Abstract
Background
As women get older, their health priorities change. We surveyed a sample of older Canadian women to investigate what health priorities are of concern to them, their perceptions about the care delivered to address these priorities and the extent to which priorities and perceptions of care differ across age groups and provinces.
Methods
The WOW (What Older women Want) cross-sectional health survey was mailed in October 2003 to 5000 community-dwelling women aged 55–95 years from 10 Canadian provinces. Women were asked questions on 26 health priorities according to the World Health Organization's International Classification of Functioning, Disability and Health, and their perceptions of whether these priorities were being addressed by health care providers through screening or counselling. Differences in priorities and perceptions of care delivery were examined across age groups and provinces.
Results
The response rate was 52%. The mean age of the respondents was 71 (standard deviation 7) years. The health priorities identified most frequently by the respondents were preventing memory loss (88% of the respondents), learning about the side effects of medications (88%) and correcting vision impairment (86%). Items least frequently selected were counselling about community programs (28%), counselling about exercise (33%) and pneumonia vaccination (33%). Up to 97% of the women recalled being adequately screened for heart disease and stroke risk factors, but as little as 11% reported receiving counselling regarding concerns about memory loss or end-of-life issues. Women who stated that specific priorities were of great concern or importance to them were more than twice as likely as those who stated that they were not of great concern or importance to perceive that these priorities were being addressed: osteoporosis (odds ratio [OR] 2.6, 95% confidence interval [CI] 2.1–3.2), end-of-life care (OR 2.6, 95% CI 2.0–3.4), anxiety reduction (OR 2.2, 95% CI 1.8–2.6), fall prevention (OR 2.1, 95% CI 1.6–2.7), stroke (OR 2.1, 95% CI 1.4–3.0), depression (OR 2.1, 95% CI 1.7–2.7) and urinary incontinence (OR 2.1, 95% CI 1.7–2.5). The respondents' perceptions of care delivery varied across age groups and provinces.
Interpretation
According to the perceptions of surveyed women, health care providers are addressing many, but not all, of their health concerns, especially those that are of great concern or importance to these women.
As women's life expectancy increases, physicians are confronted with the challenge of treating an elderly population that is predominantly female and has a variety of health priorities and needs. Older women face functional, psychological and social difficulties in addition to health-related conditions. One solution to align care more closely with women's health priorities is to practise patient-centred care, whereby clinical decision-making is focused primarily on the priorities and preferences of individual patients.1,2,3 Data on older women's health priorities are scarce,4,5,6 and understanding the gamut of their concerns is important for directing patient-centred, priority-driven agendas. The WOW — What Older women Want — health survey was conducted to determine health priorities of older Canadian women and the extent to which women perceive that their priorities are being addressed by health care professionals.
Methods
The WOW health survey, conducted in October 2003, was a cross-sectional mailed survey of community-dwelling women aged 55–95 years from 10 Canadian provinces. The sampling frame consisted of all households whose addresses were registered with Canada Post. The women in this age group who responded to 2 household-level Canada Post surveys during 2002 (n = 216 040) made up the study list sample; they represented 15%– 18% of people who responded from all households surveyed (every household in Canada received a Canada Post survey). For the WOW study sample, a computer-generated random sample of 5000 names and addresses of women 55 years and older was obtained from the list of respondents to the Canada Post surveys. We used a higher sampling fraction for women aged 65 years and over to ensure adequate representation of women in older groups (a ratio of 15% women aged 55–64 and 85% women aged 65 and over). The self-administered questionnaire with prestamped return envelopes was mailed to participants once only. Women who had originally responded to the Canada Post survey in French were mailed a French questionnaire. The Ethics Board of the Institut universitaire de gériatrie de Montréal approved the study protocol.
The WOW questionnaire asked women to rate the importance of 26 health-priority items that had been generated from qualitative work with community-dwelling women aged 65 and over5 and tested in a community sample.6 The conceptual framework proposed by the World Health Organization's International Classification of Functioning, Disability and Health was used to categorize priorities into 3 groups: health conditions, functioning and contextual factors.7 Health conditions included breast cancer, heart disease, stroke, Alzheimer's disease, colon cancer, hip fracture, osteoporosis, falls, diabetes mellitus and pneumonia (for which preventive influenza and pneumococcal vaccines are available). Priorities that fell under the functioning category included common symptoms associated with advanced age that negatively affected function, namely urinary incontinence, muscle weakness, memory problems, vision loss, pain and depression. Contextual factors were defined as priorities related to personal beliefs, communication or environmental issues associated with aging and access to care. Respondents were asked to rate their level of concern (greatly, somewhat, a little or not at all concerned) over developing the different health conditions listed and to indicate the degree of importance they attributed to preventing loss of function and addressing contextual factors (very, somewhat, a little or not at all important).
To learn about women's perceptions of the care they received to address these health priorities, we asked respondents to indicate whether they recalled receiving screening procedures or counselling from their health care providers to address each priority item. For items related to health conditions, questions about the frequency and type of screening were based on recommendations by the Canadian Task Force on Preventive Health Care and the US Preventive Services Task Force and other relevant literature.8,9,10 For breast cancer, respondents were asked whether they had received a mammogram or had had their breasts examined for “lumps” in the 2 years before the survey. For heart disease and stroke, they were asked about yearly blood pressure measurements and cholesterol screening. For Alzheimer's disease, they were asked about memory testing. For colon cancer, they were asked about yearly stool screening for occult blood, or colonoscopy or sigmoidoscopy screening every 5 years. For osteoporosis, they were questioned about ever having undergone bone mineral density testing or “bone x-rays” to check for brittle bones. For diabetes, women were asked whether they received blood tests to check for high blood sugar at least every 3 years, and for pneumonia whether they had received a flu vaccine yearly. For each of the functioning and contextual priorities, women were asked to indicate whether any of their health care providers had ever addressed these items with them (Yes or No).
Standard sociodemographic data were collected. Self-rated physical and mental health status was measured with the use of the Physical Component Summary (PCS) and Mental Component Summary (MCS) scales of the Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12).11,12 This measure allowed us to compare health status data for the study sample with normative health status data for Canadian women aged 65 and over.12 The 6-digit postal code was retained for each respondent to determine provincial origin and whether each participant resided in an urban or rural area. Income level was not queried directly, but aggregated census data were used to infer the mean income level for each respondent according to the first 3 digits of her postal code.
Data from the completed questionnaires were entered into a computer database and checked for accuracy by a second data-entry assistant. Descriptive statistics were used to estimate proportions of women indicating specific health priorities and perceptions of care. For all remaining analyses, priorities were divided into 2 groups: those “of great concern or importance” and those “not of great concern or importance” (i.e., priorities rated as somewhat, a little bit or not at all important). To estimate the likelihood of respondents perceiving that specific health priorities were being addressed by their health care providers when those priorities were of great concern or importance to them, priorities were regressed individually on corresponding perceptions of care using logistic regression analysis. Regression analyses were adjusted for age and for physical and mental health status of the respondents. Results are reported as odds ratios (OR) with 95% confidence intervals (CI).
Differences in the frequency of specific priorities and perceptions of care by age group (55–64, 65–69, 70–74, 75–79 and ≥ 80 years) were tested using χ2 analyses, with significance set at a p value of less than 0.05. To test the hypothesis that there was no provincial variation in women's perceptions of the care they received for addressing different health priorities, we assumed that each province had an equal probability of being ranked first or last with respect to the proportion of women in each province stating that a given priority was being addressed. We used a normal distribution around 3.7 (26 health items divided by 7 provincial groupings) to test whether the observed frequency of a province being ranked first or last fell within the expected frequency of 3.7 in a uniform distribution. Significant variations outside of expected frequencies for first or last rankings were determined with the use of the χ2 test (p < 0.05). To ensure an adequate sample size, we grouped women from the Atlantic provinces together.
A sample size of 5000 was calculated on the basis of an expected 50% response rate from a pilot mailing of 150 questionnaires. This sample size was chosen to provide estimates of proportions of women stating health priorities who are in subgroups with a minimum prevalence of 10% (e.g., caregivers) and the most conservative response rate of 50% with an accuracy of ± 5% (99 times out of 100). The use of data from the entire sample would be expected to result in estimates of proportions with an accuracy of ± 2.5% (99 times out of 100). For subgroups of 200–300 women, the estimated proportions would be expected to be accurate within 6%–7% (95 times out of 100).
Results
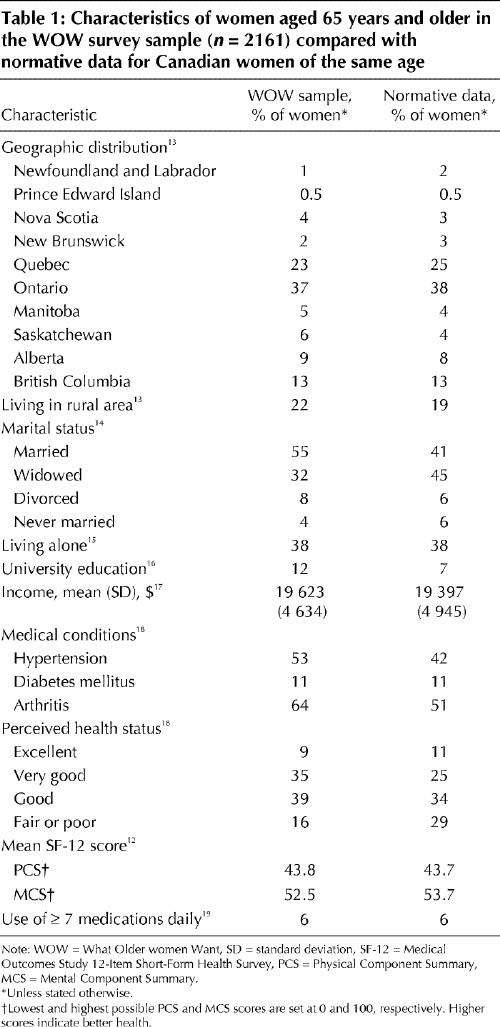
The response rate was 52%. Nonrespondents had similar geographic distribution, age and language characteristics as the respondents (data not shown). The mean age of the respondents was 71 years (standard deviation 7, range 55–95, median 71); 16% were 55–64 years old, and 84% were 65 years and older. The representativeness of the respondents aged 65 and older in comparison with the general elderly female population in Canada is shown in Table 1.12,13,14,15,16,17,18,19 We compared women in this age group and not those aged 55–64 because of the way Canadian norms are reported in the 2001 census data (age groups 18–44, 45–64, ≥65 years). Respondents aged 55–64 were better educated (20% v. 12% had a university education), physically healthier (mean PCS score 46.1 v. 43.4) and less likely to live alone (16% v. 38%) than the older respondents.
Table 1
The health priorities most frequently identified by the respondents were preventing memory loss (88% of the respondents), learning about the side effects of medications (88%) and correcting vision impairment (86%) (Table 2). Health priorities least frequently identified were counselling about community programs (28%), counselling about exercise (33%) and pneumonia vaccination (33%). Up to 97% of the women recalled being adequately screened for heart disease and stroke risk factors, but as little as 11% reported receiving counselling regarding concerns about memory loss or end-of-life issues.
Table 2
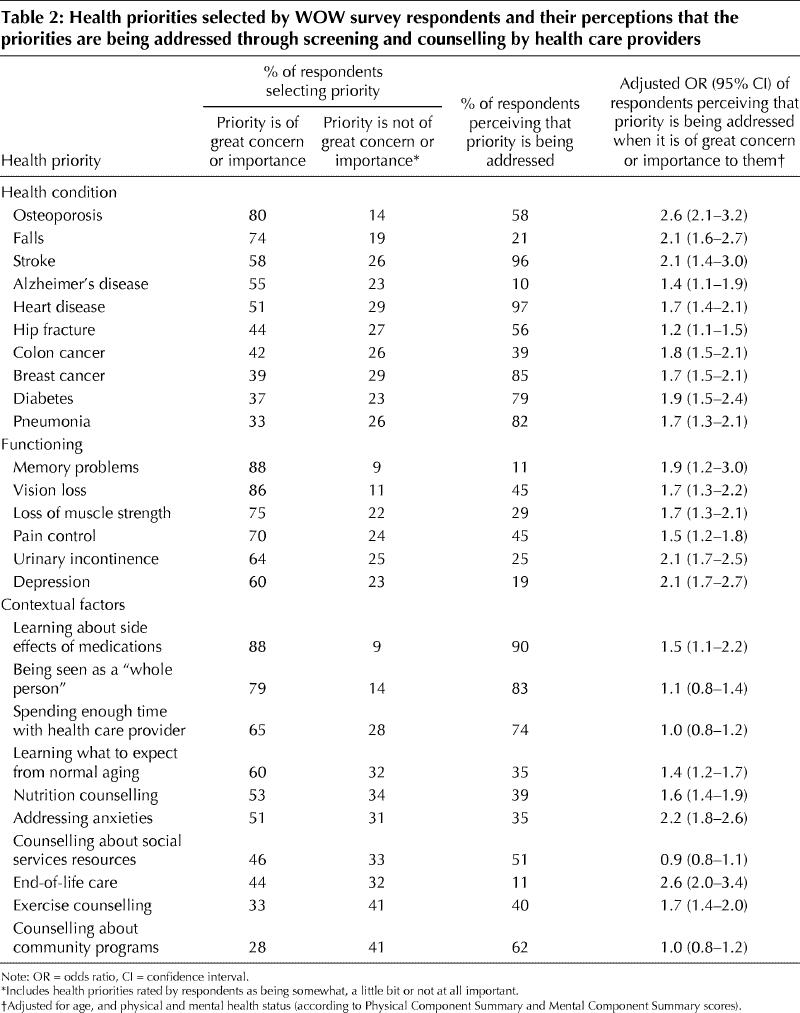
For all priorities related to health conditions and functioning issues, women who stated that the priorities were of great concern or importance to them were significantly more likely than those who stated that they were not of great concern or importance to them to perceive that these priorities were being addressed by their health care provider (Table 2). For 4 of the contextual priorities — being seen as a “whole person,” spending enough time with the health care provider, receiving counselling about social services resources and receiving counselling about community programs — the respondents' perceptions that care was being provided were not significantly associated with their reports that these priorities were of great importance to them.
For the most part, the proportions of women with specific priorities and perceptions of care were similar across the age groups. Only a few priorities significantly decreased in frequency with increasing age (Fig. 1). Among these, concerns about treating depression and reducing anxiety were most notably less frequent in later years. Concerns about hip fracture and being informed about social services increased slightly in the older groups but did not remain significant in post hoc regression analyses after adjustment for physical and mental health status (data not shown).
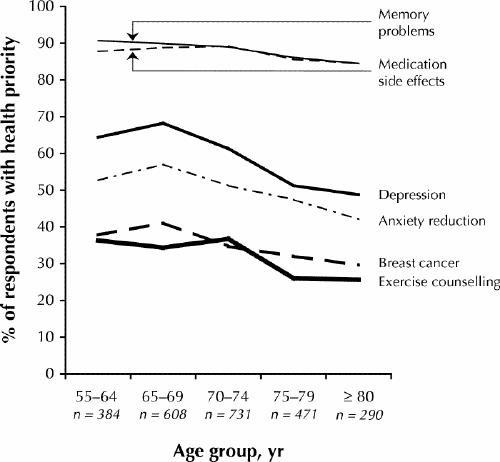
Fig. 1: Health priorities that decreased in frequency with increasing age of respondents. Proportions shown are unadjusted and differed significantly (p < 0.05) between age groups in χ2 analyses.
Fig. 2 shows the age-related differences in the proportions of women who perceived that care was being delivered. The largest reported significant difference in the perception of care delivery between the younger and older women was for breast cancer screening: 92% of those aged 55–64 reporting having received screening mammography or clinical breast examination during the 2 years before the survey, compared with 66% of those 80 years and older (Fig. 2, left panel). The opposite was true for pneumonia vaccination: 65% of women in the youngest group reported being vaccinated, compared with 91% of those in the oldest group (Fig. 2, right panel).
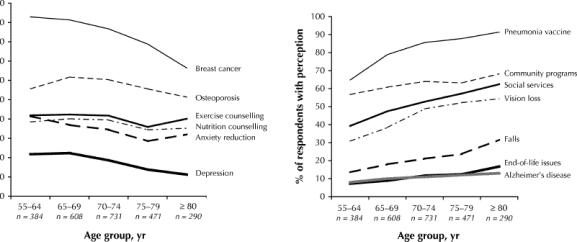
Fig. 2: Age-related differences in the proportions of women who perceived that health priorities were being addressed by their health care providers. Left: Health priorities for which more women in the younger groups than in the older groups perceived as being addressed. Right: Health priorities for which more women in the older groups than in the younger groups perceived as being addressed. Proportions shown are unadjusted and differed significantly (p < 0.05) between age groups in χ2 analyses.
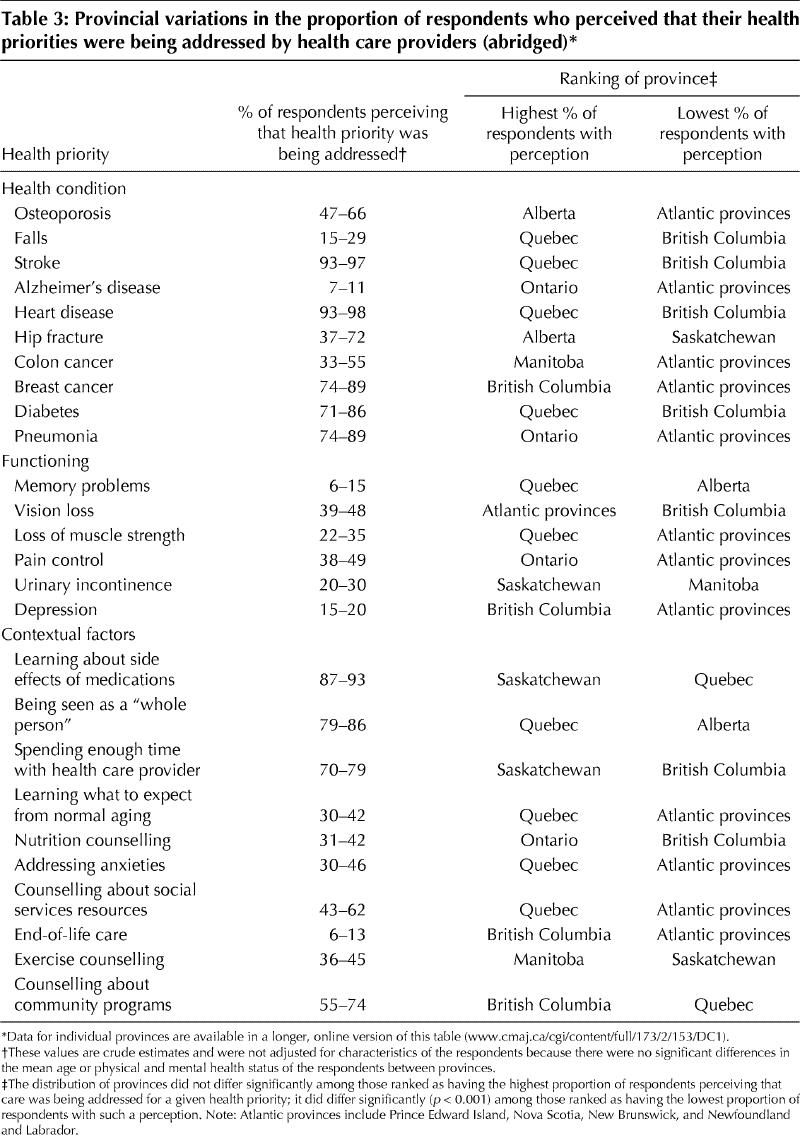
Provincial variations in the proportion of respondents who perceived that care was being delivered to address different health priorities are presented in Table 3. Quebec was ranked as having the highest proportion for 10 of the 26 health priorities; however, although this frequency was greater than the expected frequency of 3.7, it did not quite reach statistical significance (χ2 = 10.73, 6 degrees of freedom [df], 0.01 > p > 0.05). The Atlantic provinces were ranked as having the lowest proportion for 12 of the 26 health priorities; this frequency did differ significantly from the expected frequency of 3.7 (χ2 = 18.6, 6 df, p < 0.01).
Table 3
Interpretation
The results of this large national survey suggest that older women's health priorities encompass a wide range of physical, functional and psychosocial concerns about aging. The respondents' priorites remained fairly consistent in early and late postmenopausal years. Perceptions of whether care was being delivered to address these health priorities varied according to the priority in question and, to a lesser extent, the age of the respondents and possibly the province in which they lived. For the most part, however, women who considered a specific health issue to be of great concern or importance to them were more likely than those who did not consider it to be of great concern or importance to perceive that care was being delivered to address the issue of concern.
These results should be interpreted in light of several limitations. The first is the relatively low response rate. Only 52% of the women who were sent the questionnaire completed and returned it. Although this response rate is consistent with rates in other mailed health surveys involving elderly people,20,21 a selection bias necessarily emerges: the WOW respondents aged 65 and older were more educated and slightly healthier than the average Canadian woman in the same age group. In addition, a sampling bias resulted from the original sampling frame of Canada Post survey respondents, which only represented 15%–18% of the population. Priorities and perceptions of care could reasonably be different for less well-educated or sicker women, women who are not interested or capable of answering surveys, or those who are bed-bound or living in institutions. A second limitation is that recall bias may have led to an underestimation of women's perceptions of the care they received, especially because a response option of “I do not remember” was not offered. Cognitive impairment was not measured among the respondents, although it is unlikely that women with such impairments would have been able to complete and return the questionnaire. Even among people with intact cognition, important differences often exist between care advised or delivered and care that is recollected or followed.22,23 Furthermore, certain clinical screening strategies, such as observing gait and balance during an assessment of fall risk and informally testing a patient's memory, may not be fully appreciated by older women.
The decreases in frequency with increasing age that were observed for certain health priorities in the WOW study may have been due to shifting health concerns as part of the normal aging process for women or to secular trends in health concerns more prevalent among members of the younger “baby-boomer” generation. The differences in perceptions of care between different age groups may have been due to differences in recall among younger and older women. Actual variations in care is another possibility. Low but uniform rates of recall about addressing memory loss may have resulted from unclear recommendations to physicians about the benefits of screening for cognitive dysfunction among elderly people without functional impairment.24 Despite current recommendations for screening, memory problems ranked at the top of the list of health priorities for women of all ages. Screening might be reconsidered, with the aim of reassuring older women when cognitive dysfunction does not exist.
Provincial variations in the respondents' perceptions of the delivery of care must also be interpreted cautiously. The WOW study was not designed to measure a priori such perceptions in different provinces. Nonetheless, for a statistically significant number of health priorities, the Atlantic provinces were ranked last in terms of the proportion of respondents who perceived that care was being delivered to address them. Results of our study can be used as incentive to investigate whether perceptions mirror actual deficiencies in care for these priorities in the Atlantic provinces compared with other Canadian provinces.
Conclusions about patient-centred care being delivered in concordance with the majority of women's health priorities must be viewed in light of the cross-sectional nature of this survey. For example, women who reported being greatly concerned about osteoporosis were 2.6 times more likely than those who were not greatly concerned about it to perceive that their physicians screened them for this condition. Do women first express concern about osteoporosis and then their physician sends them for bone mineral density testing, or is the importance of preventing and treating osteoporosis only recognized by women after undergoing screening? The former presupposes that women have the power to direct the health agenda and that imparting knowledge to older women may lead to improved screening rates for certain conditions. The latter suggests that physicians should continue to be targeted for education campaigns about the importance of health promotion and disease prevention among their elderly female patients.
In conclusion, older women have many health priorities, and if their perceptions are correct, it appears that health care providers are addressing many, but not all, of their health concerns. Further research is needed to test whether addressing older women's health priorities results in measurable improvements in their health outcomes.
β See related article page 165
Supplementary Material
Acknowledgments
This study was supported by an operating grant from the Canadian Institutes of Health Research. Cara Tannenbaum is a junior Fonds de la recherche en santé (FRSQ) chercheur-boursier award recipient. Nancy Mayo and Francine Ducharme are senior FRSQ chercheur-boursier award recipients.
Footnotes
This article has been peer reviewed.
Contributors: Cara Tannenbaum conceptualized the project, developed the questionnaire, conducted the study, analyzed the results and wrote the manuscript. Nancy Mayo was responsible for developing the methodology, guiding the analyses and revising the original manuscript. Francine Ducharme was involved in the development of the protocol and theoretical framework for the study and reviewed the final draft of the manuscript. All of the authors approved the final version to be published.
Competing interests: None declared.
Correspondence to: Dr. Cara Tannenbaum, Centre de recherche, Institut universitaire de gériatrie de Montréal, 4565 Queen Mary Rd., Montréal QC H3W 1W5; fax 514 340-3540; cara.tannenbaum@umontreal.ca
References
- 1.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469-75. [DOI] [PubMed]
- 2.Tinetti ME, Fried T. The end of the disease era. Am J Med 2004;116:179-85. [DOI] [PubMed]
- 3.Stewart M, Brown J, Weston W, McWinney I, McWilliam C, Freeman T. Patient-centred medicine: transforming the clinical method. London: Sage; 1995.
- 4.Phelan EA, Anderson LA, LaCroix AZ, Larson EB. Older adults' views of “successful aging” — How do they compare with researchers' definitions? J Am Geriatr Soc 2004;52:211-6. [DOI] [PubMed]
- 5.Tannenbaum CB, Nasmith L, Mayo N. Understanding older women's health care concerns: a qualitative study. J Women Aging 2003;15:103-16. [DOI] [PubMed]
- 6.Tannenbaum C, Mayo N. Women's health priorities and perceptions of care: a survey to identify opportunities for improving preventative health care delivery for older women. Age Ageing 2003;32:626-35. [DOI] [PubMed]
- 7.World Health Organization. International classification of functioning, disability and health. Beginner's guide. Geneva: The Organization; 2002.
- 8.Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. Ottawa: Canada Communication Group-Publishing; 1994. Cat no H21-117/1994E.
- 9.US Preventive Services Task Force. Guide to clinical preventive services. 2nd ed. Baltimore: Williams & Wilkins; 1996.
- 10.Goldberg TH, Chavin SI. Preventive medicine and screening in older adults. J Am Geriatr Soc 1997;45:344-54. [DOI] [PubMed]
- 11.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. [DOI] [PubMed]
- 12.Hopman WM, Towheed T, Anastasssiades T, Tenenhouse A, Poliquin S, Berger C, et al; Canadian Multicentre Osteoporosis Study Research Group. Canadian normative data for the SF-36 health survey. CMAJ 2000;163(3):265-71. [PMC free article] [PubMed]
- 13.Profile by age and sex for Canada, provinces, and territories, 2001 census. Ottawa: Statistics Canada. Cat no 95F0486XCB01000.
- 14.Marital status by age and sex group for Canada, provinces, and territories, 2001 census. Ottawa: Statistics Canada. Cat no 95F0407XCB01004
- 15.Living arrangements, age groups and sex for private households in Canada, provinces, and territories, 2001 census. Ottawa: Statistics Canada. Cat no 95F0315XCB01004.
- 16.Highest educational attainment, diplomas and certificates by age group and sex for population 15 years and older, for Canada, provinces, and territories, 2001 census. Ottawa: Statistics Canada. Cat no 95F0419XCB01005.
- 17.Income by age group and sex for population 15 years and older, for Canada, provinces, and territories, 2001 census. Ottawa: Statistics Canada. Cat no 95F0431XCB01005.
- 18.Canadian Institute for Health Information. Health indicators. Ottawa: The Institute: 2002. Cat no 82-221-XIE.
- 19.Laurier C, Moride Y, Kennedy WA. Health survey data on potentially inappropriate geriatric drug use. Ann Pharmacother 2002;36:404-9. [DOI] [PubMed]
- 20.Picavet HS. National health surveys by mail or home interview: effects on response. J Epidemiol Community Health 2001;55:408-13. [DOI] [PMC free article] [PubMed]
- 21.Mallinson S. The Short-Form 36 and older people: some problems encountered when using postal administration. J Epidemiol Community Health 1998;52:324-8. [DOI] [PMC free article] [PubMed]
- 22.Madlensky L, McLaughlin J, Goel V. A comparison of self-reported colorectal cancer screening with medical records. Cancer Epidemiol Biomarkers Prev 2003;12:656-9. [PubMed]
- 23.Beaulieu MD, Beland F, Roy D, Falardeau M, Hebert G. Factors determining compliance with screening mammography. CMAJ 1996;154(9):1335-43. [PMC free article] [PubMed]
- 24.Patterson CJ, Gass DA. Screening for cognitive impairment and dementia in the elderly. Can J Neurol Sci 2001;28:S42-51. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


