Abstract
Background
Colorectal cancer (CRC) has become a significant global concern, presenting formidable challenges to healthcare systems and leading to substantial healthcare expenses. This study examines the projected prevalence and trends of CRC worldwide, encompassing 21 regions and 195 nations.
Methods
We employed an illness-death model (IDM) in order to forecast the anticipated prevalence of CRC by the year 2040. To accomplish this, we utilized data retrieved from the Global Health Data Exchange (GHDx) query tool spanning from 1990 to 2021. The primary objective of this study is to furnish sex-specific estimations encompassing various geographical regions.
Results
By 2040, the global age-standardized prevalence rate (ASPR) of CRC among the total population is projected to rise, reaching 145.82 per 100,000, which reflects an increase of 8.15%. East Asia is forecasted to have the highest ASPR at 330.17 per 100,000, representing a substantial rise of 94.81%. Notably, the most rapid percentage increase is projected in Andean Latin America, with an anticipated rise of 106.2%. In contrast, many countries, particularly in developed nations, are expected to see a decline in ASPR during this period. The United Arab Emirates is projected to experience the most significant decrease in ASPR, at -86.51%, while Mauritius is anticipated to have the largest increase in CRC prevalence rate, at 226.26%. Globally and regionally, the ASPR among males is expected to remain higher than that among females over the next 21 years.
Conclusions
The global prevalence of CRC is increasing, particularly in developing countries, while developed countries are anticipated to observe a declining trend. This highlights the significance of appropriately allocating resources and implementing effective preventive measures, especially in developing nations.
Supplementary Information
The online version contains supplementary material available at 10.1007/s44197-025-00348-3.
Keywords: Age-standardized prevalence, Cancer epidemiology, Colorectal cancer, Illness-death model
Introduction
Colorectal cancer (CRC) presents a pressing global health challenge, given its alarming rates of occurrence and mortality. Based on data from the Global Burden of Disease (GBD) study, it was estimated that in 2020, there were more than 1.9 million new cases of CRC reported worldwide, with approximately 930,000 deaths reported as a direct result of the disease [1]. Consequently, CRC ranks as the third most prevalent cancer globally and stands as one of the primary contributors to cancer-related fatalities [2, 3]. It is anticipated that the burden of CRC will rise significantly worldwide, reaching an estimated 3.2 million new cases and 1.6 million deaths by 2040, with this increase expected to be particularly prominent in countries with a high or very high Human Development Index (HDI) [1]. However, the global incidence of CRC displays significant variability shaped by factors such as geographical location, gender, age, and socioeconomic status. In certain regions, Europe, encompassing nations like the Netherlands, Norway, Slovakia, and Hungary, emerges with the most substantial incidence rates. Nevertheless, it is crucial to highlight that Asia, as one of the most densely populated continents globally, continues to shoulder the heaviest burden of this disease [4–6].
The increase in the prevalence and overall incidence of CRC reflects the strong influence of lifestyle factors such as obesity, smoking, sedentary lifestyle, and changing reproductive patterns associated with urbanization, as well as the aging of the population worldwide [7]. In addition, variations in the genetic background between different populations are thought to be associated with the development of CRC [8]. Knowledge of the prevalence of the disease and the percentage of increase predicted for it in the coming years by adequately qualified researchers may encourage participation in risk-reduction behaviors, including participation in screening programs and lifestyle changes to reduce the incidence of the disease. Conversely, numerous medium-income and low-income countries have experienced a significant upward trajectory in the incidence and prevalence of CRC [4]. Hence, it is crucial to have a comprehensive understanding of the epidemiological attributes of CRC, such as its temporal trends and geographical distribution worldwide, to effectively manage and prevent this disease on a global scale.
In the present study, we projected the age-standardized prevalence rate (ASPR) of CRC on a global, regional, and national scale, analyzing its trends from 1990 to 2040. The research offers significant insights into the evaluation of current prevention strategies, the advancement of knowledge, and targeted planning in countries expected to face a higher prevalence of CRC in the future.
Materials and Methods
Source of Data
To predict the prevalence of CRC by 2040, we utilized the illness-death model (IDM), a multistate model in epidemiology for analyzing chronic diseases [9, 10]. The Global Health Data Exchange (GHDx) query tool at the Institute for Health Metrics and Evaluation (IHME) provided us with the necessary data extracted from the GBD 2021.
This included age-standardized all-cause and specific mortality rates (ASMR) for both genders at the global, regional, and national levels spanning from 1990 to 2021. Population data, crucial for our model, was obtained from freely accessible GHDx query tools available at https://vizhub.healthdata.org/population-forecast/.
Modeling
We employed the IDM, a dynamic model based on ordinary differential equations (ODEs), to capture the various states of health individuals experience over time, including gender-specific variations. Two specific ODEs were utilized to establish the relationship between epidemiological indices, enabling us to estimate disease prevalence for the projected period from 2021 to 2040 [11, 12]:
The data retrieved from the GBD database spanning from 1990 to 2040 was utilized to calibrate the model and generate predictions for different geographical units. In line with the study conducted by Ito et al. [13], our aim was to offer estimates of CRC prevalence up to 2040 at the global, regional, and national levels across 216 countries, taking into consideration the availability of population data.
Projection
Our investigation focused on three distinct states: susceptible individuals, individuals impacted by CRC, and death (an absorbing state). These states delineate three potential pathways: i. the shift from the susceptible state to the illness state, ii. the progression from the illness state to the death state, and iii. a direct transition from the susceptible state to the death state at a specific time point. To facilitate our analysis, we intend to furnish annual projected data for each geographic unit up to the year 2040. All statistical analyses were carried out using the R software packages.
Results
Global Prevalence of CRC
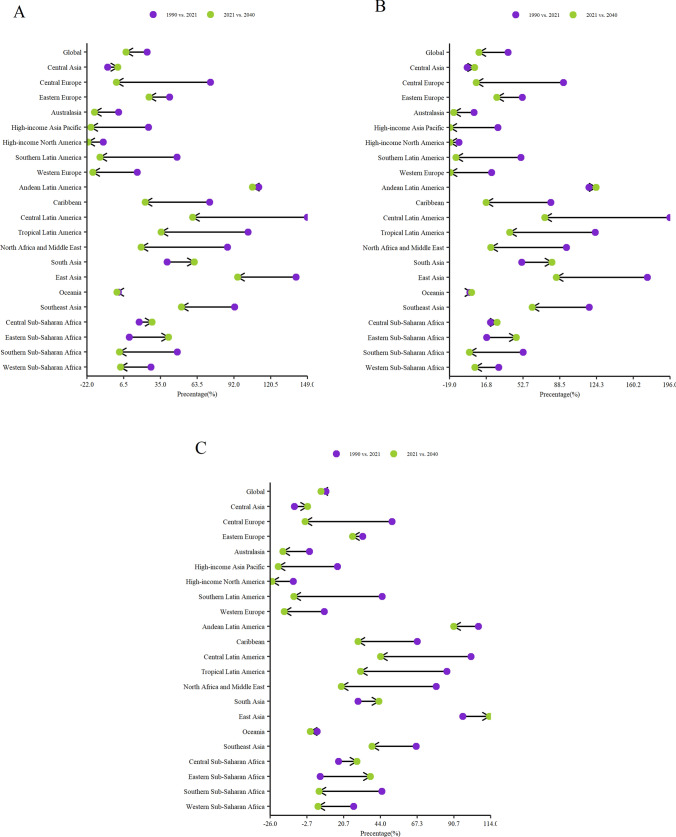
Figure 1 displays the observed and predicted global trends in CRC rates spanning from 1990 to 2040. The data reveals a consistent escalation in the ASPR of CRC for both genders on a worldwide scale, with a substantial 24.56% surge observed between 1990 and 2021. Notably, this rise is more pronounced among males, reflecting a percentage increase of 38.01%, in contrast to females at 6.15%. Projections indicate the continuation of this upward trajectory, forecasting an anticipated ASPR of 145.82 (95% CI, 141.16–150.66) per 100,000 individuals by 2040. This signifies an 8.15% upswing compared to the rates documented in 2021, as detailed in Table 1 and depicted in Fig. 2. Furthermore, males are expected to encounter a higher surge (9.55%) in contrast to females (6.15%). Consequently, the projected ASPR for 2040 anticipates rates of 181.98 (95% CI, 176.6–18) per 100,000 for males and 113.73 (95% CI, 109.3–118.35) per 100,000 for females. However, a noteworthy shift becomes apparent in the percentage changes from 2020 to 2040, revealing a decline in the rate of increase among males while females exhibit a heightened rate. In essence, the projections indicate that the ASPR of CRC is set to escalate more rapidly among females compared to males over the specified period.
Fig. 1.
The global ASPR of CRC trend from 1990 to 2040. The dashed line represents the observed trend from 1990 to 2021 and the halo effect represents the projected trend from 2021 to 2040
Table 1.
Global and regional projected ASPR of CRC per 100,000 of total population in 2022, 2025, 2030, 2035, and 2040, as well as its percentage changes from 1990 to 2021 and from 2021 to 2040
| Region | ASPR per 100 000 (95% CI) | Percentage change | |||||
|---|---|---|---|---|---|---|---|
| 2022 | 2025 | 2030 | 2035 | 2040 | 1990 VS. 2021 | 2021 VS. 2040 | |
| Global | 135.9 (135.07–136.75) | 137.51 (136.09–138.95) | 140.23 (137.77–142.74) | 143 (139.45–146.64) | 145.82 (141.16–150.66) | 24.56 | 8.15 |
| Central Asia | 44.62 (44.58–44.68) | 44.74 (44.62–44.87) | 44.94 (44.69–45.2) | 45.14 (44.76–45.53) | 45.34 (44.84–45.87) | − 6.04 | 1.69 |
| Central Europe | 183.18 (183.11–183.33) | 183.41(183.17–183.72) | 183.79 (183.26–184.38) | 184.17 (183.36–185.05) | 184.55 (183.45–185.72) | 73.79 | 0.77 |
| Eastern Europe | 152.43 (152.22–152.69) | 158.08 (157.48–158.74) | 167.98 (166.66–169.38) | 178.5 (176.37–180.73) | 189.68 (186.64–192.84) | 41.93 | 25.94 |
| Australasia | 273.36 (273.22–273.63) | 265.75 (265.31–266.32) | 253.54 (252.62–254.58) | 253.54 (252.62–254.58) | 230.78 (229.02–232.63) | 2.45 | −16.36 |
| High-income Asia Pacific | 277.72 (273.36–282.16) | 268.95 (261.87–276.23) | 254.94 (243.6–266.81) | 241.66 (226.56–257.77) | 229.07 (210.69–249.05) | 25.58 | −19 |
| High-income North America | 237.04 (232.41–241.77) | 228.65 (221.18–236.39) | 215.33 (203.46–227.89) | 202.78 (187.11–219.76) | 190.96 (172.07–211.93) | − 9.59 | −21.37 |
| Southern Latin America | 127.8 (124.89–130.79) | 124.69 (119.94–129.64) | 119.68 (112–127.89) | 114.86 (104.56–126.19) | 110.24 (97.6–124.53) | 47.84 | −12.12 |
| Western Europe | 245.36 (240.75–250.06) | 237.61 (230.15–245.33) | 225.24 (213.31–237.85) | 213.52 (197.66–230.66) | 213.52 (197.66–230.66) | 16.98 | −17.56 |
| Andean Latin America | 81.01 (77.26–84.95) | 90.15 (83.24–97.65) | 107.75 (94.05–123.46) | 128.78 (106.18–156.19) | 153.91 (119.86–197.64) | 111.23 | 106.2 |
| Caribbean | 172.9 (169.86–176) | 178.25 (173–183.66) | 187.52 (178.21–197.33) | 197.28 (183.53–212.08) | 207.55 (188.99–227.94) | 73.1 | 22.97 |
| Central Latin America | 83.38 (81.89–84.92) | 89.77 (87.07–92.56) | 101.52 (96.36–106.95) | 114.8 (106.62–123.61) | 129.82 (117.97–142.88) | 148.81 | 59.95 |
| Tropical Latin America | 75.56 (74.55–76.59) | 79.18 (77.4–81.01) | 85.61 (82.35–89) | 92.55 (87.6–97.79) | 100.06 (93.18–107.47) | 102.77 | 35.36 |
| North Africa and the Middle East | 76.6 (76–77.22) | 78.75 (77.7–79.83) | 82.47 (80.61–84.39) | 86.37 (83.61–89.23) | 90.45 (86.72–94.35) | 86.87 | 19.76 |
| South Asia | 20.54 (20.26–20.83) | 22.08 (21.58–22.61) | 24.92 (23.95–25.93) | 28.11 (26.57–29.75) | 31.72 (29.48–34.14) | 40.15 | 61.08 |
| East Asia | 177.5 (175.11–179.92) | 196.84 (192.4–201.39) | 233.88 (224.95–243.17) | 277.88 (262.95–293.67) | 330.17 (307.36–354.68) | 140.13 | 94.81 |
| Oceania | 21.56 (21.55–21.57) | 21.6 (21.58–21.63) | 21.67 (21.63–21.72) | 21.74 (21.68–21.81) | 21.81 (21.73–21.91) | 2.2 | 1.24 |
| Southeast Asia | 73.69 (73.01–74.38) | 78.53 (77.31–79.78) | 87.31 (85.01–89.69) | 97.08 (93.47–100.85) | 107.95 (102.77–113.4) | 92.48 | 51.21 |
| Central Sub-Saharan Africa | 23.17 (22.97–23.38) | 24.11 (23.76–24.47) | 25.75 (25.11–26.42) | 27.51 (26.54–28.52) | 29.39 (28.06–30.79) | 18.29 | 28.38 |
| Eastern Sub-Saharan Africa | 32.32 (32.09–32.56) | 34.1 (33.69–34.52) | 37.29 (36.53–38.07) | 40.77 (39.59–41.99) | 44.58 (42.92–46.31) | 10.75 | 41.21 |
| Southern Sub-Saharan Africa | 42.72 (42.69–42.75) | 42.92 (42.85–43) | 43.27 (43.12–43.43) | 43.61 (43.38–43.86) | 43.96 (43.65–44.29) | 48.05 | 3.08 |
| Western Sub-Saharan Africa | 17.29 (17.14–17.45) | 17.4 (17.15–17.67) | 17.59 (17.16–18.05) | 17.79 (17.16–18.44) | 17.98 (17.17–18.85) | 27.58 | 3.79 |
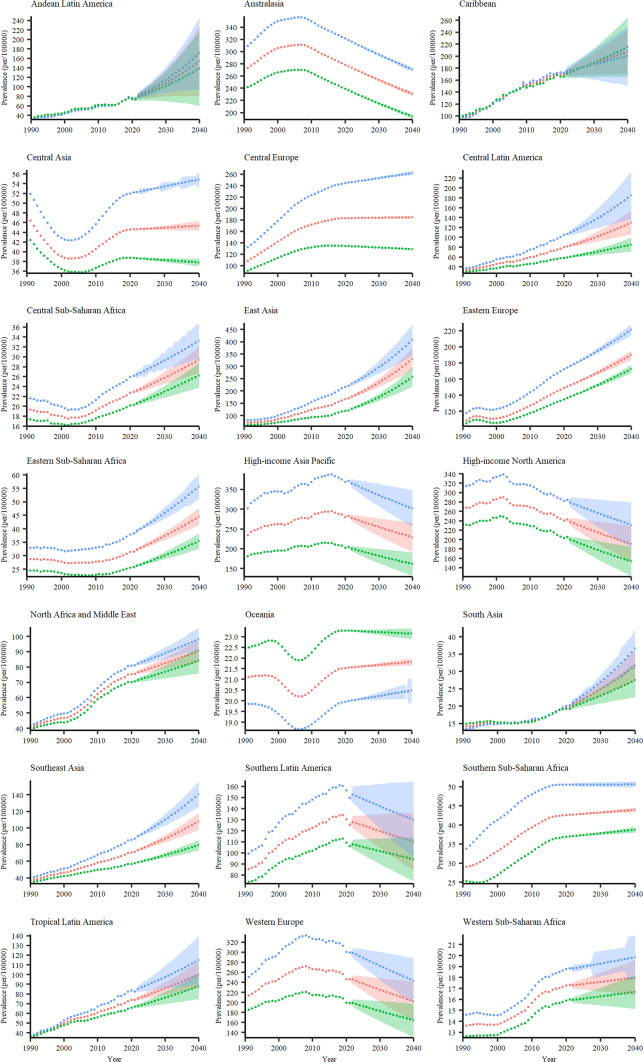
Fig. 2.
Lollipop plots depicting the global and regional percentage changes in ASPR of CRC per 100,000 population from 1990 to 2021, along with projected changes from 2021 to 2040, for the both sexes (A), males (B), and females (C)
Regional Prevalence of CRC in the Total Population
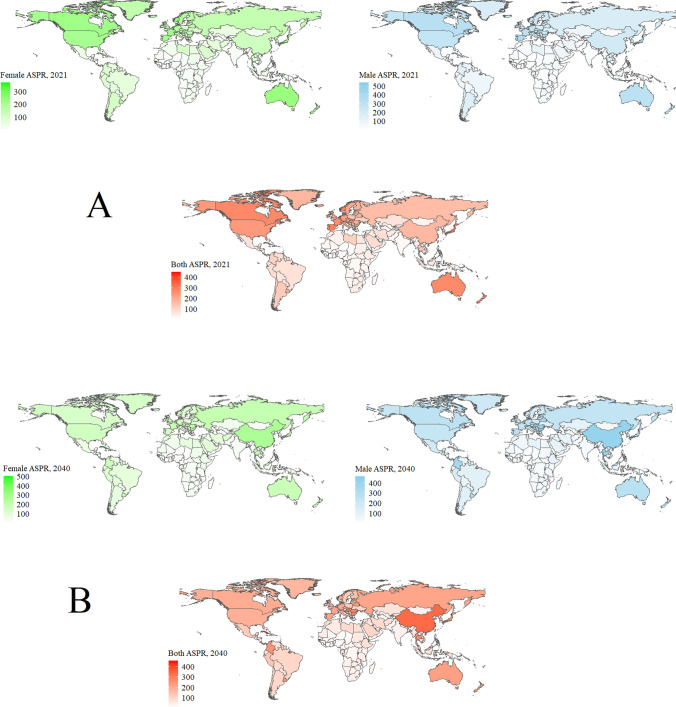
Table 1 and Figs. 2 and 3 offer a comprehensive overview of the projected ASPR of CRC and their corresponding percentage changes across 21 GBD regions up to 2040. Notably, East Asia stands out with the highest ASPR for both genders, expected to reach 330.17 (95% CI, 307.36–354.68) per 100,000 individuals by 2040, indicating a substantial 94.81% increase from 2021 to 2040. Following East Asia, Australasia is projected at 230.78 (95% CI, 229.02–232.63) per 100,000, and High-income Asia Pacific at 299.07 (95% CI, 210.69–249.05) per 100,000. However, these regions are anticipated to experience declines of -16.36% and -19% during the same time period, respectively. In contrast, Western Sub-Saharan Africa is anticipated to exhibit the lowest projected ASPR of 17.98 (95% CI, 17.17–18.85) per 100,000 in 2040, reflecting a modest increase of 3.79%. Following this trend, Central Sub-Saharan Africa and South Asia are forecasted to have comparatively low ASPR rates for both genders by 2040, standing at 29.39 (95% CI, 28.06–30.79) and 31.72 (95% CI, 29.48–34.14) per 100,000, respectively. However, despite their current lower rates, these regions are projected to experience substantial increases in their ASPR rates by 28.4% and 61% in 2040 compared to 2021.
Fig. 3.
The regional forecast of CRC prevalence per 100,000 individuals is depicted for males (blue lines), females (green lines), and both sexes (red lines). The halo effect illustrated in each scatter plot effectively captures projections spanning from 2021 to 2040, with 95% confidence intervals
Between 1990 and 2021, High-income North America and Central Asia were the sole regions where a decrease in CRC ASPR was observed, showing rates of -9.59 and -6.04 decline respectively. Analyzing the periods spanning 1990 to 2021 and 2021 to 2040, a notable trend emerges: ASPRs have decreased across all regions, with exceptions noted in Eastern Sub-Saharan Africa, Western Sub-Saharan Africa, Eastern Sub-Saharan Africa, and Central Asia (Table 1 and Fig. 2A). This trend indicates that while ASPRs are on the rise, the pace of this increase is projected to decelerate compared to historical trends.
Gender-Based Regional Prevalence of CRC
In general, a higher ASPR of CRC is expected among males compared to females across most regions, except for the Caribbean and Oceania where females exhibit a higher ASPR of CRC. Among the male population, East Asia exhibits the highest ASPR of CRC at 407.87 (95% CI, 375.95–443) per 100,000, experiencing a significant 85% increase from 2021 to 2040. However, Western Sub-Saharan Africa represents the region with the lowest ASPR among males, standing at 19.84 (95% CI, 18.92–21) per 100,000. Nonetheless, it is expected to witness a 5.44% increase in 2040 compared to 2021. Notably, analyzing the periods from 1990 to 2021 and 2021 to 2040 reveals an overall decrease in ASPRs across most regions, with exceptions observed in Central Asia, Andean Latin America, South Asia, Oceania, Central Sub-Saharan Africa, and Eastern Sub-Saharan Africa (Figs. 2B, 3, and Supplementary Data 3).
By 2040, East Asia is projected to have the highest female ASPR, estimated at 257.51 (95% CI, 237.53–279.19) per 100,000 individuals, representing a substantial 113.19% increase from 2021 to 2040. Conversely, Western Sub-Saharan Africa is anticipated to have the lowest CRC ASPR among females, with an ASPR of 16.68 (95% CI, 15.9–17.5) per 100,000 individuals, showing a 4.24% increase from 2021 to 2040 (Figs. 2C, 3, and Supplementary Data 4).
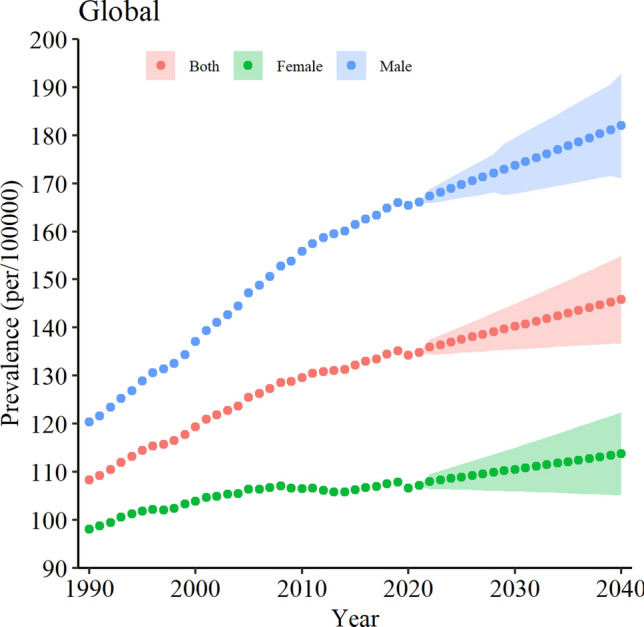
National Prevalence of CRC
Figure 4, Supplementary Data 1, and Supplementary Data 2 present the ASPRs of CRC in various countries in 2021, alongside their projected values for 2040. Specifically, Cuba (456.16 [95% CI, 389.67–534.02]), Bermuda (384.63 [95% CI, 378.44–391.21]), and China (337.81 [95% CI, 314.08–363.35]) are anticipated to exhibit the highest ASPRs per 100,000 individuals for both sexes in 2040, with increases of 79.9%, 5.81%, and 100.34%, respectively. In contrast, Mozambique (10.22 [95% CI, 10.19–10.26]), the United Arab Emirates (11.96 [95% CI, 11.68–12.26]), and the Gambia (13.19 [95% CI, 12.91–13.48]) are expected to have the lowest ASPRs per 100,000 individuals (see Supplementary Data). Importantly, among these countries, Gambia will encounter a 33.85% increase in the CRC ASPR, Mozambique will experience a slight increase of 0.7%, while the United Arab Emirates is projected to face a substantial decrease of -86.51% in 2040.
Fig. 4.
The ASPR per 100,000 of CRC for females (green maps), males (blue maps), and both sexes (red maps) in 195 nations. Panel A represents the observed ASPR of CRC in 2021, while Panel B showcases the projected ASPR of CRC in 2040
Moreover, spanning the period from 2021 to 2040, out of 194 nations, 129 countries are anticipated to exhibit an ascending trend in ASPRs for both sexes. Remarkably, four countries are predicted to undergo a growth rate surpassing 100%, including China (100.34%), Thailand (115.22%), Colombia (129.79%), and Mauritius (226.26%). Conversely, 58 nations are poised to witness a declining trend, with the most significant decreases expected in the United Arab Emirates ( − 86.51%), Andorra ( − 63.35%), Luxembourg ( − 48.23%), United States Virgin Islands ( − 47.78%), and the Netherlands ( − 46.66%) by 2040.
Interestingly, in comparison to the 1990–2021 timeframe, a greater number of nations appear to be demonstrating a downward trajectory in ASPRs between 2021 and 2040, hinting at a relative amelioration in the scenario. Noteworthy is that only Austria, Belgium, the United States of America, New Zealand, Ukraine, and Germany are projected to sustain their diminishing trends observed from 1990 to 2021 into the following two decades, with rates of − 31.28%, − 30.31%, − 20.6%, − 11.91%, − 10.33%, and − 9.4%, respectively, by 2040.
Paradoxically, although Taiwan is foreseen to uphold its status as the country with the highest CRC prevalence until 2040, the corresponding percentage change is expected to markedly decrease, approximately 65-fold, from 130% in the 1990–2021 period to 2% in the 2021–2040 timeframe. Additionally, among nations that experienced ASPR growth exceeding 100% between 1990 and 2021, only Belize, Nicaragua, Chile, and the Republic of Korea are estimated to showcase negative growth in CRC ASPR by 2040, with rates of -11.35%, -12.73%, -3.08%, and -9.92%, respectively (see Supplementary Data).
Gender-Based National Prevalence of CRC
In 2021, among the 195 nations studied, only 20 countries exhibited a higher prevalence of CRC in females compared to males. By 2040, this figure is estimated to increase to 26 nations, with a notable observation that approximately 35% of these countries are situated in Arabian and/or Middle Eastern regions. In the rest of the world, the projected trend indicates that the ASPR of CRC will be higher in males compared to females by 2040.
Among males, Mauritius (464.18 [95% CI, 300.46–717]), Taiwan (439.49 [95% CI, 325.93–593]), and Estonia (419.81 [95% CI, 413.5–427]) are set to exhibit the highest ASPRs of CRC at 407.87 (95% CI, 375.95–443) per 100,000, marking a significant 85% increase from 2021 to 2040. Conversely, the United Arab Emirates (6.9 [95% CI, 6.69–7]), Mozambique (11.62 [95% CI, 11.59–12]), and Gambia (14.26 [95% CI, 13.93–14.63]) represent the regions with the lowest ASPRs among males per 100,000 (see Supplementary Data 3).
For females in 2040, Cuba (503.11 [95% CI, 414.71–610.37]), Bermuda (304.52 [95% CI, 300.95–308.28]), and China (266.88 [95% CI, 245.56–290.07]) are anticipated to display the highest ASPRs per 100,000 individuals. Conversely, Mozambique (9.16 [95% CI, 9.13–9.2]), Guinea (11.41 [95% CI, 10.96–11.89]), and Côte d'Ivoire (14.01 [95% CI, 13.89–14.14]) are expected to have the lowest ASPRs among females (see Supplementary Data 4).
Notably, the most notable increases in ASPR among both males and females in 2040 compared to 2021 are projected to transpire in Mauritius, with an increased rate of 297.84% and 143.14%, respectively (see Supplementary Data). Conversely, the United Arab Emirates is anticipated to witness the most substantial reduction in ASPR ( − 87.5%) among males, while Andorra is forecasted to experience the highest reduction ( − 64.74%) among females by 2040, followed by the United Arab Emirates ( − 63.25%).
Discussion
The research offers significant insights for evaluating the current landscape of colorectal cancer (CRC), enhancing knowledge, and contributing to efforts aimed at reducing the disease burden. Additionally, it supports the advancement of healthcare systems to effectively address the future challenges posed by CRC at global, regional, and national levels by 2040. Despite notable variations at regional and national levels, the overall ASPR of CRC is on the rise worldwide. Between 1990 and 2021, the ASPR of CRC has more than doubled for both males and females in 31 countries. However, this upward trend is anticipated to decline, affecting 5 nations in the next 19 years. While this observed decline may initially seem promising, it highlights significant concerns for specific countries such as China, Thailand, Colombia, and Mauritius, where the ASPR of CRC is forecasted to surge by more than 100% over the upcoming two decades. Notably, Mauritius stands out as the sole nation where the ASPR of CRC is expected to exhibit an upward trajectory, with a projected increase from 150.78% in the period spanning 1990 to 2021 to 226.26% in the timeframe from 2021 to 2040.
From 1990 to 2021, a global surge of 24.56% in the ASPR of CRC was observed across both genders. Nevertheless, this trend is anticipated to persist but at a slower pace until 2040, with an estimated 8.15% increase, notably concentrated in Asia. Andean Latin America, East Asia, and South Asia are expected to see significant rises of 106.2%, 94.81%, and 61.08% respectively. These increases can be attributed to the rapid socio-economic growth, industrialization, and the adoption of unhealthy Western lifestyles in developing regions. This lifestyle is characterized by unhealthy dietary habits, substance abuse (such as smoking and alcohol consumption), decreased physical activity, and sedentary behavior [14, 15]. Furthermore, advancements in healthcare systems and disease screening have led to higher detection rates of CRC in various regions [16]. Significantly, when contrasting the percentage shifts in age-standardized CRC rates between the preceding two decades and the forthcoming two decades, a discernible pattern emerges. While global and most regional rates are projected to rise from 2021 to 2040, a decline in CRC rates is foreseen in High-income North America, High-income Asia Pacific, Western Europe, Australasia, Southern Latin America, and Central Europe.
Africa has historically been characterized by a low prevalence of CRC [17]. However, recent observations suggest an uptick in CRC prevalence in several African regions, excluding Eastern Sub-Saharan Africa. This specific region is predicted to experience a rising trend over the forthcoming 21 years (41.21%) compared to the prior two decades (10.75%). Tackling CRC in Africa faces significant challenges, primarily due to the absence of comprehensive health insurance systems in most African nations, which restrict access to affordable care. Sub-Saharan Africa, housing about two-thirds of the global impoverished population, encounters particular hardships. The high expenses associated with screening procedures, often entirely shouldered by individuals, render screening initiatives unfeasible for many. Moreover, prompt cancer diagnosis and treatment services remain scant across Sub-Saharan Africa. Consequently, previous data collection systems might not fully capture the true incidence and subsequently prevalence of the disease in these regions. This situation underscores the imperative to bolster the quality of life, encompassing healthcare services, and consider the potential impact of international technological advancements on predictive models. Enhancing healthcare services demands accurate and reliable data on the burden of CRC, emphasizing a critical need for policymakers to prioritize advancements in data collection and analysis methodologies to better understand and address the evolving landscape of CRC in Africa [18, 19].
In several developed nations including Europe, North America, and some Asian countries, the burden of CRC is either decreasing or remaining stable [5, 20]. This notable shift can be predominantly attributed to the successful implementation of screening programs and the adoption of healthier lifestyles [21]. Screening programs play a crucial role in the early detection of precancerous lesions and facilitate the removal of adenomas through endoscopic procedures. This, in turn, contributes to a reduction in the incidence and mortality of CRC. While population-based screenings may initially lead to a temporary increase in incidence, they ultimately contribute to a long-term decrease in CRC cases [22]. A prime example is the United States, where CRC screening programs were implemented in 1997. Over time, the participation rate among individuals has increased from 38% in 2000 to 66% in 2018 [23, 24]. Consequently, the ASPR of CRC among both sexes has shown a notable decline of − 9.54% from 2000 to 2018, underscoring the sustained impact of screening efforts. In our study, the United Arab Emirates exhibited a similar trend regarding the prevalence of CRC. From 1990 to 2021, there was a consistent increasing trend of 9.01% in CRC prevalence. However, our projections indicate a substantial shift towards a significant decrease of -86.51% over the next two decades, specifically by 2040.
The management of CRC in high-income countries appears promising, except for China, are projected to have a decreasing trend by 2040. The World Health Organization (WHO) emphasizes that successful cancer treatment relies on timely and accurate diagnosis, as well as access to appropriate treatments. The increasing incidence of cancer in low- and middle-income countries highlights the existing shortcomings in healthcare, including inadequate health services, limited screening programs, and a weakened economic infrastructure [25]. This agreement has successfully streamlined treatment and follow-up protocols, leading to an overall improvement in prognosis [26]. Consequently, low- and lower-middle-income countries with limited resources for diagnosis and treatment can potentially improve the epidemiological outlook for CRC through similar health cooperation agreements.
In 2040, China is projected to have the fourth highest ASPR of CRC in the general population and and the second highest among females. Abu Hassan and colleagues have shown that the overall age-standardized incidence rate of CRC is higher among individuals of Chinese ethnicity compared to other East Asian ethnicities [27]. A similar study conducted on the Singaporean population also indicated a higher age-standardized incidence rate among individuals of Chinese ethnicity compared to Malays and Indians. These findings suggest that genetic factors may play a crucial role in the etiology of CRC.
The global prevalence of CRC among males was roughly equal to that among females in 2021. However, this disparity is projected to rise, with males expected to have a prevalence that is 1.6 times higher than that of females by 2040. Several factors contribute to this gender disparity in CRC prevalence. Firstly, males have higher rates of risk factors such as smoking, alcohol consumption, elevated fasting glucose levels, and higher body mass index, particularly visceral fat, which contribute to higher overall CRC prevalence in males [28]. Dietary habits also play a role, with males having a higher inclination towards meat consumption, while females tend to consume more vegetables, potentially contributing to the gender disparity in CRC prevalence [29]. Studies suggest that endogenous estrogen and oral contraceptive use may have a protective effect against CRC in females [30, 31]. However, it is important to note that the prevalence of CRC among females globally is projected to increase at a faster rate in the next 21 years compared to the previous decades, possibly due to changing risk factors like increasing smoking rates and consumption of low-fiber diets among females [3]. In 2040, South Asia and the Caribbean are projected to be the only regions where ASPR of CRC is higher in females than in males. This distinct gender pattern may be influenced by a combination of genetic factors and lifestyle choices. A study conducted in 2016 revealed that South Asian women had higher levels of physical inactivity, making it one of the regions with the highest rates of sedentary behavior among females [32]. It is crucial to acknowledge that this lack of physical activity can contribute to an increased risk of developing CRC.
Conclusion
In summary, our study reveals significant disparities in the prevalence of CRC across different regions and nations when adjusted for age. It is concerning that, despite notable trends of decreasing CRC cases in various parts of the world, the global prevalence is projected to increase by 8% over the next two decades, reaching approximately 145.82 cases per 100,000 population. To effectively address this global concern, a comprehensive approach is essential. This approach should include multifaceted strategies that promote lifestyle modifications, particularly dietary changes, alongside proactive screening efforts targeted at high-risk individuals. Ensuring equitable access to quality healthcare and advancements in treatment options are also crucial for the effective management of CRC. Recognizing the significant impact of lifestyle choices on CRC development, fostering collaboration among diverse community organizations is vital, extending beyond the involvement of healthcare policymakers alone. By combining our efforts and resources, we can actively work to reduce the burden of CRC and improve global health outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our sincere gratitude to the research experts and the Directorate of the Research and Technology Department at Qom University of Medical Sciences for their invaluable contributions to this project. We also extend our heartfelt appreciation to the esteemed members of the Research Institute for Gastroenterology and Liver Diseases at Shahid Beheshti University of Medical Sciences in Tehran, Iran. Special thanks are due to Professor Mohammad Reza Zali for his steadfast support throughout this endeavor.
Author Contributions
MO and HH have made significant contributions to the conception and design of the work, project development, obtaining funding, critical revision of the manuscript for important intellectual content, and approval of the submitted version. MO has contributed to the development of the methodology. MO performed data analysis. FR, EA, MAH, AS, MPN and ZG were involved in the interpretation of data and drafting of the article. All authors have carefully reviewed and approved the final version of the manuscript for authorship.
Funding
This study was financially supported by Vice-chancellor of Research and Technology of Qom University of Medical Science with a registration code of No. 14021720.
Availability of Data and Materials
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
The authors declare no competing interests.
Ethics Approval and Consent to Participate
This project has received ethical approval from the Ethics Committee at Qom University of Medical Sciences, Qom, Iran (IR.MUQ.REC.1402.185).
Consent for Publication
Not applicable.
References
- 1.Morgan E, Arnold M, Gini A, Lorenzoni V, Cabasag CJ, Laversanne M, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Gut. 2023;72(2):338–44. [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clinic. 2021;71(3):209–49. [DOI] [PubMed] [Google Scholar]
- 3.Sharma R, Abbasi-Kangevari M, Abd-Rabu R, Abidi H, Abu-Gharbieh E, Acuna JM, et al. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7(7):627–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Douaiher J, Ravipati A, Grams B, Chowdhury S, Alatise O, Are C. Colorectal cancer—global burden, trends, and geographical variations. J Surg Oncol. 2017;115(5):619–30. [DOI] [PubMed] [Google Scholar]
- 5.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683–91. [DOI] [PubMed] [Google Scholar]
- 6.Mukalil GM, Nandania P, Daid S, Bolla P, Banerjee A, Suppala P, et al. IDDF2024-ABS-0440 Global burden of colorectal cancer and its attributable risk factors in southeast asia, east asia, and oceania from 1990–2021: an insight from the global burden of disease study 2021. 2024;73(2):A380-A2.
- 7.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clinic. 2015;65(2):87–108. [DOI] [PubMed] [Google Scholar]
- 8.Tanikawa C, Kamatani Y, Takahashi A, Momozawa Y, Leveque K, Nagayama S, et al. GWAS identifies two novel colorectal cancer loci at 16q24.1 and 20q13.12. Carcinogenesis. 2018;39(5):652–60. [DOI] [PubMed] [Google Scholar]
- 9.Brinks R, Hoyer A. Illness-death model: statistical perspective and differential equations. Lifetime Data Anal. 2018;24(4):743–54. [DOI] [PubMed] [Google Scholar]
- 10.Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, de Beaufort C, et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabet Endocrinol. 2022;10(10):741–60. [DOI] [PubMed] [Google Scholar]
- 11.Brinks R. Illness-Death model in chronic disease epidemiology: characteristics of a related, differential equation and an inverse problem. Comput Math Methods Med. 2018. 10.1155/2018/5091096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brinks R, Hoyer A. Illness-death model: statistical perspective and differential equations. Lifetime Data Anal. 2018;24:743–54. [DOI] [PubMed] [Google Scholar]
- 13.Ito C, Kurth T, Baune BT, Brinks R. Illness-death model as a framework for chronic disease burden projection: application to mental health epidemiology. Front Epidemiol. 2022;2. [DOI] [PMC free article] [PubMed]
- 14.Marchand LL, Wilkens LR, Kolonel LN, Hankin JH, Lyu L-C. Associations of sedentary lifestyle, obesity, smoking, alcohol use, and diabetes with the risk of colorectal cancer. Can Res. 1997;57(21):4787–94. [PubMed] [Google Scholar]
- 15.Aleksandrova K, Pischon T, Jenab M, Bueno-de-Mesquita HB, Fedirko V, Norat T, et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. 2014;12(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14(10): 101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cmjas RA, Ward E. Worldwide variations in colorectal cancer. CA Cancer J Clin. 2009;596:366–78. [DOI] [PubMed] [Google Scholar]
- 18.Kwakye G, Dally CK. Colorectal cancer screening in sub-Saharan Africa. Lancet Glob Health. 2022;10(7):e938–9. [DOI] [PubMed] [Google Scholar]
- 19.Graham A, Adeloye D, Grant L, Theodoratou E, Campbell H. Estimating the incidence of colorectal cancer in Sub-Saharan Africa: a systematic analysis. J Glob Health. 2012. 10.7189/jogh.02.020404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RG, Barzi A, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):177–93. [DOI] [PubMed] [Google Scholar]
- 21.Wong MC, Huang J, Lok V, Wang J, Fung F, Ding H, et al. Differences in incidence and mortality trends of colorectal cancer worldwide based on sex, age, and anatomic location. Clin Gastroenterol Hepatol. 2021;19(5):955-66.e61. [DOI] [PubMed] [Google Scholar]
- 22.Winawer SJ, Zauber AG, Ho MN, O’brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. New Engl J Med. 1993;329(27):1977–81. [DOI] [PubMed] [Google Scholar]
- 23.Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar M, Mulrow C, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997;112(2):594–642. [DOI] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics DoHIS. National Health Interview Survey Public Use Data File 2018. Centers for Disease Control and Prevention; 2019.
- 25.Shah SC, Kayamba V, Peek RM Jr, Heimburger D. Cancer control in low- and middle-income countries: Is it time to consider screening? J Glob Oncol. 2019;5:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vilares AT, Ciabattoni R, Cunha TM, Félix A. Cervical cancer in Cape Verde: reappraisal upon referral to a tertiary cancer centre. eCancermedicalscience. 2022. 10.3332/ecancer.2022.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hassan MRA, Ismail I, Suan MAM, Ahmad F, Khazim WKW, Othman Z, et al. Incidence and mortality rates of colorectal cancer in Malaysia. Epidemiol Health. 2016. 10.4178/epih.e2016007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu Y, Zhang C, Wang Q, Wu K, Sun Z, Tang Z, et al. Global, regional, and national burden of colorectal cancer and attributable risk factors, from 1990 to 2019: Updated results from the Global Burden of Disease Study 2019. 2022.
- 29.Rosenfeld DL, Tomiyama AJ. Gender differences in meat consumption and openness to vegetarianism. Appetite. 2021;166: 105475. [DOI] [PubMed] [Google Scholar]
- 30.Murphy N, Strickler HD, Stanczyk FZ, Xue X, Wassertheil-Smoller S, Rohan TE, et al. A prospective evaluation of endogenous sex hormone levels and colorectal cancer risk in postmenopausal women. J Nat Cancer Inst. 2015;107(10):djv210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rennert G, Rennert HS, Pinchev M, Gruber SB, Lavie O. Hormonal and reproductive factors and reduction in the risk of colorectal cancer. Eur J Cancer Prevent Off J Eur Cancer Prev Organ (ECP). 2020;29(3):229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.