of tests via dating apps and community-based organisations [17]. It is essential that efforts to provide testing for MSM be ongoing and that healthcare professionals establish closer connections with this group. Furthermore, they must create welcoming health spaces that can facilitate the gradual integration of these men into health services. The authors highlight the necessity for readily accessible testing services for MSM [18], whether provided in healthcare facilities or through community-leader-based services.
Those who received counselling about HIV testing from a healthcare professional were more likely to have undergone an HIV test at some point in their lives. It is of particular note that healthcare professionals play a pivotal role in the promotion of HIV testing, given their involvement at various stages, including counselling and the maintenance of professional confidentiality. These elements are of paramount importance in the context of HIV testing and treatment clinics. In Brazil, the confidentiality of diagnosis is enshrined in legislation, thereby protecting individuals living with HIV from having their positive diagnosis disclosed in healthcare services, educational institutions, workplaces, public administration, law enforcement, judicial processes, and in written and audiovisual media [19]. Moreover, confidentiality regarding testing procedures and professional ethics is vital for ensuring the security of MSM. It is thus imperative that healthcare professionals provide humane care for MSM and foster trust to strengthen these relationships. Welcoming care has been demonstrated to facilitate access and build bonds between professionals and patients, thereby fostering trust [20]. Indeed, the international literature provides ample documentation of the barriers related to test confidentiality [21–23].
Other factors associated with adherence to HIV testing, as revealed by this study, included being diagnosed with an STI and being acquainted with a person living with HIV. A diagnosis of another STI may prompt MSM to comply with HIV testing. However, a comprehensive systematic review revealed that individuals who sought treatment for an STI often failed to take the opportunity to test for HIV, with only 35.3% of individuals diagnosed with another STI undergoing HIV testing. Policymakers need to consider various aspects of testing services, including infrastructure, test availability, human resource qualifications, and institutional policies for HIV and STI prevention and control [24].
It is important to consider certain limitations while interpreting our results. Firstly, the recruitment of the group investigated in this study took place in networks and social media that produced content aimed at the LGBTQQICAAPF2K + audience (Lesbian, Gay, Bisexual, Transgender, Queer, Questioning, Intersex, Curious, Asexual, Allied, Pansexual, Polysexual, Family, 2-spirits and Kink). Therefore, the sample composition may not represent the population that does not use these networks. Secondly, the concentration of MSM on social networks may have overestimated a certain group that has very similar characteristics. MSM part of the queer community, for example, may have been left out of the study due to do not identify with the community LGBTQQICAAPF2K+. Thus, we may have overestimated the characteristics of the group that participated in the research.
Further investigation of other social, economic, behavioural, and health factors that may predict acceptance, adherence, and completion of HIV testing among MSM should be considered for future research. In conclusion, we found the frequency of never-tested MSM is still significant despite the advances in prevention methods.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Abbreviations
- UHS
Unified Health System (in Portuguese: Sistema Único de Saúde – SUS)
- HIV
Human Immunodeficiency Virus (HIV)
- AIDS
Human Immunodeficiency Syndrome
- MSM
men who have sex with men
- UNAIDS
Joint United Nations Program on HIV/AIDS
- COR
Crude Odds Ratio
- AOR
Adjusted Odds Ratio
Author contributions
Conceptualization, L.R.M.S., R.K.R., M. W., and E.G.; Methodology, L.R.M.S., R.K.R., M. W., and E.G.; Formal Analysis, L.R.M.S. and D.M.R.; Investigation, L.R.M.S., R. A. G. C., D. M. R., M. A., M. J. C. F., M. W., E.G., R. K. R.; Resources, L.R.M.S., E.G., R.K.R.; Data curation, L.R.M.S.; Funding acquisition, none; Writing—original draft preparation, all authors.; Writing—review and editing, all authors.; Visualization, R.K.R and E.G.; Supervision, R.K.R and E.G.; Project administration, R.K.R and E.G.; All authors have read and agreed to the published version of the manuscript.
Funding
none.
Data availability
The data sets used and/or analyzed during the present study are available with the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study followed all the guidelines of the Declaration of Helsinki and the Brazilian National Health Council Resolution 466/12. It was approved by the Ethics in Research Committee of the Ribeirão Preto College of Nursing, under number 3.172.445. Consent to participate in the study was given in electronic signature by all participants before data collection. They signed the Informed Consent Form. It is a document with specific information about the research containing the main objectives, possible risks and benefits, and information about confidentiality, privacy, and information about the research coordinators. The anonymity of all participants was preserved.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Joint United Nations Programme on HIV/Aids (UNAIDS). UNAIDS data. 2019. https://www.unaids.org/en/resources/documents/2019/2019-UNAIDS-data [PubMed]
- 2.Kerr LR, Mota RS, Kendall C, Pinho Ade A, Mello MB, Guimarães MD, Dourado I, de Brito AM, Benzaken A, McFarland W, Rutherford G, HIVMSM Surveillance Group. HIV among MSM in a large middle-income country. AIDS. 2013;27[62]:427 – 35. 10.1097/QAD.0b013e32835ad504 [DOI] [PubMed]
- 3.Kerr L, Kendall C, Guimarães MDC, Salani Mota R, Veras MA, Dourado I, et al. HIV prevalence among men who have sex with men in Brazil. Medicine. 2018;9763:S9–15. 10.1097/MD.0000000000010573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyrer C, Sullivan P, Sanchez J, Baral SD, Collins C, Wirtz AL, Altman D, Trapence G, Mayer K. The increase in global HIV epidemics in MSM. AIDS. 2013;2764:2665–78. 10.1097/01.aids.0000432449.30239.fe. [DOI] [PubMed] [Google Scholar]
- 5.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, Brookmeyer R. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380[65]:367 – 77. 10.1016/S0140-6736[66]60821-6 [DOI] [PMC free article] [PubMed]
- 6.Trapence G, Collins C, Avrett S, Carr R, Sanchez H, Ayala G, Diouf D, Beyrer C, Baral SD. From personal survival to public health: community leadership by men who have sex with men in the response to HIV. Lancet. 2012. 10.1016/S0140-6736(12)60834-4. 380[65]:400 – 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altman D, Aggleton P, Williams M, Kong T, Reddy V, Harrad D, Reis T, Parker R. Men who have sex with men: stigma and discrimination. Lancet. 2012;380(65):439–45. 10.1016/S0140-6736[66]60920-9. [DOI] [PubMed] [Google Scholar]
- 8.Valdiserri RO, Holtgrave DR, West GR. Promoting early HIV diagnosis and entry into care. AIDS. 1999;1364:2317–30. 10.1097/00002030-199912030-00003. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. HIV Testing. 2022. https://www.cdc.gov/hiv/testing/index.html
- 10.Monteiro SS, Brigeiro M, Vilella WV, Mora C, Parker R. Challenges facing HIV treatment as prevention in Brazil: an analysis drawing on literature on testing. Cien Saude Colet. 2019;2467:1793–807. 10.1590/1413-81232018245.16512017. Portuguese, English. [DOI] [PubMed] [Google Scholar]
- 11.Joint United Nations Programme on HIV/Aids (UNAIDS). Fast-Track—Ending the AIDS epidemic by 2030. https://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf:2014
- 12.Leenen J, Wijers JNAP, Den Daas C, de Wit J, Hoebe CJPA, Dukers-Muijrers NHTM. HIV testing behaviour and associated factors in men who have sex with men by level of urbanisation: a cross-sectional study in the Netherlands. BMJ Open. 2022;12[68]:e049175. 10.1136/bmjopen-2021-049175 [DOI] [PMC free article] [PubMed]
- 13.The jamovi project. jamovi. (Version 2.3) [Computer Software]. 2022. Retrieved from https://www.jamovi.org
- 14.Passaro RC, Castañeda-Huaripata A, Gonzales-Saavedra W, Chavez-Gomez S, Segura ER, Lake JE, Clark JL. Contextualizing condoms: a cross-sectional study mapping intersections of locations of sexual contact, partner type, and substance use as contexts for sexual risk behavior among MSM in Peru. BMC Infect Dis. 2019;19:1–12. 10.1186/s12879-019-4517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ibragimov U, Harnisch JA, Nehl EJ, He N, Zheng T, Ding Y, Wong FY. Estimating self-reported sex practices, drug use, depression, and intimate partner violence among MSM in China: a comparison of three recruitment methods. AIDS Care. 2017;291. 10.1080/09540121.2016.1201191. [DOI] [PMC free article] [PubMed]
- 16.Deblonde J, Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Pub Health. 2010;204:422–32. 10.1093/eurpub/ckp231. [DOI] [PubMed] [Google Scholar]
- 17.Ren C, Tucker JD, Tang W, Tao X, Liao M, Wang G, Ma W. Digital crowdsourced intervention to promote HIV testing among MSM in China: study protocol for a cluster randomized controlled trial. Trials. 2020;21:1–9. 10.1186/s13063-020-04860-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persson KI, Berglund T, Bergström J, Eriksson LE, Tikkanen R, Thorson A, Forsberg BC. Motivators and barriers for HIV testing among men who have sex with men in Sweden. J Clin Nurs. 2016;3605–18. 10.1111/jocn.13293. 25[23–24]. [DOI] [PubMed]
- 19.Brasil. Senado Federal. Projeto de Lei 7658/2014. Brasília, Distrito Federal, 2020. https://www.camara.leg.br/propostas-legislativas/618055
- 20.Sousa LRM, Mesquita RFD, Matos FRN, Moura LKB, Moura MEB. Dimensões da satisfação dos usuários da Estratégia Saúde da Família. Revista Portuguesa De Investigação Comportamental E Social. 2017, 3[2]: 2–9. 10.7342/ismt.rpics. 2017.3.2.50.
- 21.Hoyos J, Fernández-Balbuena S, Fuente L, Sordo L, Ruiz M, Barrio G. Madrid Rapid HIV Testing Group. Never tested for HIV in Latin‐American migrants and spaniards: prevalence and perceived barriers. Afr J Reprod Gynaecol Endoscopy. 2013, 161. [DOI] [PMC free article] [PubMed]
- 22.Joseph HA, Belcher L, O’Donnell L, Fernandez MI, Spikes PS, Flores SA. HIV testing among sexually active Hispanic/Latino MSM in Miami-Dade County and New York City: opportunities for increasing acceptance and frequency of testing. Health Promot Pract. 2014;156:867–80. 10.1177/152483991453749. [DOI] [PubMed] [Google Scholar]
- 23.George-Svahn L, Eriksson LE, Wiklander M, Björling G, Svedhem V, Brännström J. Barriers to HIV testing as reported by individuals newly diagnosed with HIV infection in Sweden. AIDS Care. 2021;3310:1286–95. [DOI] [PubMed] [Google Scholar]
- 24.Saleem K, Ting EL, Loh AJ, Baggaley R, Mello MB, Jamil MS, Ong JJ. Missed opportunities for HIV testing among those who accessed sexually transmitted infection (STI) services, tested for STIs and diagnosed with STIs: a systematic review and meta-analysis. J Int AIDS Soc. 2023;264. 10.1002/jia2.26049. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets used and/or analyzed during the present study are available with the corresponding author upon reasonable request.


