Abstract
Autoantibody production during infections is considered to result from nonspecific activation of low-affinity autoreactive B cells. Whether this can lead to autoimmune disease remains uncertain. We show that chronic infection by Borrelia burgdorferi of Tg animals expressing human rheumatoid factor (RF) B cells (of low or intermediate affinities) in the absence or in the constitutive presence of the autoantigen (represented here by chimeric IgG with human constant region) breaks their state of immunological ignorance, leading to the production of RFs. Surprisingly, this production was more pronounced in intermediate-affinity RF Tg mice coexpressing the autoantigen. This overproduction was mediated by immune complexes and involved synergistic signaling between the B cell receptor and Toll-like receptors and T cell help. These findings indicate that chronic infection can activate autoreactive B cells with significant affinity and creates conditions that can drive them to differentiate into memory cells. Such cells may have some physiological yet undetermined role, but in autoimmune-prone individuals, this scenario may initiate autoimmunity.
Introduction
Susceptibility to autoimmune diseases is determined by a combination of genetic and environmental factors, the latter being mostly unknown. Among them, the role of infectious agents in the setting off or exacerbation of autoimmune diseases is still a matter of debate. Although there is substantial evidence that, in some circumstances, infections may have a protective effect against autoimmune-mediated diseases, clinical observations and several experimental models have suggested for decades that autoimmune diseases may be initiated or worsened by microbial infections (1). However, there is no real understanding of the underlying mechanisms (2). These questions have clear clinical implications.
In theory, the mechanisms by which a microbe may activate autoreactive cells could fall into 2 categories: antigen-specific and antigen-nonspecific. On one hand, the antigen-specific theory relies mainly on epitope mimicry. Indeed, cross-reactivity is frequent at the B cell level and even more at the T cell level because of the degeneracy of the T cell repertoire, making this model tantalizing for immunologists. However, it has not yet been convincingly demonstrated that epitope mimicry can set off an autoimmune disease (3). On the other hand, the antigen-nonspecific mechanisms are numerous and loosely grouped under the term “bystander activation.” For B cells, it has been known for decades that bacterial or viral infection, particularly when it is persistent, leads to polyclonal B cell proliferation and Ig production, and that newly synthesized specific Abs constitute generally only a small fraction in the resulting hypergammaglobulinemia (4–8). The mechanisms underlying this nonspecific B cell activation are far from obvious; in particular, they are most probably not limited to cytokines released from activated T cells, since they may involve cognate interactions with specific T cells (7). As recently emphasized by Silverstein and Rose, the old question of whether this polyclonal activation includes the turning on of anti-self and therefore may lead to autoimmune disease is still open (9). With current knowledge, 2 different situations can be considered. In the first, natural autoreactive B cells produce only low-affinity Abs. They escape tolerance mechanisms because they fall below the threshold for induction of anergy, deletion, or editing. Then polyclonal activation would result in the production of more of these innocuous Abs with no role for the autoantigen and with no clinical consequences. On the other hand, some anti-self B cells normally present in healthy subjects may have sufficient affinity to bind autoantigens and to receive some signal through the B cell receptor (BCR). Indeed, anti-self memory B cells expressing somatically mutated autoantibodies can be detected in normal individuals (10, 11). Under normal circumstances such cells would remain quiescent because a second signal is lacking or because they are kept silent by active immunological-ignorance mechanisms. The processes that allow these cells to escape normal tolerance mechanisms and that can trigger them to secrete autoantibodies are mostly unknown. In this view, important questions are: (a) do such cells participate in the polyclonal activation induced by an infection; (b) if so, by which mechanisms; and (c) can this lead to an autoantigen-driven maturation?
In order to address these issues, and to facilitate the analysis, we designed experimental infections of self-reactive B cell Tg mice. We chose Tg animals expressing a highly relevant model of human autoantibody, the rheumatoid factor (RF) (12). Indeed, B cells expressing BCRs specific for self Cγ (IgG), known as RF B cells, are present in large numbers in the normal human repertoire in spite of the ubiquitous presence of IgG in different biological forms (free or in immune complexes, soluble or membrane bound). Under normal conditions, RF B cells seem autoantigen ignorant and do not secrete RF. However, RF B cells can be activated in many autoimmune conditions, but also in nonautoimmune conditions and in particular during infectious diseases. Thus, we used 4 different lines of Tg mice expressing chimeric RFs (human variable regions, mouse IgM and IgD constant regions) that differed mainly by the affinity of the RFs for human IgG (huIgG), and by the absence or the constitutive presence of human Cγ1. Briefly, Smi RF Tg mice (previously designated nAAb; ref. 13) were constructed with a low-affinity (Kd = 10–6 M) polyreactive human RF. The autoreactive B cells of these mice are self antigen ignorant (i.e., they are not activated after encountering huIgG), even in the presence of the constitutive expression of chimeric IgG (cIgG; mouse variable regions, human Cγ1 region) (14); this mimics the physiological situation in humans. Hul RF Tg animals express somatically mutated V regions of a monoreactive and higher-affinity (Kd = 10–8 M) human RF, and their surface IgM+IgD+ (sIgM+sIgD+) autoreactive B cells are also ignorant after in vivo injections of huIgG (15). The fourth line of RF Tg mice also expresses Hul RF, but in the constitutive presence of cIgG, and is described in the first part of Results. Albeit there are some phenotypic differences among these Tg lines, their general features are the following: sIgM+sIgD+ RF B cells develop normally in the bone marrow, localize in the B zones of the secondary lymphoid organs, are not activated in the presence of huIgG, and without features of anergy (they can be activated through BCR-dependent and -independent pathways).
In the present study, we examine whether an experimental infection with Borrelia burgdorferi, a chronic infectious disease that is known to be associated with polyclonal hypergammaglobulinemia in both humans and mice (16), can break this state of immunological ignorance, and, if so, by which mechanisms. Our different Tg models allow us to study the potential roles of the autoantigen and of the affinity of the RF.
Results
Brief presentation of Hul × cIgG mice.
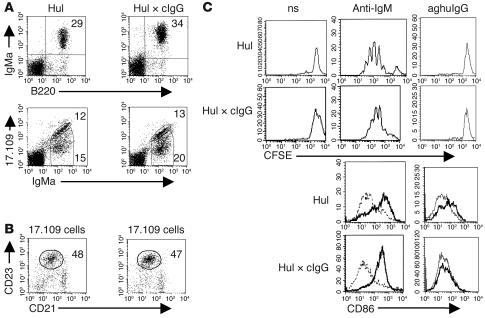
Given the potential role of membrane IgD in B cell tolerance (15), all the Tg lines used in this study coexpress the IgM and IgD isotypes of the Tg H chain. The Tg μ and κ chains are detected by an anti-μa reagent and 17.109 anti-idiotypic mAb, respectively. By crossing Hul Tg mice with cIgG knock-in mice, we generated animals designated Hul × cIgG that express both the chimeric Hul RF and a repertoire of cIgG with human Cγ1 region and murine variable regions (14, 17). In these animals, mean serum cIgG levels range between 150 and 200 μg/ml. As judged by triple immunofluorescence analysis with anti-IgMa, 17.109, and anti-huIgG, cIgGs were produced by a small proportion of IgMa–17.109– B cells that were present in the spleens (about 2%), excluding a cis effect (ref. 14 and data not shown). Rather unexpectedly, Hul RF B cells develop normally, populate the secondary lymphoid organs, and remain functionally naive, despite the fact that they are able to bind huIgG and cIgG at 50 μg/ml (ref. 15; and P. Soulas, unpublished results). Hul and Hul × cIgG mice had similar numbers of splenic B cells (18 × 106 ± 5 × 106 and 16 × 106 ± 6 × 106, respectively), and IgMa+17.109+ B cells that stained diagonally with the 2 Abs represented approximately 40% of total B cells in the spleen and LNs in both Tg mice (Figure 1A and Figure 2A, respectively). Most of the other B cells expressed the Tg H chain but were 17.109low/–. We previously showed that these cells express endogenous L chains and do not bind huIgG and therefore can be used as an internal control (15). Three- and 4-color FACS analysis indicated that most IgMa+17.109+ B cells were CD23+CD21+ and expressed basal levels of CD86, CD44, and CD69, a phenotype typical of naive follicular B cells (Figure 1, B and C, and data not shown). Although they could not be stimulated by huIgG either in monomeric form or aggregated, Hul RF B cells from Hul × cIgG Tg animals were not anergic. Their levels of BCR and CD86 expression were similar to those of Hul RF B cells from Hul Tg mice (Figures 1A and 2A), and they could be stimulated by anti-IgM Ab (Figure 1C). In summary, mature Hul RF B cells seem to behave similarly to mature Smi RF B cells in Smi × cIgG mice. Table 1 summarizes the main genetic and functional differences among the several types of transgenic mice used in our study.
Figure 1.
B cells in Hul and Hul × cIgG mice. Hul × cIgG RF B cells develop normally and remain functionally ignorant. (A) Flow cytometry of splenocytes from Hul and Hul × cIgG mice. Viable lymphocytes are gated on forward scatter (FSC) and side scatter (SSC) parameters. B220 staining reflects total B cells; IgMa is the Tg heavy chain allotype; 17.109 is the Tg light chain idiotype. Numbers indicate the mean percentage in the quadrants or the outlined gates. (B) Percentages of follicular B cells assessed by CD21 and CD23 expression on splenic 17.109+ cells. (C) Effects of in vitro stimulations on Hul and Hul × cIgG splenic B cells. Splenocytes were cultured for 72 hours in the presence of aggregated huIgG (aghuIgG, 1 mg/ml), anti-mouse IgM (10 μg/ml), or medium alone (nonstimulated [ns] or dashed line). Histograms show divisions of CFSE-labeled 17.109high B cells or surface expression of the CD86 activation marker on these cells.
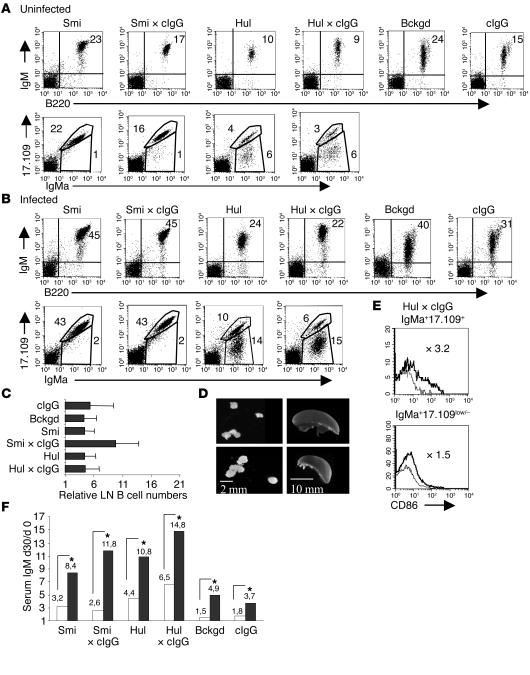
Figure 2.
LN B cells in RF Tg infected mice compared with uninfected mice. B. burgdorferi infection is associated with B cell activation and IgM production. Intermediate-affinity RF B cells appear specially sensitive to activation. (A and B) Flow cytometry analysis of LN cells from infected and uninfected mice. Analysis was performed as in Figure 1A. Numbers indicate the mean percentage for 5–13 mice. Differences between percentages of cells from infected versus uninfected mice are statistically significant for all lines (P < 0.05, Mann-Whitney test). (C) Numbers of IgM+B220+ B cells in infected animals, determined by cytofluorimetry in pooled LNs, relative to uninfected controls. Each value ± 1 SD represents the mean ratio from 5–13 mice. (D) Lymphadenomegaly in infected animals. Shown are spleen and inguinal LNs from an infected Hul × cIgG mouse (bottom), compared with the uninfected control (top). (E) Surface expression of CD86 on gated RF B cells (IgMa+17.109+) and non-RF B cells (IgMa+17.109low/–) 30 days after B. burgdorferi infection (thick line) in the Hul × cIgG line. (F) Levels of serum IgM in infected mice compared with controls. IgM levels were measured by ELISA. Values represent the mean relative increase of the total IgM production from day 0 to day 30 in infected mice (black bars) and uninfected mice (white bars). *P < 0.05, Mann-Whitney test. Numbers of tested animals are those represented in Figure 3A. Bckgd, background.
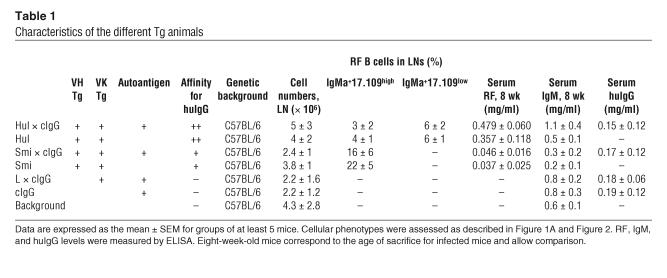
Table 1.
Characteristics of the different Tg animals
The B. burgdorferi infection model.
B. burgdorferi is able to induce in many inbred mouse strains, including C57BL/6, a chronic systemic infection characterized by recurrent bacteremia and by the invasion of many tissues (16, 18). The highest concentrations of spirochetes are found in ankle joints, heart, and skin. Although Abs play an important role in controlling spirochetes, the host defense is unable to completely eradicate established infection (19). This failure is thought to be the consequence of the important potential for antigenic variation in this organism, which involves different mechanisms (20). A hallmark of murine B. burgdorferi infection is the development of an arthritis that peaks 2–3 weeks after intradermal injection of the pathogen.
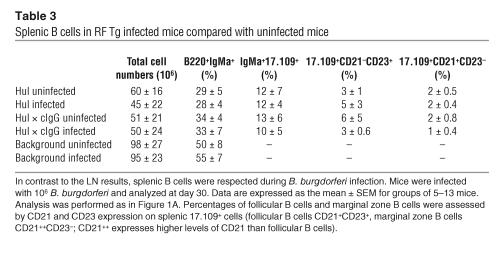
In the subsequent experiments, Hul and Smi Tg mice can be compared with Hul × cIgG and Smi × cIgG, respectively, since they share the same genetic backgrounds (see Methods). Four-week-old Tg and littermate controls were injected with 106 B. burgdorferi organisms and were sacrificed for analysis generally at 4 weeks after infection. The susceptibility of the Tg mice to experimental B. burgdorferi infection was evidenced by the following facts: (a) most RF Tg mice developed ankle joint arthritis 2 weeks after B. burgdorferi injection; (b) all the mice had a positive B. burgdorferi culture from at least 1 tissue sample (heart, ear skin, bladder) at 4 weeks; and (c) all the mice mounted a strong anti–B. burgdorferi IgG response, including a cIgG response in the relevant animals (Table 2). Infection resulted in at least a 3- to 4-fold increase in the total LN B cell numbers as compared with those in control mice injected with culture medium alone (Figure 2, B and C). The increase varied little among Tg, Tg × cIgG, and non-Tg mice. In Tg animals, RF B cells (IgMa+17.109+) and non-RF B cells (IgMa+17.109low/–) were equally affected (Figure 2B). The increase was already detected by day 20 after infection and persisted at day 45 (not shown). By contrast, we found no significant modification in the splenic B cell populations, which is possibly consistent with the fact that, for unclear reasons, spleen generally harbors very low numbers of B. burgdorferi (21) (Table 3). Accordingly, LNs from infected mice were always significantly enlarged, whereas spleen sizes remained normal (Figure 2D).
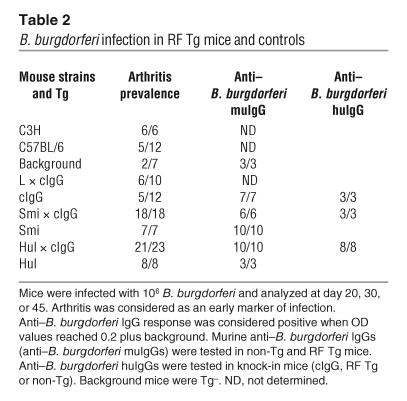
Table 2.
B. burgdorferi infection in RF Tg mice and controls
Table 3.
Splenic B cells in RF Tg infected mice compared with uninfected mice
Together these data are consistent with the facts that B. burgdorferi and its lipoproteins have been shown to possess in vitro mitogenic activity in both human and mouse B lymphocytes and that in vivo infection is associated with polyclonal hypergammaglobulinemia, only a minor fraction of which represents B. burgdorferi–specific Abs (8, 16, 22, 23).
B cell marker analysis indicates that Hul RF B cells have distinctive behavior in the presence of their autoantigen.
Spleen and LN B cells were analyzed by flow cytometry for levels of CD86 activation marker. At day 30 after infection, membrane expression of CD86 was close to basal levels in LN and splenic B cells in all the strains of non-Tg mice as well as in cIgG animals (CD86 mean fluorescent intensity, increased from 1.1 to 1.5 compared with respective uninfected mice). This is in accord with previous work showing that B. burgdorferi infection indeed upregulates the surface expression of CD86 in B cells, but only transiently, during the first 2 weeks after infection (24). By contrast, during the same period of time, a significant increase in CD86 level was still detected in IgMa+17.109+ LN cells, compared with that in IgMa+17.109low/– cells, from Hul × cIgG mice (Figure 2E) (P = 0.0007). Interestingly, no such observation could be made for IgMa+17.109+ cells from Hul, Smi, and Smi × cIgG mice, in which CD86 levels were close to baseline (not shown).
B. burgdorferi infection induced production of RF that was in part dependent on the presence of the autoantigen.
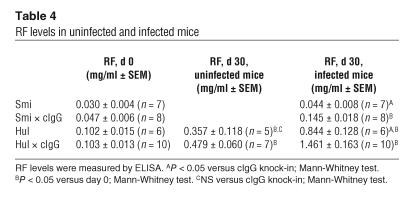
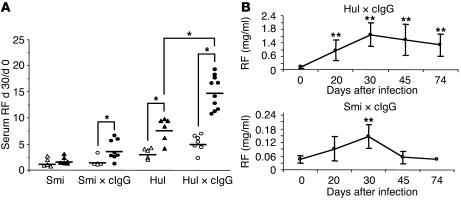
Consistent with previous work in wild-type animals (22), infection of Tg mice and of non-Tg littermates resulted in a 2- to 4-fold increase in the serum concentration of total IgM as compared with injection with culture medium (Figure 2F). To examine whether RF B cells were involved in the hypergammaglobulinemia induced by B. burgdorferi infection, serum Tg RF concentrations were measured by ELISA at different times after infection. At day 30 after infection, RF levels were increased in all infected mice (Table 4). Since serum total IgM and RF naturally increase in animals between 4 and 8 weeks of age, we also compared the ratios of serum RF at day 30 after infection to serum RF at day 0 between infected and uninfected animals (Figure 3A). Interestingly, the increase of RF production resulting from B. burgdorferi infection was significantly higher in Smi × cIgG and Hul × cIgG mice than in Smi and Hul animals, respectively. In addition, this increase was most noticeable in infected Hul × cIgG animals compared with uninfected mice as well as with infected Hul Tg mice (P = 0.0002 and P = 0.0017, respectively). The data presented in Table 4 allowed us to calculate the ratios of RF levels at day 30 between infected and uninfected animals and to show that the increase of RF production was more than 30% higher in Hul × cIgG mice than in Hul mice. In Hul × cIgG mice, RF represented 95% of the total serum IgM at day 30 after infection (mean RF level 1.46 ± 0.16 mg/ml and mean IgM level 1.55 ± 0.25 mg/ml) versus 60% in uninfected Hul × cIgG controls. These data imply that during B. burgdorferi infection, RF B cells are activated by 2 different additive mechanisms: 1 is nonspecific, and the second depends on the presence of the autoantigen cIgG. Although Smi and Hul mice must be compared with caution since they are different Tg lines, a role for an RF-cIgG interaction in the second mechanism is further supported by (a) the fact that the overproduction of RF when cIgG was present was most noticeable in Hul animals (Hul RF affinity for IgG was roughly 2 log higher than that of Smi); and (b) the kinetic of RF production in Tg × cIgG mice: in Smi × cIgG mice the RF response was transient, peaking around day 30 after infection to return to base-line levels by day 45. By contrast, in Hul × cIgG mice the response was more sustained (Figure 3B).
Table 4.
RF levels in uninfected and infected mice
Figure 3.
B. burgdorferi infection induces production of RF that is in part dependent on the presence of the autoantigen. (A) Ratios of serum RF levels between day 30 and day 0 in infected mice compared with controls. Each point represents an individual mouse and the relative level of RF at day 30 compared with the day 0 level. Open symbols, uninfected; filled symbols, infected. *P < 0.05, Mann-Whitney test. (B) Kinetic of mean RF levels between day 0 and day of sacrifice in Hul × cIgG infected mice, compared with Smi × cIgG infected mice. **P < 0.005 compared with day 0 level, Mann-Whitney test.
These data together with the CD86 expression analysis indicate that during B. burgdorferi infection RF B cells are activated to proliferate and to secrete RF by a nonspecific mechanism, i.e., irrespective of the BCR specificity. However, RF B cells are further activated in the presence of cIgG, possibly reflecting BCR signaling. This is especially true for Hul mice; thus we focused our next experiments on these lines.
Mechanisms of RF B cell activation.
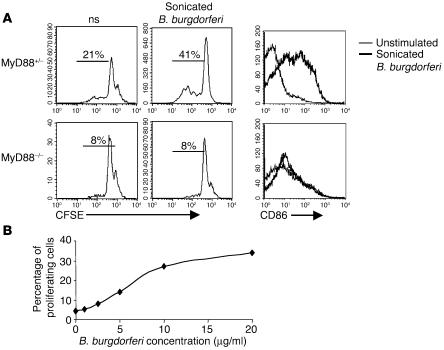
As mentioned above, B. burgdorferi lipoproteins have been reported to possess potent B cell mitogenic properties capable of stimulating polyclonal activation and proliferation and Ig production in vitro. These properties are dependent on the Pam3Cys modification of lipoproteins and involve TLRs, particularly TLR2 complexed to TLR1 (21, 25–27). Most known mammalian TLRs, including the TLR1/2 complex, signal through the adapter protein MyD88 (28). Purified B cells could be activated by a B. burgdorferi sonicate in vitro, but the proliferation was completely abolished for cells from MyD88-deficient mice (Figure 4A). As expected, Hul RF B cells from Hul × cIgG Tg mice proliferated in a dose-dependent manner in the presence of B. burgdorferi sonicate (Figure 4B). Since we previously determined that purified Hul IgM-RF does not bind B. burgdorferi antigens (ELISA and Western blot; not shown), these data together with previous studies indicate that during B. burgdorferi infection RF B cells can be activated mainly by a TLR pathway independent of BCR specificity.
Figure 4.
Proliferation and activation of B cells in MyD88 wild-type (or MyD88+/–) mice and MyD88-deficient mice. (A) Purified B cells from MyD88–/– or MyD88+/– mice on a C57BL/6 background were cultured for 72 hours in the presence or absence of sonicated B. burgdorferi (10 μg/ml). Histograms show divisions of CFSE-labeled B cells or surface expression of CD86 activation marker. Percentages indicate proliferating cells. (B) Splenocytes from Hul × cIgG mice were cultured in the presence of different concentrations of sonicated B. burgdorferi. The percentage of proliferating cells was measured for each concentration after CFSE staining.
However, nonspecific B cell activation does not explain why RF production is enhanced in Hul × cIgG Tg mice compared with that in Hul Tg animals. We considered 2 not mutually exclusive mechanisms: (a) synergy between the BCR and a second receptor on the B cell surface, and (b) T cell help.
In view of the above data, candidate second receptors include members of the TLR family. Recently, Leadbetter et al. showed that AM14 RF B cells, which express a low-affinity murine Tg RF, can be activated in vitro by chromatin/IgG complexes isolated from the serum of autoimmune mice but not by IgG alone (29). This effective activation required a synergistic engagement of the antigen receptor and a member of the MyD88-dependent TLR family, most probably TLR9, which binds hypomethylated CpG motifs. We hypothesized that a similar mechanism, possibly involving other TLRs including the TLR1/2 complex, could operate in Hul × cIgG infected animals. In this view it is worth noting that anti-chromatin IgGs were not detected in the serum of any infected mice by ELISA (data not shown). To examine further the mechanisms of RF B cell activation in Hul Tg mice, splenocytes from these animals were stimulated in vitro with sonicated B. burgdorferi, purified huIgG from patients with high serum levels of anti–B. burgdorferi IgG (anti–B. burgdorferi huIgG), or immune complexes prepared by preincubation of these anti–B. burgdorferi huIgGs with sonicated B. burgdorferi. We also checked for the absence of anti-chromatin Ab in the patients’ purified huIgG. All these reagents were toxin free. In the following experiments, sonicated B. burgdorferi was used at low concentration (2.5 μg/ml) to avoid masking the potential contribution of the huIgG. After 72 hours, we harvested the cells for flow cytometric analyses and collected the supernatants for measurements of IgM-RF by ELISA. RF B cells increased in size, upregulated CD86, and proliferated strongly in response to B. burgdorferi/anti–B. burgdorferi huIgG immune complexes, whereas B. burgdorferi or anti–B. burgdorferi huIgG alone, as well as B. burgdorferi preincubated with huIgG from healthy subjects (normal huIgG), produced little, if any, response (Figure 5A). RF B cell activation was autoantigen specific, since IgMa+17.109low/– B cells were not activated under the same conditions. Finally, sonicated B. burgdorferi stimulated RF production in vitro, whereas anti–B. burgdorferi huIgG alone did not. In accord with the proliferation data, B. burgdorferi/anti–B. burgdorferi huIgG immune complexes enhanced RF production by 30% compared with B. burgdorferi alone (Figure 5B).
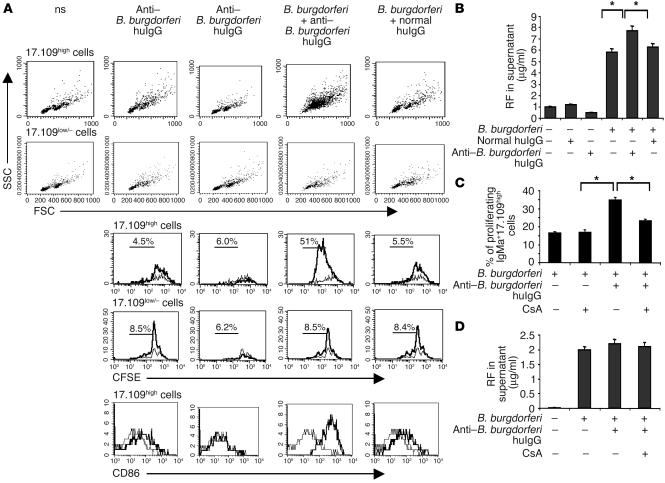
Figure 5.
Proliferation and activation of RF B cells in response to B. burgdorferi are increased in the presence of B. burgdorferi/IgG complexes. (A and B) Splenocytes of Hul Tg mice were cultured with suboptimal concentrations (2.5 μg/ml) of sonicated B. burgdorferi, purified human anti–B. burgdorferi huIgG (1 mg/ml), a mixed solution containing B. burgdorferi and purified anti–B. burgdorferi huIgG, or a mixed solution containing B. burgdorferi and nonspecific huIgG (normal huIgG). (A) Side scatter versus forward scatter plots were used to monitor cell size of 17.109high or 17.109low/– B cells (top 2 rows). The next 2 rows of histograms show divisions of CFSE-labeled 17.109high or 17.109low/– B cells; percentages indicate proliferating cells. The bottom row of histograms shows surface expression of CD86 on 17.109high B cells. Thick lines represent the stimulated B cells, and thin lines the nonstimulated B cells. Results shown are representative of 4 separate experiments. Acquisition parameters were determined to analyze at least 2 × 103 cells in the 17.109high or 17.109low/– B cell gates (total numbers of cells: 4 × 104 to 2 × 106). (B) RF supernatant production was measured at day 3. Values ± 1 SEM are shown. *P < 0.05. (C and D) Purified splenic B cells of Hul Tg mice were cultured as in A. (C) CsA (50 ng/ml) was added at culture initiation. Values ± SEM represent the percentage of proliferating IgMa+17.109high cells in the different conditions of stimulation. *P < 0.05. (D) RF supernatant production ± SEM was measured at day 3.
This selective activation could reflect BCR signaling; alternatively, surface RF, by trapping immune complexes, may simply concentrate B. burgdorferi particles on the B cell membrane, thus enhancing TLR signaling. To distinguish between these hypotheses, we took advantage of the fact that the calcineurin antagonist cyclosporin A (CsA) is known to prevent the BCR cross-linking–induced activation of NFAT required for cellular proliferation without significantly altering TLR signaling, which does not involve any known calcium-calcineurin step (30). Purified Hul RF B cells were cultured as before in the presence or absence of CsA at 50 ng/ml (higher concentrations resulted in cellular toxicity). Consistent with our first hypothesis, CsA blocked the selective enhancement of Hul RF B cell proliferation induced by B. burgdorferi/IgG immune complexes without interfering with the proliferation induced by B. burgdorferi alone (Figure 5C). Since for these experiments we used purified B lymphocytes, the data also show that both BCR-dependent and BCR-independent RF B cell–induced proliferations did not require other cells — in particular, T cells. However, a different pattern comes to light when autoantibody production is examined. Indeed, anti–B. burgdorferi immune complexes were no more able to increase the RF secretion induced by B. burgdorferi alone (Figure 5D). This suggests that the Ab secretion component of the RF B cell activation induced by B. burgdorferi/huIgG complexes may depend on the presence of other cells, Th cells being obvious candidates.
Among autoreactive B cells, RF B cells have the noteworthy property of recognizing an autoantigen of which the main biological role is to bind foreign antigens. It has been shown in vitro that RF B cells are able to capture foreign antigens in immune complex form and to activate specific T cells (31). However, the relevance of this mechanism in vivo is unknown. To investigate the role of T cells in the breakdown of Tg RF B cell tolerance, we treated Hul and Hul × cIgG mice 2 days before the infectious challenge with a nondepleting anti-CD4 mAb under conditions demonstrated to completely coat and block CD4+ T cells for 4 weeks (32). Animals were sacrificed 30 days after infection and analyzed as above. There was no significant difference in the B cell phenotypes between these animals and the immunocompetent ones (not shown); in particular, B. burgdorferi infection resulted in a comparable increase of the LN B cell compartments (roughly 4-fold). Likewise, serum RF levels were still increased in Hul infected animals compared with healthy animals, which is consistent with the fact that B. burgdorferi is directly mitogenic for B cells in vitro (Figure 6A). However, most interestingly, CD4 T cell blockage completely abolished the autoantigen-dependent enhanced production of serum RF in infected Hul × cIgG mice.
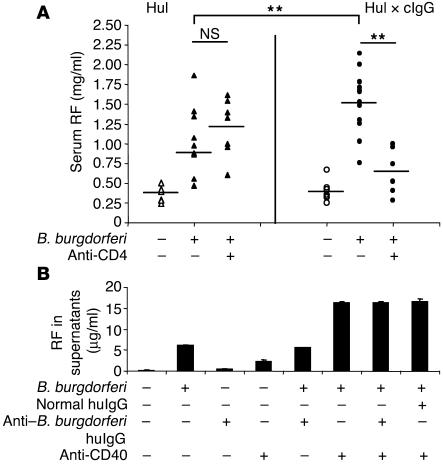
Figure 6.
cIgG-dependent RF production in Hul × cIgG Tg mice requires T cell help. (A) Transgenics were treated by several i.p. injections of the anti-CD4 mAb YTS177 to block CD4+ cells for at least 4 weeks (see Methods). Each point represents the serum RF level in a single mouse. The infected and treated mice are compared with infected and untreated mice. Uninfected mice are shown as controls. Differences between Hul × cIgG infected treated and untreated mice are significant (P < 0.05, Mann-Whitney test), whereas differences between Hul infected treated and untreated mice are not (NS). Differences between Hul infected and Hul × cIgG infected treated and untreated mice are significant (**P < 0.05, Mann-Whitney test). (B) Purified splenic B cells of Hul Tg mice were cultured for 6 days in the same conditions as in Figure 5A. Anti-CD40 agonist (10 μg/ml) was added beforehand to mimic T cell help. RF production ± SEM was measured at day 6 in the supernatants.
Depending on the system, the T cell help can be mediated by the interaction of CD40 ligand (CD154) with CD40 that is constitutively expressed by B cells, and/or by secreted ILs. Because syngeneic B. burgdorferi–specific T cell clones were not available, we evaluated the contribution of CD40 signaling using a stimulating anti-CD40 Ab. Purified B cells from Hul Tg mice were cultured with sonicated B. burgdorferi, anti–B. burgdorferi huIgG, or B. burgdorferi/anti–B. burgdorferi huIgG immune complexes in the presence or absence of activating anti-CD40 Ab (Figure 6B). Anti-CD40 Ab clearly promoted RF secretion induced by B. burgdorferi alone. This indicates that concurrent TLR stimulation by B. burgdorferi is synergistic with CD40 signaling to induce B lymphocyte differentiation into Ab-secreting cells. Such a costimulation was not observed for B cells from MyD88–/– mice (data not shown). In these experiments anti–B. burgdorferi huIgG immune complexes were not more potent than B. burgdorferi alone nor than B. burgdorferi preincubated with normal huIgG to induce RF production. This could be due to culture conditions; alternatively, it could indicate that the main role of the BCR in the autoantigen-specific activation of RF B cells is to deliver B. burgdorferi antigens to specific T cells.
Discussion
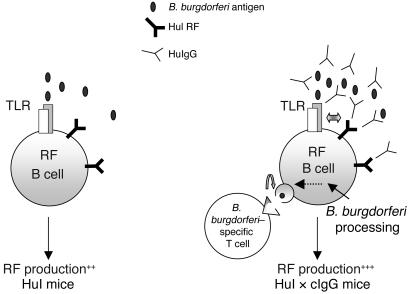
Overall, the data presented herein show that, during a chronic bacterial infection, innate immunity receptors (most probably TLRs), the autoantigen, and CD4 T cells cooperate to break the immunological ignorance of RF B cells in mice that are not genetically prone to develop autoimmune diseases (see Figure 7 for a summary of the mechanisms potentially involved).
Figure 7.
A possible mechanism for the activation of RF-expressing Hul B cells in Hul × cIgG mice by immune complexes containing anti–B. burgdorferi IgG and B. burgdorferi antigens. In the left panel, B cells as well as RF B cells are stimulated by B. burgdorferi through TLR interaction. In the right panel, the presence of anti–B. burgdorferi huIgG in Hul × cIgG mice induces the formation of B. burgdorferi–containing immune complexes, which are able to cosignal through TLR and RF-BCR. B. burgdorferi is processed into antigenic peptides in RF B cells after internalization; B. burgdorferi–specific T cells cooperate to increase RF production. ++ and +++ refer to the intensity of RF production.
In humans, infectious diseases with a wide variety of pathogens, as diverse as subacute bacterial endocarditis, tuberculosis, and type C viral hepatitis, are frequently associated with a high production of RFs (12). The mechanism of this production is usually considered to be nonspecific, i.e., irrespective of the BCR specificity. Indeed, our results show that autoantigen-ignorant Tg RF B cells proliferate like other B cells and that RFs participate in the resulting hypergammaglobulinemia. However, RF production is substantially higher and is more sustained in Hul × cIgG compared with the other Tg lines (low-affinity RF, and Hul), which shows that an autoantigen-induced step constitutes a second mechanism involved in RF production.
The mechanisms underlying nonspecific B cell activation during infectious states have long been studied, although many issues remain unclear (1, 2, 4, 5–7, 9, 33). There is convincing evidence that these mechanisms are numerous, including direct activation by B cell mitogens; cytokines released from activated T cells, which may substitute nonspecifically for Th cells; or even T cell help that occurs through cognate interaction but is independent of BCR specificity (7). Regarding B. burgdorferi infection, activation of B cells through TLRs certainly plays an important role. B. burgdorferi lipoproteins including OspA and OspB possess potent B cell mitogenic properties capable of stimulating polyclonal proliferation and Ig production in vitro (21, 25–27). These properties are dependent on the Pam3Cys modification of lipoproteins and involve TLRs, particularly TLR2. Here we have shown that the proliferation of B cells from wild-type mice induced by B. burgdorferi in vitro is completely abolished for cells from MyD88-deficient mice. In addition, the experiments depicted in Figure 4A and Figure 5C clearly demonstrate that purified murine B cells can be directly stimulated by B. burgdorferi, even though the participation in vivo of other cells expressing TLRs and/or of other pathogen-associated molecular pattern (PAMP) receptors is likely. Still, the process is not dependent on CD4 T cells, since their blockade does not reduce the production of RFs in Hul infected mice.
The second, autoantigen-induced, step is illustrated by the increased RF production in Hul × cIgG mice compared with Hul animals. The results in vivo are underpinned by in vitro experiments. Immune complexes made of anti–B. burgdorferi huIgG and sonicated B. burgdorferi greatly enhance the activation and proliferation of RF B cells as well as the secretion of RF compared with those induced by B. burgdorferi alone. This phenomenon is autoantigen-specific, since it is not observable for non-RF IgMa+17.109low/– B cells. As expected from previous data (15), anti–B. burgdorferi huIgG alone had no effect. While CsA treatment did not interfere with B. burgdorferi-induced proliferation, it blocked the enhancement of proliferation induced by the immune complexes, which strongly support BCR signaling. This phenomenon could find its biological significance in a possible role as an amplifier of immune responses, which is suspected for RF B cells. Indeed, Roosnek and Lanzavecchia have shown in vitro that RF B cells can capture exogenous antigens in immune complex form, process them, and present antigenic peptides to specific CD4 T cells (31). These T cells could then induce RF B cells to secrete through cognate interactions. In accord with this hypothesis, we show that CD4 T cell blockade in vivo had no effect on the nonspecific part of the RF B cell activation, since serum RFs were similar between anti-CD4–treated and untreated Hul infected mice. However, CD4 T cell blockade completely suppressed the autoantigen-dependent RF production in Hul × cIgG mice. To be precise, CD4 T cells seem dispensable for the proliferation component of the selective activation mediated by anti–B. burgdorferi immune complexes, since it was still observed with purified B cells and since IgMa+17.109+ cell numbers were increased in similar proportions in anti-CD4–treated and untreated mice. However, their presence is critical for the autoantigen-induced secretion of RF. With current knowledge, the most straightforward explanation is that RF B cells, having captured B. burgdorferi antigens in immune complex form, receive T cell help through a cognate interaction with anti–B. burgdorferi–specific T cells, which allows them to differentiate into plasma cells. Alternatively, secondary to TLR/BCR costimulation, B cells may be able to differentiate following noncognate interaction with activated CD4 T cells or with cytokines produced by them. Distinguishing between these hypotheses is at present hampered by the lack of available B. burgdorferi–specific CD4 T cell clones. A limitation of our study is the impossibility to provide direct evidence for the involvement of immune complexes in vivo.
From an autoimmunity point of view, several points merit further attention. First, it has been shown that in vivo bacterial infectious disease can activate not only low-affinity autoreactive B cells, but also higher-affinity anti-self B cells that have escaped central or peripheral tolerance. These last cells are known to exist in humans during chronic infection with mycobacteria (34), but also in healthy individuals (10, 35), maybe as a consequence of repeated benign infections. Whether autoreactive B cell activation by this process can lead to affinity maturation remains an open question. Somatic hypermutation is usually poorly effective in regular Ab Tg systems on non–autoimmune-prone genetic backgrounds; therefore it is probable that it cannot be readily studied with our current models. However, efficient antigen-driven somatic hypermutation is usually dependent on the availability of T cell help, which is shown here to occur in the second, autoantigen-induced, step of RF B cell activation.
Second, in view of the recent data from Marshak-Rothstein’s and Goodnow’s groups (29, 30), it is reasonable to assume that Hul RF B cells are activated through a 2-signal mechanism involving concurrent stimulations of the BCR and some PAMP receptor, most probably TLR, pathways. The direct demonstration of this hypothesis and the identification of the involved receptors will necessitate the generation of RF Tg backcrosses to appropriate KO mice. Rui et al. have demonstrated in the anti–hen-egg lysozyme (anti-HEL) model that stimulation with antigen is synergistic with CpG DNA through TLR9 signaling (30), and Leadbetter et al. have shown that mammalian chromatin-containing IgG immune complexes induce the proliferation of AM14 RF B cells in vitro and have provided strong evidence that this phenomenon results from the sequential engagement of the BCR and TLR9 (29). In our model, TLR9 is probably not similarly involved, since infected mouse serum and purified huIgG enriched in anti–B. burgdorferi huIgG were devoid of anti-chromatin Abs. This theory was recently questioned by Rui et al., who showed in vitro that autoreactive B cells that were anergized by the constitutive presence of the autoantigen could not be induced to produce autoantibodies by activation of the TLR pathway (30). Our data suggest that there is a window of BCR affinities that allow autoreactive B cells to evade classical tolerance mechanisms and to appear ignorant but that permit their activation by the autoantigen when a second signal is provided. We think that our results extend the BCR/TLR9 coengagement paradigm and further support a role for this mechanism as a link between infection and autoimmunity.
Third, the next question is whether any autoreactive B cells can be activated by this mechanism provided that self antigen is accessible to the BCR. Recently, Viglianti et al. have extended the BCR/TLR9 coengagement to DNA-reactive B cells (36). However, an important result from our in vitro experiments is that normal huIgG (i.e., devoid of anti–B. burgdorferi Abs) are unable to increase the activation of Hul RF B cells induced by B. burgdorferi. This suggests that a physical interaction or a cross-link between the TLR and the BCR may be required. Since TLR9 is not expressed at the B cell membrane, this could occur at the membrane of the TLR9-associated subcellular compartment after internalization of the BCR complexed with DNA fragments. If such a limitation proved to be true, it could, together with the high frequencies of RF and anti-nuclear Abs expressing B cells in the naive repertoire, account for the fact that these autoantibodies are the most frequent produced during infectious diseases. However, the results obtained in the CpG DNA anti-HEL model are more difficult to account for. One possibility could be that HEL binds to CpG DNA through charge-based interactions (30). Clearly this question needs further investigation.
Finally, further studies will be required to first determine the mechanism that controls the occurrence of pathogenic autoantibodies in individuals recurrently exposed to infectious diseases, and second, to determine what differentiates these individuals from patients suffering from autoimmune disease.
Methods
Mice.
All mouse lines were housed and crossed in isolator cages at the animal facility of the Centre de recherche d’immunologie et d’HÉmatologie (Hôpital Civil). B. burgdorferi–inoculated mice and the uninfected controls were housed in the animal facility at the Laboratoire de bactériologie (Hôpitaux universitaires de Strasbourg). C57BL/6 and C3H/Hej mice were bought from Harlan France SARL. MyD88-deficient mice (MyD88 KO, or MyD88–/–) on a C57BL/6 background were bought from the Centre de Distribution, de Typage et d’Archivage (Orleans, France) animal laboratories. All animal experiments were performed with approval by the Direction départementale des services vétérinaires (Strasbourg, France).
The generation of Smi, Smi × cIgG, Hul, and Hul × cIgG mice has been previously described (13–15). Briefly, RF transgenics are generated as single-chain transgenics (H or L) on a C57BL/6 background. Single-chain transgenics are crossed with cIgG knock-in mice generated on a mixed background (at least 6 backcrosses with C57BL/6 mice) and then intercrossed to obtain Smi, Smi × cIgG, Hul, and Hul × cIgG mice on the same genetic background. For experiments, Tg mice were always compared with their littermate controls. The cIgG knock-in line was kindly provided by K. Rajewsky (CBR Institute for Biochemical Research, Harvard Medical School, Boston, Massachusetts, USA) and expressed cIgG with human γ chain C1 region.
Screening of the transgenics was performed as previously described (13). Smi and Hul transgenics were identified after tail DNA PCR typing, and cIgG knock-in mice were selected by ELISA (huIgG dosage; ref. 17).
MyD88+/– mice were obtained by backcrossing of MyD88 KO mice with C57BL/6 mice.
B. burgdorferi infection.
The B. burgdorferi sensu stricto cN40 isolate was cultivated at low passage in Barbour-Stoenner-Kelly medium (BSK-H medium; Sigma-Aldrich) supplemented with 6% normal rabbit serum (Sigma-Aldrich) at 33°C. Four-week-old mice were infected with 106 spirochetes by intradermal injection of 0.1 ml in the shaved back. Control mice were injected with an equal volume of sterile BSK-H medium and housed in the same conditions as infected animals. Mice were killed at intervals of 2–8 weeks after inoculation. The infectious status of the animals was determined at sacrifice by culture of different specimens (bladder, ear, heart, spleen) in 7-ml tubes of BSK-H medium for up to 4 weeks at 33°C. Considering 100 infected animals, culture of at least 1 organ was positive for 90. Only the animals with a positive culture were included in our analysis.
Flow cytometry.
Preparation of LNs and spleen cell suspensions and their staining for flow cytometry have been already described (13). The analysis of the B cell phenotype was performed by double or triple staining with anti-B220FITC, anti-IgMabiotin, anti-IgMPE, CD21FITC, CD23PE (BD Biosciences — Pharmingen), and 17.109biotin; 17.109 recognizes the Tg RF VK chain idiotype and was provided by D.A. Carson (University of San Diego, San Diego, California, USA). The expression analysis of the activation marker CD86 was performed using anti-CD86PE (BD Biosciences — Pharmingen). Viable cells were identified by incorporation of propidium iodide (5 mg/ml). The analysis was performed with a FACSCalibur using the CellQuest software package (BD Biosciences).
ELISA.
ELISA assays for serum IgM and serum chimeric RF were done as previously described (13, 15). Binding of total IgM was determined by addition of a peroxidase-coupled anti-mouse IgM (Jackson ImmunoResearch Laboratories Inc.). For RF dosage, plates were coated with anti-IgMa (Smi and Smi × cIgG mice) or the mAb H1.10 (Hul and Hul × cIgG mice), and serum RF concentrations were revealed by addition of biotin-labeled 17.109 Ab and then steptavidin-peroxidase. The H1.10 mAb recognizes the Tg Hul RF VH chain idiotype and was provided by D.A. Carson.
For murine RF, plates were coated with total murine IgG (50 μg/ml; Jackson ImmunoResearch Laboratories Inc.), and serum RF concentrations were revealed by addition of a peroxidase-coupled anti-mouse IgM.
Mouse sera were tested for human and murine IgG Abs against B. burgdorferi using a modified commercial kit (Enzygnost Borreliosis IgG kit; Dade Behring Inc.). To detect murine IgG against B. burgdorferi, the anti-human conjugate was replaced by a peroxidase-conjugated F(ab′)2 goat anti-mouse IgG diluted to 1:50,000 (Jackson ImmunoResearch Laboratories Inc.). The other steps of the protocol were as described by the manufacturer. Sera were considered positive when OD values reached the OD of pooled uninfected mice plus 3 SD.
Mouse sera were tested for huIgG Abs against chromatin using a commercial kit (QUANTA Lite chromatin kit; INOVA Diagnostics Inc.). The subsequent steps of the test were performed as described previously (37). As positive controls, the positive standard serum included in the kit and a positive patient’s serum were used.
B cell proliferation assays.
Spleens or LNs were removed from Tg mice, non-Tg littermates, MyD88-deficient mice, MyD88+/– mice, or control C57BL/6 mice and teased apart. Cells were washed and resuspended in RPMI 1640 with L-glutamine (BioWhittaker Inc.) supplemented with gentamicin (40 μg/ml; BioWhittaker Inc.), 2-mercaptoethanol (50 μM; Sigma-Aldrich), and 10% heat-inactivated FCS (Dominique Dutscher). Cells (1.106 per milliliter) were incubated in 24-well BD Falcon plates (in a total volume of 1,000 μl) with 10 μg/ml LPS from Salmonella typhi (Sigma-Aldrich), 10 μg/ml of a F(ab′)2 goat anti-mouse IgM (Jackson ImmunoResearch Laboratories Inc.), 1 mg/ml of aggregated huIgG (Sandoglobuline; Novartis Pharma), 2.5–10 μg/ml of sonicated B. burgdorferi, 1 mg/ml purified huIgG from healthy individuals or B. burgdorferi-infected patients, or mixed solution containing B. burgdorferi (2.5 μg/ml) and huIgG (1 mg/ml), in the presence or absence of 10 μg/ml anti-CD40 agonist (BD Biosciences — Pharmingen) or 50 ng/ml CsA (Novartis Pharma). Aggregated huIgGs were prepared by heating at 65°C for 15 minutes.
After 60–72 hours of culture at 37°C, the phenotype of the cells was determined by flow cytometry analysis.
For proliferation assays, cells were labeled with CFSE (Invitrogen Corp.) before addition of LPS, anti-IgM, or B. burgdorferi with or without huIgG. Suspensions of 2.107 cells per milliliter in 0.1% PBS/BSA were incubated with CFSE at a final concentration of 2 μM for 10 minutes at 37°C. Cells were then washed and resuspended in the culture medium.
For CD86 expression, the cells were labeled after 60–72 hours of culture, as described in “Flow cytometry.”
Preparation of B. burgdorferi/huIgG complexes.
Sonicated B. burgdorferi was prepared as follows. B. burgdorferi sensu stricto cN40 was grown at 33°C in ten 7-ml tubes of BSK-H medium and harvested after 5 days of culture. The cell pellet was washed 3 times with cold PBS and 0.1% MgCl2 (pH 7.2). The final pellet was resuspended in 1 ml of Tris-HCl, 0.5 M (pH 8), and 2 ml of Laemmli buffer (Bio-Rad Laboratories) and denaturated by heating at 95°C for 3 minutes. The protein content of this preparation was determined by Lowry assay.
To purify huIgG, pooled sera from infected patients or controls (IgG anti–B. burgdorferi titers between 500 and 1,000 U as determined by the Enzygnost Borreliosis IgG kit; Dade Behring Inc.) were cleared by centrifugation and decomplemented. Each pool of serum was then loaded onto a DEAE Affi-Gel Blue Gel column (Bio-Rad Laboratories) according to the manufacturer’s instructions. Eluted fractions were concentrated and switched to PBS buffer using Stir Cel Omega 30K (Pall Corp.). IgG titers were measured by ELISA. IgG solutions were then tested for endotoxins (PYROGENT Plus Cel Clot Assay; Cambrex Corp.).
Immune complexes comprising B. burgdorferi and huIgG were made by premixing of B. burgdorferi solution with IgG at room temperature for 120 minutes, before addition to the assay.
B lymphocyte purification (magnetic cell separation).
Splenic B cells were isolated with a magnetic cell separation (MACS) depletion protocol (Miltenyi Biotec). Splenocyte samples were depleted of non-B cells with anti-CD43 magnetic beads (Miltenyi Biotec). The purity of the B cell fractions was greater than 80%.
Anti-CD4 treatment.
Nondepleting mouse anti-CD4 Abs (YTS177.9.6.1; ref. 38) in ascite form diluted in PBS (50 μl ascite plus 50 μl PBS per mouse per injection) were administered i.p. 2 days before B. burgdorferi infection, and then twice a week until sacrifice. Control animals were injected with PBS.
Acknowledgments
We thank S. Muller and F. Monneaux for help with murine and human anti-chromatin IgG ELISAs. This work was supported by grants from INSERM, Association pour la Recherche sur la Polyarthrite, and Strasbourg Louis Pasteur University.
Footnotes
Nonstandard abbreviations used: anti–B. burgdorferi huIgG, huIgG from patients with high serum levels of anti–B. burgdorferi IgG; BCR, B cell receptor; BSK-H medium, Barbour-Stoenner-Kelly medium; CsA, cyclosporin A; huIgG, human IgG; PAMP, pathogen-associated molecular pattern; RF, rheumatoid factor.
Conflict of interest: The authors have declared that no conflict of interest exists.
References
- 1.Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N. Engl. J. Med. 2002;347:911–920. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 2.Wucherpfennig KW. Mechanisms for the induction of autoimmunity by infectious agents. J. Clin. Invest. 2001;108:1097–1104. doi:10.1172/JCI200114235. doi: 10.1172/JCI14235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benoist C, Mathis D. Autoimmunity provoked by infection: how good is the case for T cell epitope mimicry [review]? Nat. Immunol. 2001;2:797–801. doi: 10.1038/ni0901-797. [DOI] [PubMed] [Google Scholar]
- 4.Sangster MY, et al. Analysis of the virus-specific and nonspecific B cell response to a persistent B-lymphotropic gammaherpesvirus. J. Immunol. 2000;164:1820–1828. doi: 10.4049/jimmunol.164.4.1820. [DOI] [PubMed] [Google Scholar]
- 5.Oldstone MB, Dixon FJ. Pathogenesis of chronic disease associated with persistent lymphocytic choriomeningitis viral infection. I. Relationship of antibody production to disease in neonatally infected mice. J. Exp. Med. 1969;129:483–505. doi: 10.1084/jem.129.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coutelier JP, Coulie PG, Wauters P, Heremans H, Logt JT. In vivo polyclonal B-lymphocyte activation elicited by murine viruses. J. Virol. 1990;64:5383–5388. doi: 10.1128/jvi.64.11.5383-5388.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunziker L, et al. Hypergammaglobulinemia and autoantibody induction mechanisms in viral infections. Nat. Immunol. 2003;4:343–349. doi: 10.1038/ni911. [DOI] [PubMed] [Google Scholar]
- 8.Yang L, et al. Evidence for B-lymphocyte mitogen activity in Borrelia burgdorferi-infected mice. Infect. Immun. 1992;60:3033–3041. doi: 10.1128/iai.60.8.3033-3041.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silverstein AM, Rose NR. On the implications of polyclonal B cell activation. Nat. Immunol. 2003;4:931–932. doi: 10.1038/ni1003-931. [DOI] [PubMed] [Google Scholar]
- 10.Lieby P, et al. Memory B cells producing somatically mutated antiphospholipid antibodies are present in healthy individuals. Blood. 2003;102:2459–2465. doi: 10.1182/blood-2003-01-0180. [DOI] [PubMed] [Google Scholar]
- 11.Schettino EW, Chai SK, Kasaian MT, Schroeder HW, Casali P. VHDJH gene sequences and antigen reactivity of monoclonal antibodies produced by human B-1 cells. J. Immunol. 1997;158:2477–2489. [PMC free article] [PubMed] [Google Scholar]
- 12.Dorner T, Egerer K, Feist E, Burmester GR. Rheumatoid factor revisited. Curr. Opin. Rheumatol. 2004;16:246–253. doi: 10.1097/00002281-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Koenig-Marrony S, et al. Natural autoreactive B cells in transgenic mice reproduce an apparent paradox to the clonal tolerance theory. J. Immunol. 2001;166:1463–1470. doi: 10.4049/jimmunol.166.3.1463. [DOI] [PubMed] [Google Scholar]
- 14.Julien S, Soulas P, Garaud JC, Martin T, Pasquali JL. B cell positive selection by soluble self-antigen. J. Immunol. 2002;169:4198–4204. doi: 10.4049/jimmunol.169.8.4198. [DOI] [PubMed] [Google Scholar]
- 15.Soulas P, et al. A role for membrane IgD in the tolerance of pathological human rheumatoid factor B cells. Eur. J. Immunol. 2002;32:2623–2634. doi: 10.1002/1521-4141(200209)32:9<2623::AID-IMMU2623>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 16.Wooten RM, Weis JJ. Host-pathogen interactions promoting inflammatory Lyme arthritis: use of mouse models for dissection of disease processes [review] Curr. Opin. Microbiol. 2001;4:274–279. doi: 10.1016/s1369-5274(00)00202-2. [DOI] [PubMed] [Google Scholar]
- 17.Zou YR, Muller W, Gu H, Rajewsky K. Cre-loxP-mediated gene replacement: a mouse strain producing humanized antibodies. Curr. Biol. 1994;4:1099–1103. doi: 10.1016/s0960-9822(00)00248-7. [DOI] [PubMed] [Google Scholar]
- 18.Barthold SW, Beck DS, Hansen GM, Terwilliger GA, Moody KD. Lyme borreliosis in selected strains and ages of laboratory mice. J. Infect. Dis. 1990;162:133–138. doi: 10.1093/infdis/162.1.133. [DOI] [PubMed] [Google Scholar]
- 19.McKisic MD, Barthold SW. T-cell-independent responses to Borrelia burgdorferi are critical for protective immunity and resolution of Lyme disease. Infect. Immun. 2000;68:5190–5197. doi: 10.1128/iai.68.9.5190-5197.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang FT, Nelson FK, Fikrig E. Molecular adaptation of Borrelia burgdorferi in the murine host. J. Exp. Med. 2002;196:275–280. doi: 10.1084/jem.20020770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wooten RM, et al. Toll-like receptor 2 is required for innate, but not acquired, host defense to Borrelia burgdorferi. J. Immunol. 2002;168:348–355. doi: 10.4049/jimmunol.168.1.348. [DOI] [PubMed] [Google Scholar]
- 22.Yang L, et al. Evidence for B-lymphocyte mitogen activity in Borrelia burgdorferi-infected mice. Infect. Immun. 1992;60:3033–3041. doi: 10.1128/iai.60.8.3033-3041.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma Y, Weis JJ. Borrelia burgdorferi outer surface lipoproteins OspA and OspB possess B-cell mitogenic and cytokine-stimulatory properties. Infect. Immun. 1993;61:3843–3853. doi: 10.1128/iai.61.9.3843-3853.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anguita J, et al. B7-1 and B7-2 monoclonal antibodies modulate the severity of murine Lyme arthritis. Infect. Immun. 1997;65:3037–3041. doi: 10.1128/iai.65.8.3037-3041.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolz DD, et al. MyD88 plays a unique role in host defense but not arthritis development in Lyme disease. J. Immunol. 2004;173:2003–2010. doi: 10.4049/jimmunol.173.3.2003. [DOI] [PubMed] [Google Scholar]
- 26.Alexopoulou L, et al. Hyporesponsiveness to vaccination with Borrelia burgdorferi OspA in humans and in TLR1- and TLR2-deficient mice. Nat. Med. 2002;8:878–884. doi: 10.1038/nm732. [DOI] [PubMed] [Google Scholar]
- 27.Takeuchi O, et al. Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins. J. Immunol. 2002;169:1–14. doi: 10.4049/jimmunol.169.1.10. [DOI] [PubMed] [Google Scholar]
- 28.Akira S, Takeda K. Toll-like receptor signalling [review]. Nat. Rev. Immunol. 2004;4:499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 29.Leadbetter EA, et al. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature. 2002;416:603–607. doi: 10.1038/416603a. [DOI] [PubMed] [Google Scholar]
- 30.Rui L, Vinuesa CG, Blasioli J, Goodnow CC. Resistance to CpG DNA-induced autoimmunity through tolerogenic B cell antigen receptor ERK signaling. Nat. Immunol. 2003;4:594–600. doi: 10.1038/ni924. [DOI] [PubMed] [Google Scholar]
- 31.Roosnek E, Lanzavecchia A. Efficient and selective presentation of antigen-antibody complexes by rheumatoid factor B cells. J. Exp. Med. 1991;173:487–489. doi: 10.1084/jem.173.2.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kouskoff V, et al. Organ-specific disease provoked by systemic autoimmunity. Cell. 1996;87:811–822. doi: 10.1016/s0092-8674(00)81989-3. [DOI] [PubMed] [Google Scholar]
- 33.Reed AJ, Riley MP, Caton AJ. Virus-induced maturation and activation of autoreactive memory B cells. J. Exp. Med. 2000;192:1763–1774. doi: 10.1084/jem.192.12.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Djavad N, et al. Comparison of rheumatoid factors of rheumatoid arthritis patients, of individuals with mycobacterial infections and of normal controls: evidence for maturation in the absence of an autoimmune response. J. Immunol. 1996;26:2480–2486. doi: 10.1002/eji.1830261031. [DOI] [PubMed] [Google Scholar]
- 35.Borretzen M, Chapman C, Natvig JB, Thompson KM. Differences in mutational patterns between rheumatoid factors in health and disease are related to variable heavy chain family and germ-line gene usage. Eur. J. Immunol. 1997;27:735–741. doi: 10.1002/eji.1830270323. [DOI] [PubMed] [Google Scholar]
- 36.Viglianti GA, et al. Activation of autoreactive B cells by CpG dsDNA. Immunity. 2003;19:837–847. doi: 10.1016/s1074-7613(03)00323-6. [DOI] [PubMed] [Google Scholar]
- 37.Stemmer C, et al. Dual reactivity of several monoclonal anti-nucleosome autoantibodies for double-stranded DNA and a short segment of histone H3. J. Biol. Chem. 1996;271:21257–21261. doi: 10.1074/jbc.271.35.21257. [DOI] [PubMed] [Google Scholar]
- 38.Cobbold SP, Martin G, Waldmann H. The induction of skin graft tolerance in major histocompatibility complex-mismatched or primed recipients: primed T cells can be tolerized in the periphery with anti-CD4 and anti-CD8 antibodies. Eur. J. Immunol. 1990;20:2747–2755. doi: 10.1002/eji.1830201232. [DOI] [PubMed] [Google Scholar]