Abstract
Respiratory syncytial virus (RSV) and human metapneumovirus (hMPV) cause a similar spectrum of respiratory infections in humans. Classified within the Paramyxoviridae family, Pneumovirinae subfamily, RSV and hMPV present a significant degree of divergence in genome constellation, organization, and protein sequences. RSV has been reported to be a poor inducer of alpha/beta interferons (IFN-α/β) and partially resistant to its antiviral activity. The nature of the innate immune response to hMPV is currently unknown. Herein, an experimental mouse model was used to investigate the interplay between RSV and hMPV infections and IFN-α in the airways. RSV-infected BALB/c mice treated intranasally with either poly-ICLC, a potent inducer of IFN-α, or directly with recombinant IFN-α showed significantly reduced lung viral titers, inflammation, and clinical disease than untreated controls. However, RSV was significantly less sensitive to the antiviral activity of IFN-α than hMPV. Similarly, when the ability to directly induce IFN-α production was assessed, RSV was clearly a weaker inducer of IFN-α than hMPV, as shown by both kinetics and the absolute amount of IFN-α secreted into the bronchoalveolar lavage. To further investigate the putative inhibitory effect of these viruses on IFN-α production, mice were infected for 48 h prior to treatment with poly-ICLC or a specific Toll-like receptor 9 ligand, CpG oligodeoxynucleotides. Strikingly, both poly-ICLC- and CpG-mediated IFN-α production was abrogated by either RSV or MPV infection. These results suggest that a complex interplay between virus-specific and host-mediated responses regulates IFN-α in the lung during infection by members of the Pneumovirinae family.
Respiratory syncytial virus (RSV) is the most common cause of viral lower respiratory tract infections leading to pneumonia in infants and children (11). In the absence of an effective vaccine for RSV, alternative prophylactic or treatment options are being actively pursued (e.g., polyclonal antibodies, monoclonal antibodies, antisense nucleotides, and viral inhibitors) (36). Interferons (IFNs) are a heterogeneous family of cytokines with demonstrated antiviral, antitumor, and immunomodulatory activities (3, 35). Local production of IFN-α/β plays an important defensive role in many respiratory virus infections by limiting viral replication until virus-specific host defense mechanisms develop (4). However, the role of IFN in RSV infection remains controversial.
Some laboratory strains of RSV have been reported to be sensitive to either nonviral IFN inducers such as synthetic double-stranded RNA or relatively impure preparations of IFN (16, 24). Other studies in fibroblast cell lines have shown that RSV is resistant to IFN-α2 and -β (51). In lung epithelial cells, IFN-β appears to restrict viral replication (40), but studies in which the susceptibility of RSV was compared to that of other respiratory viruses have suggested that RSV is relatively resistant to the effect of IFN-α/β (2). In children, little or no nasal interferon has been shown to be produced in the course of natural infections caused by RSV compared with those caused by other respiratory viruses (21, 39).
When IFN has been evaluated for possible treatment, the results have been controversial. One study reported that intramuscular treatment of RSV-infected children with IFN-α did improve their clinical course after the second day of treatment (53). On the other hand, Chipps et al. reported that children with bronchiolitis caused by RSV who were treated with intramuscular injection of IFN-α did not show significant difference in the clinical course, duration of oxygen requirement, or physical assessment compared to a placebo group. Likewise, no difference in the shedding of infectious virus in the nasal secretions was detected (10). In clinical trials involving experimental infections of adult volunteers with RSV, recombinant IFN-α2 given intranasally was shown to improve the clinical score when given prior to viral inoculation, but was not effective as a therapeutic agent (23).
In an experimental murine model of RSV infection, a role for IFN-α/β has recently been suggested by the observation of an increase of viral titer in the lung of IFN-nonresponsive STAT-1-deficient mice (12). The complex interplay between RSV and IFN is also suggested by studies in which the RSV nonstructural proteins NS1 and NS2 have been implicated in virus-induced inhibition of IFN-α/β (49, 56), viral susceptibility to IFN-α/β (45), and disease pathogenesis (61).
Human metapneumovirus (hMPV) is a recently identified RNA virus belonging to the Paramyxoviridae family, which includes several major human and animal pathogens. The Paramyxoviridae family is organized in two subfamilies, the Paramyxovirinae and the Pneumovirinae, the latter taxonomically divided into the Pneumovirus and Metapneumovirus genera. The classification of the two genera is based primarily on their gene constellation (13). Metapneumoviruses lack the nonstructural proteins NS1 and NS2, and the gene order is different from that of pneumoviruses. RSV is the type species of the Pneumovirus genus, while based on biological properties and genomic sequence, hMPV has been assigned to the Metapneumovirus genus.
Analysis of the sequences of all open reading frames, intergenic sequences, and partial sequence of the genomic termini has shown that hMPV has a higher percentage of sequence identity to avian pneumoviruses than to human or bovine RSV (57). For the N, P, M, F, M2-1, and M2-2 open reading frames of hMPV an overall aa identity of 80% with avian pneumovirus C and 18 to 41% with human RSV has been found (57). The close relationship between hMPV and avian pneumovirus C does not account for the host susceptibility, since avian pneumovirus infects birds, in contrast to hMPV. Indeed, a number of epidemiologic studies indicate that, similar to RSV, hMPV is a significant human respiratory pathogen with worldwide distribution (15, 26, 43). Both viruses appear to cause similar clinical manifestations (5, 32, 58) and affect many of the same subpopulations (27). Little is currently known regarding the immune response in the course of hMPV infection, including aspects of the innate immunity that involve production of IFN-α/β and whether distinct features exist between RSV and hMPV host responses.
In this study we have used an experimental mouse model to determine whether in vivo RSV and/or hMPV are sensitive to the antiviral activity of IFN-α, either induced by intranasal inoculation of poly-ICLC (stable form of synthetic double-stranded RNA) or directly administered in recombinant form; IFN-α has an effect on viral-induced clinical disease and lung inflammation; RSV or hMPV are able to induce endogenous IFN-α production in the airways; and RSV and hMPV are able to inhibit the production of IFN-α in the lung.
MATERIALS AND METHODS
RSV and hMPV preparations.
RSV A2 was grown in HEp-2 cells (American Type Culture Collection, Manassas, VA) and purified by polyethylene glycol precipitation, followed by centrifugation on 35 to 65% discontinuous sucrose gradients as described elsewhere (42, 55). The virus titer was determined by a methylcellulose plaque assay (30). The hMPV strain CAN97-83 was obtained from the Centers for Disease Control, Atlanta, GA, with permission from Guy Boivin at the Research Center in Infectious Diseases, Regional Virology Laboratory, Laval University, Quebec, Canada. Virus was propagated in LLC-MK2 cells (American Type Culture Collection) in minimal essential medium (without serum) containing 1 μg trypsin/ml, followed by purification on a 60% sucrose cushion. Virus titer was determined by a cell-based immunoassay. For that, sucrose-purified virus was serially diluted (log10) on LLC-MK2 cell monolayers in 96-well flat-bottom plates. Forty-eight hours later, monolayers were washed and incubated with guinea pig anti-hMPV antibody (kindly provided by MedImmune, Inc.) and stained with horseradish peroxidase-labeled anti-guinea pig antibody (Zymed, San Francisco, CA). Infected cells were detected using 3-amino-9-ethyl-carbazole, infectious units being enumerated by light microscopy.
Infection of mice and treatment protocol.
Female, 8- to 10-week-old BALB/c mice were purchased from Harlan (Houston, TX) and housed under pathogen-free conditions in the animal research facility of the University of Texas Medical Branch, Galveston, TX, in accordance with the National Institutes of Health and University of Texas Medical Branch institutional guidelines for animal care. Under light anesthesia, mice were treated intranasally with increasing doses of poly-ICLC (Oncovir, Inc., Washington, DC) or murine recombinant IFN-α (rIFN-α) (a kind gift of Sidney Pestka and William Clark, PBL Biomedical Laboratories) or with control diluent. Twenty-four hours later, mice were infected intranasally with 50 μl of RSV diluted in phosphate-buffered saline (final administered dose: 107 PFU) (20). Control mice were inoculated with the same volume of culture medium (referred to hereafter as sham infection). In some experiments, mice were first infected with RSV and 72 h later they were treated with 104 IU of rIFN-α.
In a separate set of experiments, mice were first infected with RSV or hMPV for 48 h and subsequently treated with either 10 μg/mouse of poly-ICLC or 30 μg/mouse of a synthetic phosphorothioate-modified CpG oligodeoxynucleotide (ODN). The synthetic CpG-ODN (5′-GCTAGACGTTAGCGT-3′) was synthesized by Sigma-Genosys (The Woodlands, TX). Similar to the RSV infection protocol, mice were then infected intranasally with 50 μl of sucrose-purified hMPV (107 PFU). At the indicated time points (see Results) mice were anesthetized with an intraperitoneal injection of ketamine and xylazine before the thoracic cavity was opened. The mice were exsanguinated and the trachea was opened by incision of the cricothyroid membrane.
To collect a bronchoalveolar lavage (BAL), the lungs were flushed twice with ice-cold sterile minimal essential medium (1 ml) containing 2% fetal bovine serum. BAL fluid was centrifuged and stored at −70°C until analysis. Lungs were removed for RSV or hMPV titration, IFN determination, or histopathology (see below). For RSV titration, the lungs were homogenized in 1 ml of Dulbecco's modified Eagle's medium. Homogenized samples were centrifuged twice at 10,000 × g for 1 min. Serial twofold dilutions of the supernatant were tested by a methylcellulose plaque assay (30). For hMPV titration, serial twofold serial dilutions of lung homogenates were titrated in LLC-MK2 cell monolayers in 96-well flat-bottomed plates (as described for virus stock preparation). The theoretical limit of detection of these assays was 10 and 25 PFU/g of lung tissue for RSV and hMPV, respectively.
Illness score and body weight.
The severity of illness in mice was scored daily by two investigators using a standardized 1 to 5 grading system as follows: 0, healthy; 1, barely ruffled fur; 2, ruffled fur but active; 3, ruffled fur and inactive; 4, ruffled fur, inactive and hunched; and 5, dead (18). In addition, daily determination of body weight was used to monitor the progression of disease.
IFN measurement in BAL and lung tissue.
The IFN-α concentration in BAL was determined by a commercial enzyme-linked immunosorbent assay (ELISA) (PBL Biomedical Laboratories, Piscataway, NJ), according to the manufacturer's instructions. The range of sensitivity of the assay is 12.5 to 500 pg/ml. IFN bioactivity in BAL, lung, or serum was determined by a standard microtiter plaque reduction assay using vesicular stomatitis virus on murine fibroblast L-929 cells, as described previously (33). For comparison, 1 IU of bioactive IFN-α is equal to ≈10 to 20 pg of IFN-α by ELISA (28). For IFN-α determination in lung tissue, lungs were collected and processed exactly as described for viral titration.
Pulmonary histopathology.
Lungs were perfused and fixed in 10% buffered formalin and embedded in paraffin. Multiple 4 μm-thick sections were stained with hematoxylin and eosin. Slides were analyzed and scored for cellular inflammation under light microscopy by two independent pathologists, as previously described (20, 52). Briefly, inflammatory infiltrates were scored by enumerating the layers of inflammatory cells surrounding the vessels and bronchioles. Finding zero to three layers of inflammatory cells was considered normal. Finding moderate to abundant infiltrate (more than three layers of inflammatory cells surrounding 50% or more of the circumference of the vessel or bronchioles) was considered abnormal. The number of abnormal perivascular and peribronchial spaces divided by the total perivascular and peribronchial spaces was the percentage reported as the pathology score.
Statistical analysis.
Statistical analyses were performed with the InStat 3.05 biostatistics package (GraphPad, San Diego, CA) using a two-tailed, unpaired Student's t test. Unless otherwise indicated, mean ± standard error of the mean is shown.
RESULTS
Induction of IFN-α/β in the lung of mice treated with poly-ICLC.
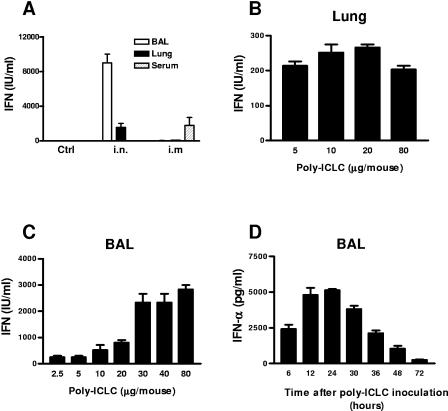
Initial experiments were conducted to identify an appropriate route of administration of poly-ICLC capable of inducing IFN production in the lung of mice. In these experiments, IFN concentrations (IU/ml) were determined by a standard bioassay (33). While intramuscular injection of poly-ICLC resulted in the appearance of IFN in serum only, a single intranasal application induced levels of IFN that were measurable both in the lung tissue and in the BAL fluid (Fig. 1A). A dose-response was also established using increasing doses of poly-ICLC. In general, doses of poly-ICLC below 20 μg were well tolerated by the mice, i.e., no signs of systemic toxicity (assessed by body weight loss or illness score). A dose-dependent response in IFN production (at 24 h) was observed, both in lung tissue (Fig. 1B) and in BAL (Fig. 1C), which appeared to plateau at doses of poly-ICLC of 20 to 30 μg (Fig. 1B and 1C).
FIG. 1.
Poly-ICLC induces IFN-α/β in mice. IFN was measured in BALB/c mice treated with poly-ICLC. (A) Mice were treated either intranasally or intramuscularly with 80 μg of poly-ICLC, and IFN-α/β bioactivity was measured in BAL, lung, and serum by a standard microtiter plaque reduction assay. Dose response: increasing doses of poly-ICLC were instilled intranasally in mice. IFN-α/β bioactivity was detected in (B) lung tissue and (C) BAL. (D) IFN-α concentration was measured by ELISA at different time points in BAL fluid of mice treated intranasally with 10 μg of poly-ICLC. The bar graph represents mean ± standard error of the mean (n = 4 mice/group).
Neutralization experiments using National Institutes of Health reference antisera showed that poly-ICLC-induced IFN bioactivity in the lung was due to IFN-α/β (data not shown). The dose of 10 μg was then chosen for subsequent studies, in which a detailed kinetics of poly-ICLC-induced IFN was determined in BAL fluid by an ELISA specific for IFN-α. By this ELISA, 10 to 20 pg of IFN-α are equal to 1 IU of bioactive IFN-α. As shown in Fig. 1D, IFN-α was detected in BAL as early as 6 h following poly-ICLC inoculation, reached peak concentrations between 12 and 24 h, and gradually declined over the next 48 h.
Treatment with poly-ICLC inhibits RSV replication and ameliorates disease and lung inflammation.
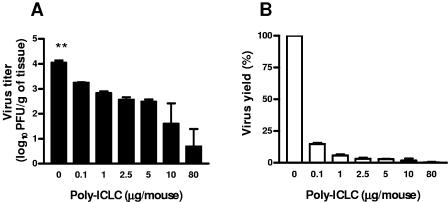
Having established a mouse model characterized by high levels of inducible IFN-α/β in the lung allowed us to investigate whether RSV was susceptible to IFN activity in vivo. For that, groups of BALB/c mice were treated with increasing doses of poly-ICLC, ranging from 0.1 to 80 μg/mouse, or control medium, and 24 h later infected with RSV. As direct measure of the inhibitory effect of poly-ICLC-induced IFN on RSV replication we determined peak viral titer in the lung of mice at day 5 after inoculation. A significant reduction in viral titers compared to control treatment (medium) was observed for each of the poly-ICLC concentration tested (Fig. 2A), with a reduction that ranged from 85% at a dose of 0.1 μg to >99% at 10 and 80 μg (Fig. 2B).
FIG. 2.
Dose-dependent inhibition of RSV replication by poly-ICLC. Groups of BALB/c mice were treated intranasally with increasing doses of poly-ICLC and 24 h later were infected with RSV (107 PFU/mouse). (A) Lung viral titer: 5 days after infection lung tissue was removed, and the viral titer was determined by a methylcellulose plaque assay. (B) Virus yield for each dose of poly-ICLC used is expressed as a percentage of the control and calculated as [(virus titer with poly-ICLC)/(virus titer without poly-ICLC)] × 100. The bar graph represents mean ± standard error of the mean (n = 3 to 12 mice/group). **, P < 0.01 compared with poly-ICLC-treated mice (at each dose).
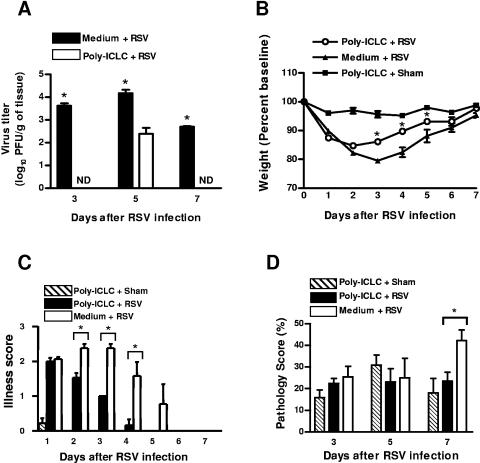
Further experiments were conducted to examine the effect of poly-ICLC-induced IFN on RSV replication at different time points in the course of infection and disease (both clinical disease and lung inflammation). A dose of 10 μg of poly-ICLC was selected for these studies. Groups of RSV-infected mice were treated with poly-ICLC or control vehicle under the protocol mentioned above and either assessed daily for body weight loss and clinical illness score or sacrificed at different time points (days 3, 5, and 7) for determination of lung viral titer and lung histopathology. As shown in Fig. 3A, RSV replication in the lung was virtually abolished in poly-ICLC-treated mice at day 3 or 7 and was reduced by ≈99% at day 5, thus extending our previous findings in the dose-response studies. In addition, infected mice treated with poly-ICLC showed a smaller but statistically significant reduction in body weight loss between days 3 and 5 compared to infected controls treated with vehicle (Fig. 3B). Similarly, clinical disease (estimated by an illness score) appeared to be less severe in poly-ICLC-treated mice than controls (Fig. 3C). As previously mentioned, poly-ICLC given alone to mice in the dose of 10 μg had minimal and transient adverse and toxic effects (Fig. 3B and C).
FIG. 3.
Poly-ICLC treatment in RSV-infected mice. BALB/c mice were inoculated with 10 μg of poly-ICLC and 24 h later infected with RSV. (A) Lung viral titer was determined 3, 5, and 7 days after RSV infection (n = 3 mice/group). ND, not detectable. (B) Body weight and (C) illness score were evaluated daily (n = 6 to 15 mice/group). (D) Pathology score was assessed in lung tissue preparations stained with hematoxylin and eosin (n = 3 mice/group). Graphs represent mean ± standard error of the mean. *, P < 0.05 compared with poly-ICLC-treated mice.
To determine whether treatment with poly-ICLC affects lung inflammation, groups of mice were sacrificed at 3, 5 and 7 days following RSV inoculation and hematoxylin and eosin-stained lung sections were analyzed and scored for inflammation (Fig. 3D) (20, 52). In sham-infected mice no lung inflammation was detected (data not shown). While at days 3 and 5 no significant difference in the degree of inflammation was observed between RSV-infected mice that received poly-ICLC or control vehicle, at day 7 postinfection we consistently observed reduced inflammation in infected mice treated with poly-ICLC compared with those treated with vehicle (P < 0.05). Given the fact that poly-ICLC treatment by itself (in absence of RSV) appeared to induce some degree of inflammation in the lung, particularly at day 5, a “protective” effect of IFN on RSV-induced inflammation may have been underestimated in these experimental conditions. This assumption is supported by the our later experiments in which rIFN-α was directly inoculated in RSV-infected mice (see Fig. 5B). The overall results are suggestive of a milder disease and/or faster recovery in RSV-infected mice as result of poly-ICLC-induced IFN production and reduced viral replication.
FIG. 5.
Viral replication and lung inflammation are reduced in mice treated with IFN-α following RSV inoculation. BALB/c mice were infected with RSV and 3 days later were treated intranasally with 104 IU of rIFN-α. (A) Two days after IFN-α treatment (i.e., 5 days after viral inoculation), lung tissue was removed and lung viral titer was determined. (B) Pathology score was determined at day 7 after RSV infection. Bar graphs represent mean ± standard error of the mean (n = 3 mice/group). *, P < 0.05 compared with untreated infected mice.
Reduced RSV replication and clinical disease in mice pretreated with IFN-α.
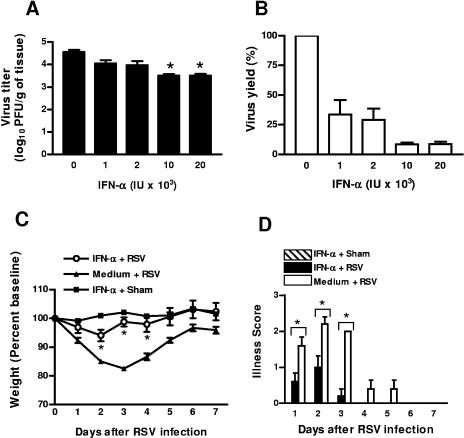
To directly test the effect of IFN-α on RSV replication in the lung, groups of mice were treated intranasally with increasing doses of murine rIFN-α (1 × 103 to 2 × 104 IU/mouse) and 24 h later were infected with RSV. Peak viral titer in the lung was determined at day 5 after infection exactly as described for poly-ICLC. All groups of RSV-infected mice that were treated with rIFN-α showed reduction in RSV replication compared with the vehicle-treated group (Fig. 4A). Compared to the control treatment, the percent reduction in lung viral titer in IFN-treated mice ranged from 66% at a dose of 103 IU to a maximum of ≈91% with doses of 1 × 104 and 2 × 104 IU (P < 0.05) (Fig. 4B). In addition, pretreatment of RSV-infected mice with IFN-α (104 IU) resulted in a significant improvement in clinical disease as shown both by body weight loss and illness scores (Fig. 4C and D). No toxic effect was observed at any of the doses of IFN-α per se (see Fig. 4C, IFN-α + Sham). Taken together, these results suggest that pretreatment with IFN-α indeed has an impact not only on viral replication but also on clinical disease during RSV infection.
FIG. 4.
Reduction of RSV replication and clinical disease in mice pretreated with recombinant IFN-α. Groups of BALB/c mice were treated intranasally with increasing doses of murine rIFN-α and 24 h later were infected with RSV. Five days after RSV infection, lung tissue was removed and homogenized and the viral titer was determined by a methylcellulose plaque assay. (A) Lung viral titer. (B) Virus yield (n = 3 mice/group). (C) Body weight and (D) illness score were evaluated daily (n = 5 mice/group). Graphs represent mean ± standard error of the mean. *, P < 0.05 compared with untreated infected mice.
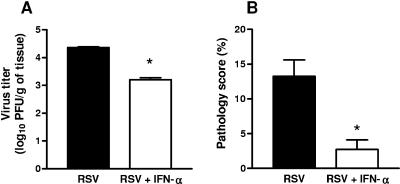
Treatment with IFN-α following RSV infection reduces viral replication and lung inflammation.
The experiments described in the previous sections have utilized a model in which treatment of mice with either poly-ICLC or IFN-α preceded virus inoculation. To examine the potential “therapeutic” effect of IFN-α, BALB/c mice were first infected with RSV and 3 days later were treated with rIFN-α (104 IU/mouse). Two and 4 days after IFN-α inoculation (i.e., 5 and 7 days after RSV infection) lung tissue was collected to determine peak viral titers and lung inflammation, respectively. As shown in Fig. 5A, viral replication was reduced by more than 14-fold (≈93%) in RSV-infected mice treated with IFN-α compared with infected mice treated with control vehicle. In addition, RSV-infected animals treated with IFN-α showed a significant reduction in the pathology score compared with controls (Fig. 5B). These results suggest that IFN-α has some beneficial effects when given after the onset of RSV infection.
hMPV is more susceptible than RSV to the antiviral activity of IFN-α.
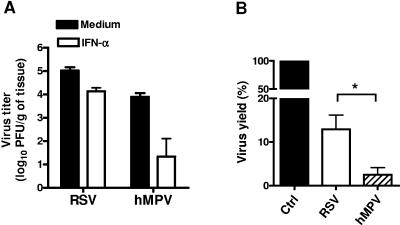
For a better understanding of the relative extent of susceptibility of RSV to the antiviral activity of IFN-α, we sought to compare it with hMPV, a recently discovered member of the Pneumovirinae family. For that, groups of mice were treated intranasally with rIFN-α (104 IU/mouse) and 24 h later infected with either RSV or hMPV. Peak viral titer in the lung was determined at day 5 after infection exactly as previously described. Following treatment with IFN-α a significant greater reduction in viral titer was observed in hMPV-infected mice than in RSV-infected ones (relative to untreated controls) (Fig. 6A). The reduction in lung viral titer in IFN-treated mice compared with controls was 87% and 97.5% for RSV and hMPV, respectively. Similar results were obtained when samples of hMPV-infected lungs were titrated by a 50% tissue culture infectious dose assay (data not shown). These results suggest a greater susceptibility to IFN-α for hMPV compared to RSV (Fig. 6B) (P < 0.05).
FIG. 6.
Susceptibility of hMPV and RSV to rIFN-α. Groups of BALB/c mice were treated intranasally with 104 IU of murine rIFN-α and 24 h later were infected with hMPV or RSV. Five days after infection, lung tissue was removed and homogenized and the viral titer was determined by immunostaining (hMPV) or a methylcellulose plaque assay (RSV). (A) Lung viral titer. (B) Virus yield. The bar graph represents mean ± standard error of the mean (n = 4 mice/group). *, P < 0.05.
IFN-α production in the course of infection with RSV or hMPV.
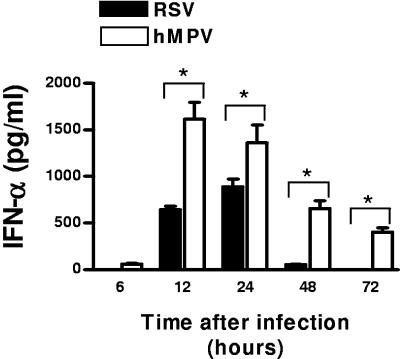
The results presented so far indicate that providing a source of IFN-α, either by administering poly-ICLC or rIFN-α directly, reduced viral replication and ameliorated disease in RSV-infected mice. We next tested in our experimental model whether RSV by itself was able to induce IFN-α production in the lung and compared it with hMPV. The results of these experiments are shown in Fig. 7. Detectable levels of IFN-α appeared in the BAL fluid of RSV-infected mice as early as 12 h after inoculation, peaked at 24 h, and then declined to levels below 50 pg/ml by 48 h. The concentrations of IFN-α measured by ELISA correlated with IFN bioactivity (data not shown). The concentrations of IFN-α in BAL were significantly lower at each time point tested in RSV-infected mice compared to hMPV-infected ones. In addition, hMPV-infected mice had detectable levels of IFN-α in BAL fluids at earlier time points than RSV-infected mice as well as sustained production at 48 and 72 h (Fig. 7). Interestingly, UV-inactivated preparations of RSV or hMPV did not induce detectable IFN-α in BAL at any time point tested, suggesting that viral replication is necessary for IFN-α production (data not shown). Overall, these results indicate that hMPV is a stronger inducer of IFN-α in vivo than RSV.
FIG. 7.
IFN-α production in lungs of mice infected with RSV or hMPV. BALB/c mice were infected with either RSV or hMPV (both at 107 PFU) and production of IFN-α was measured by ELISA in BAL samples at different time points. The bar graph represents mean ± standard error of the mean (n = 3 to 5 mice/group/time point). *, P < 0.05.
Viral inhibition of poly-ICLC- and CpG-induced IFN-α production.
There is compelling evidence in vitro that both human and bovine RSVs interfere with intracellular pathways leading to IFN production. In certain cell types such as epithelial cells and macrophages the mechanism(s) of this inhibition appears to be dependent on expression of the nonstructural viral proteins NS1 and NS2 (49, 56). Moreover, recent evidence suggests that RSV is able to block interferon production in human plasmacytoid dendritic cells by inhibiting the Toll-like receptor 7 (TLR7) and TLR9 signaling pathways (46).
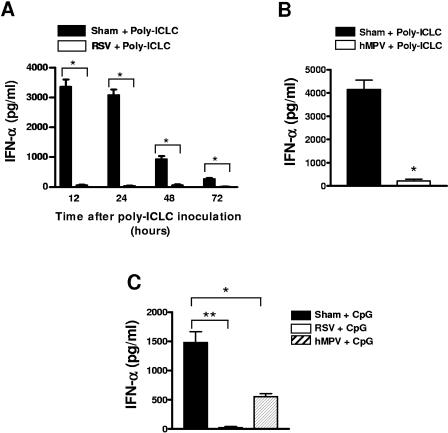
To the best of our knowledge, there are no studies that have examined whether RSV is capable of inhibiting IFN production in vivo and whether this event occurs also in the course of hMPV infection. Therefore, we determined whether RSV and/or hMPV infection was able to inhibit IFN-α production induced by intranasal application of poly-ICLC or a synthetic CpG-ODN, a well-characterized TLR9 ligand (22, 31). Groups of mice were infected with RSV or hMPV or sham infected and 48 h later were treated with poly-ICLC or CpG-ODN. BAL samples were collected at different time points after poly-ICLC or CpG-ODN treatment for measurement of IFN-α.
As shown in Fig. 8A, at all time points following poly-ICLC treatment (12, 24, 48, and 72 h), the concentrations of IFN-α were below the limit of detection in BAL fluids of RSV-infected mice, clearly indicating that production of IFN-α was severely impaired in mice that were infected with RSV compared to sham controls (Fig. 8A). A similar inhibitory effect on IFN-α production was observed when mice were infected with hMPV prior to poly-ICLC treatment (24 h) (Fig. 8B). In the next series of experiments, treatment of control mice with CpG-ODN (30 μg/mouse) induced a robust production of IFN-α that was detected in BAL fluid samples 24 h after intranasal application (Fig. 8C, sham + CpG). Strikingly, infection of mice with RSV or hMPV resulted in almost complete inhibition of CpG-induced IFN-α production (Fig. 8C). Overall, these results provide novel evidence in vivo that RSV and hMPV are able to inhibit IFN-α production induced by two distinct agonists, poly-ICLC and the TLR9 ligand CpG-ODN.
FIG. 8.
RSV and hMPV inhibit poly-ICLC- and CpG-induced IFN-α production. BALB/c mice were infected with RSV or hMPV and 48 h later were treated intranasally with either poly-ICLC or CpG-ODN. IFN-α concentrations were measured in BAL samples collected at different time points. (A) Poly-ICLC-induced IFN-α in RSV-infected mice (n = 3 to 5 mice/group/time point). (B) Poly-ICLC-induced IFN-α in hMPV-infected mice (n = 3 mice/group). (C) CpG-induced IFN-α in RSV- or hMPV-infected mice (n = 4 mice/group). The bar graph represents mean ± standard error of the mean. *, P < 0.05, and **, P < 0.01, compared with treated infected mice.
DISCUSSION
This study provides evidence that both RSV and hMPV are sensitive to the antiviral activity of IFN-α, although hMPV appears to be more susceptible than RSV. Furthermore, RSV appears to be a weaker inducer of IFN-α production than hMPV, but both RSV and hMPV infections equally interfere with the IFN pathway, leading to a dramatic inhibition of poly-ICLC- and CpG-induced IFN-α production in the lung. To test for IFN activity on RSV infection in vivo, we have used an experimental mouse model in which we induced IFN production in the lung. The susceptibility of RSV to the antiviral effect of IFN-α was observed when poly-ICLC was given at doses as low as 0.1 μg/mouse (Fig. 2A), leading to reduction of lung viral titers in RSV-infected mice. In addition to reduction in viral replication, treatment of mice with poly-ICLC resulted in an amelioration of the clinical illness and a reduction in lung inflammation (Fig. 3).
To further corroborate the specific role of IFN, we directly assessed RSV susceptibility to IFN activity by treating mice with rIFN-α prior to or following viral inoculation. The results demonstrate a significant reduction in viral replication and disease severity in IFN-α-treated mice, where the animals recovered faster and lost less body weight than untreated mice (Fig. 4). Reduction in RSV yield in IFN-treated mice was observed not only when the IFN treatment occurred prior to viral inoculation but also after the infection was established (Fig. 5). Overall, treatment with poly-ICLC resulted in a more dramatic effect on RSV replication (≈99% inhibition) than on clinical disease (body weight loss and illness score), while treatment with IFN-α was more effective in improving clinical disease than in reducing RSV replication.
The complex network of genes with both antiviral and proinflammatory activity which are induced by poly-ICLC (i.e., synthetic double-stranded RNA) in the airways was likely responsible for the very effective reduction of RSV replication, yet the less evident effect on clinical disease by this treatment (1). In fact, as we noted in the Results section, poly-ICLC treatment by itself appeared to induce some degree of inflammation in the lung, particularly at day 5 (Fig. 3D). On the other hand, the results observed with the direct IFN-α treatment suggest that IFN may improve RSV-induced disease by additional immune-type mechanisms. Among those, IFN-α/β has been shown to activate immature dendritic cells, to affect generation of CD8+ T cells, and to stimulate antibody responses (9, 34, 38). Alternatively, the more effective antiviral activity observed with poly-ICLC treatment may be due to a greater biological activity or bioavailability of endogenously produced IFN-α than of the exogenous recombinant form.
For a better understanding of the relative degree of sensitivity of RSV to the antiviral activity of IFN, we directly compared the sensitivity of RSV and hMPV to IFN-α. Our results show that in mice treated with rIFN-α prior to infection, viral yield in the lung was smaller for hMPV than for RSV, suggesting that hMPV is more susceptible than RSV to the antiviral effect of IFN-α (Fig. 6). We speculate that the RSV nonstructural proteins NS1 and NS2, which are not expressed by hMPV, could play a role in this phenomenon. Indeed, it has been shown that the NS1 and NS2 proteins mediate some resistance to the antiviral action of IFN-α/β in vitro (6, 45). Additional mechanisms responsible for these differences in susceptibility to IFN-α activity cannot be ruled out at present.
RSV has been reported to be a poor inducer of IFN-α/β (21, 39). However, there is limited information on the in vivo production of IFN-α by RSV in highly controlled experimental models. In this study, we tested the ability of RSV to induce IFN-α in mice and compared it with that of hMPV. We observed a peak of IFN-α production as early as 24 h after RSV infection, but this induction decreases by 48 h, and by 72 h the amount of IFN-α induced by RSV reached undetectable levels. On the other hand, in animals infected with hMPV, IFN-α was consistently detected in small concentrations as early as 6 h after infection, the production reached a peak between 12 and 24 h and was sustained up to 72 h returning to basal levels by day 5 (Fig. 8). IFN-α in BAL was detected in significantly higher amounts in hMPV-infected mice than RSV-infected mice at all time points tested. The mechanism(s) responsible for the observed difference in the level and kinetics of IFN-α production in the lung following infection with RSV or hMPV is currently unknown. As mentioned in relation to the viral susceptibility to IFN-α/β, it is possible the RSV NS1 and NS2 proteins play a pivotal role in limiting IFN-α/β production in vivo. This hypothesis is supported by recent studies in which treatment of mice with a short interfering RNA targeting the NS1 gene of RSV resulted in higher IFN-α/β production in the lung (61).
To further investigate the putative inhibitory effect of RSV and hMPV infections on IFN-α production in vivo, mice were infected with RSV or hMPV and inoculated 48 h later with poly-ICLC. As shown in Fig. 8, poly-ICLC-mediated IFN-α production was completely suppressed by RSV or hMPV infection, suggesting that both these members of the Pneumovirinae family are able to interfere with signaling pathways that lead to IFN production in the lung. The induction of IFN-α/β production is primarily controlled at the transcriptional level, wherein the IFN regulatory factor (IRF) family of transcription factors play an essential role (54). In addition, NF-κB and AP-1 are also a component of the so called “enhanceosome,” a transcriptional enhancer complex, which controls the transcription of the IFN-α/β gene (37). Depending on the cell type and the conditions that lead to its generation, the initial steps involved in double-stranded RNA-induced IFN-α/β production include two intracellular sensors, the IFN-inducible double-stranded RNA-activated protein kinase R (PKR) and the recently discovered RNA helicase, retinoic acid-inducible gene I (RIG-I) (59, 60). Following binding to double-stranded RNA, PKR dimerizes, becomes activated via autophosphorylation, and interacts with proteins of the tumor necrosis factor receptor-associated factor (TRAF) family, which in turn trigger activation of IKK and NF-κB (17). While PKR also activates the p38 mitogen-activated protein kinase pathway, the activation of IRF-3 does not seem to be a downstream target of PKR (reviewed in reference 41). On the other hand, binding of RIG-I by double-stranded RNA has been shown to activate both NF-κB and IRF-3 (60).
In addition to PKR and RIG-I, double-stranded RNA (also in the form of the analogue synthetic poly-ICLC) activates TLR3, which is expressed predominantly in the cellular endosomal compartment (1). Via the adaptor protein TRIF and the activation of the IκB kinase ɛ and TANK-binding kinase 1, the double-stranded RNA/TLR3-activated pathway converges on the phosphorylation and activation of IRF-3, which is required for induction of the IFN-α/β gene (14, 44, 48). Given the complex regulation of IFN-α/β in vivo, RSV and hMPV infections could interfere with multiple signal transduction pathways in a virus-specific manner, leading to IFN gene transcription in the lung.
There are some considerations that need to be addressed in our attempt to dissect these potential mechanisms. First, in our work the inhibitory effect of RSV and hMPV appears to affect not only double-stranded RNA- but also CpG-mediated IFN production in the lung. Interestingly, inhibition of CpG-mediated IFN production by human RSV and hMPV has been observed in purified peripheral blood plasmacytoid dendritic cells (46; A. Guerrero-Plata et al., submitted for publication). CpG-ODN binds to TLR9 in the endosomal compartment (22) and similarly to TLR7/8 (also expressed in the cell endosomes), activates IFN production via a mechanism that requires the adaptor molecules MyD88, IRAK-1, and TRAF6 (47). In this pathway, IRF-5 and IRF-7, rather than IRF-3, appear to be activated (29, 47). IRF-7 in particular has been shown to be a master regulator of murine IFN-α/β production, as mice deficient in the irf7 gene are severely impaired in the production of IFN-α/β triggered by both MyD88-dependent and MyD88-independent pathways (25). Recent work in cultured epithelial cells suggested that human RSV is capable of suppressing activation and nuclear translocation of IRF-3 early in the course of infection (10 to 14 h) (50). However, this was not observed in studies by other investigators (7, 8). When this putative effect of RSV on IRF-3 inhibition was observed, infection of cells with RSV mutants lacking the NS1 and NS2 proteins resulted in more sustained IRF-3 activation than the wild-type parent virus (50). We are currently investigating whether RSV and/or hMPV infection in the lung is able to interfere with the induction or activation of IRF proteins, including IRFs 5 and 7, as well as other signal transduction pathways that control IFN-α/β gene expression.
A second consideration is that the similar inhibitory effect of RSV and hMPV on IFN-α production observed in vivo in the present work and in our in vitro studies of plasmacytoid dendritic cells (A. Guerrero-Plata et al., submitted) points to the fact that these two viruses, which have considerable genomic and structural diversity, employ distinct virus-specific mechanisms to interfere with IFN-α production. In the case of hMPV, this putative mechanism(s) of IFN inhibition would not be obviously linked to the expression of the NS proteins as it might in the course of RSV infections. Members of the Paramyxoviridae family have indeed developed distinct mechanisms to antagonize the effect of the IFN response in order to survive the host innate defense and enhance their pathogenesis potential.
As a final consideration, we cannot exclude that the effector mechanism responsible for the dramatic inhibition of RSV and hMPV on poly-ICLC- and CpG-induced IFN-α production may be an unidentified soluble factor(s) which is secreted in the lung in the course of infection. Indeed, it seems unlikely that all or most of the cells potentially responding to the IFN-inducing agents in the mouse airways would be infected by RSV or hMPV. In fact, although the type of cells that produce IFN-α/β in the lung in response to double-stranded RNA or CpG-ODN treatment remains to be defined, the characteristics of RSV as well as hMPV experimental infection suggest a rather patchy and limited distribution of viral antigen in the mouse airways (19; A. Casola, personal communication).
In conclusion, the results described in this study indicate the existence of a complex interplay between infections caused by the paramyxoviruses RSV and hMPV and the antiviral activity and regulatory pathways of IFN-α production in the lung. New information is provided on innate immune mechanisms in the course of hMPV infection. Finally, our findings suggest that a careful reexamination of antiviral strategies for treating RSV infections based on IFN-α may be worthwhile in future trials.
Acknowledgments
We thank Allan R. Brasier (UTMB) for helpful discussions and Xiang Yu and LeAnne Spetch for technical assistance.
This work was supported by NIAID grant AI053785 and American Heart Association grant 0355084Y (R. P. Garofalo). A. Guerrero-Plata was supported by a fellowship from the James W. McLaughlin Fellowship Fund.
REFERENCES
- 1.Alexopoulou, L., A. C. Holt, R. Medzhitov, and R. A. Flavell. 2001. Recognition of double-stranded RNA and activation of NF-kappaB by Toll-like receptor 3. Nature 413:732-738. [DOI] [PubMed] [Google Scholar]
- 2.Atreya, P. L., and S. Kulkarni. 1999. Respiratory syncytial virus strain A2 is resistant to the antiviral effects of type I interferons and human MxA. Virology 261:227-241. [DOI] [PubMed] [Google Scholar]
- 3.Baron, S., I. Singh, A. Chopra, D. Coppenhaver, and J. Pan. 2000. Innate antiviral defenses in body fluids and tissues. Antiviral Res. 48:71-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biron, C., and G. C. Sen. 2001. Interferons and Other Cytokines, p. 321-351. In D. M. Knipe and P. M. Howley (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 5.Boivin, G., Y. Abed, G. Pelletier, L. Ruel, D. Moisan, S. Cote, T. C. Peret, D. D. Erdman, and L. J. Anderson. 2002. Virological features and clinical manifestations associated with human metapneumovirus: a new paramyxovirus responsible for acute respiratory-tract infections in all age groups. J Infect. Dis. 186:1330-1334. [DOI] [PubMed] [Google Scholar]
- 6.Bossert, B., and K. K. Conzelmann. 2002. Respiratory syncytial virus (RSV) nonstructural (NS) proteins as host range determinants: a chimeric bovine RSV with NS genes from human RSV is attenuated in interferon-competent bovine cells. J. Virol. 76:4287-4293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casola, A., N. Burger, T. Liu, M. Jamaluddin, A. R. Brasier,, and R. P. Garofal. 2001. Oxidant tone regulates RANTES gene transcription in airway epithelial cells infected with respiratory syncytial virus: role in viral-induced interferon regulatory factor activation. J. Biol. Chem. 276:19715-19722. [DOI] [PubMed] [Google Scholar]
- 8.Casola, A., R. P. Garofalo, H. Haeberle, T. F. Elliott, A. Lin, M. Jamaluddin, and Brasier, A. R. 2001. Multiple cis regulatory elements control RANTES promoter activity in alveolar epithelial cells infected with respiratory syncytial virus. J. Virol. 75:6428-6439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cella, M., M. Salio, Y. Sakakibara, H. Langen, I. Julkunen, and A. Lanzavecchia. 1999. Maturation, activation, and protection of dendritic cells induced by double-stranded RNA. J. Exp. Med. 189:821-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chipps, B. E., W. F. Sullivan, and J. M. Portnoy. 1993. Alpha-2A-interferon for treatment of bronchiolitis caused by respiratory syncytial virus. Pediatr. Infect. Dis. J. 12:653-658. [DOI] [PubMed] [Google Scholar]
- 11.Collins, P. L., K. McIntosh, and R. M. Chanock. 1996. Respiratory syncytial virus, p. 1313-1351. In B. N. Fields, D. M. Knipe, and P. M. Howley (ed.), Fields virology. Lippincott-Raven Publishers, Philadelphia, Pa.
- 12.Durbin, J. E., T. R. Johnson, R. K. Durbin, S. E. Mertz, R. A. Morotti, R. S. Peebles, and B. S. Graham. 2002. The role of IFN in respiratory syncytial virus pathogenesis. J. Immunol. 168:2944-2952. [DOI] [PubMed] [Google Scholar]
- 13.Easton, A. J., J. B. Domachowske, and H. F. Rosenberg. 2004. Animal pneumoviruses: molecular genetics and pathogenesis. Clin. Microbiol. Rev. 17:390-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzgerald, K. A., S. M. McWhirter, K. L. Faia, D. C. Rowe, E. Latz, D. T. Golenbock, A. J. Coyle, S. M. Liao, and T. Maniatis. 2003. IKKepsilon and TBK1 are essential components of the IRF3 signaling pathway. Nat. Immunol. 4:491-496. [DOI] [PubMed] [Google Scholar]
- 15.Freymouth, F., A. Vabret, L. Legrand, N. Eterradossi, F. Lafay-Delaire, J. Brouard, and B. Guillois. 2003. Presence of the new human metapneumovirus in French children with bronchiolitis. Pediatr. Infect. Dis. J. 22:92-94. [DOI] [PubMed] [Google Scholar]
- 16.Gardner, P. S., R. McGuckin, A. Beale, and R. Fernandes. 1970. Interferon and respiratory syncytial virus. Lancet i:574-575. [DOI] [PubMed] [Google Scholar]
- 17.Gil, J., M. A. Garcia, P. Gomez-Puertas, S. Guerra, J. Rullas, H. Nakano, J. Alcami, and M. Esteban. 2004. TRAF family proteins link PKR with NF-κB activation. Mol. Cell. Biol. 24:4502-4512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graham, B. S., L. A. Bunton, P. F. Wright, and D. T. Karzon. 1991. Role of T lymphocyte subsets in the pathogenesis of primary infection and rechallenge with respiratory syncytial virus in mice. J. Clin. Investig. 88:1026-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham, B. S., M. D. Perkins, P. F. Wright, and D. T. Karzon. 1988. Primary respiratory syncytial virus infection in mice. J. Med. Virol. 26:153-162. [DOI] [PubMed] [Google Scholar]
- 20.Haeberle, H. A., W. A. Kuziel, H.-J. Dieterich, A. Casola, Z. Gatalica, and R. P. Garofalo. 2000. Inducible expression of inflammatory chemokines in respiratory syncytial virus-infected mice: role of MIP-1α in lung pathology. J. Virol. 75:878-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall, C. B., R. G. J. Douglas, R. L. Simons, and J. M. Geiman. 1978. Interferon production in children with respiratory syncytial, influenza, and parainfluenza virus infections. J. Pediatr. 93:28-32. [DOI] [PubMed] [Google Scholar]
- 22.Hemmi, H., O. Takeuchi, T. Kawai, T. Kaisho, S. Sato, H. Sanjo, M. Matsumoto, K. Hoshino, H. Wagner, K. Takeda, and S. Akira. 2000. A Toll-like receptor recognizes bacterial DNA. Nature 408:740-745. [DOI] [PubMed] [Google Scholar]
- 23.Higgins, P. G., G. I. Barrow, D. A. Tyrrell, D. Isaacs, and C. L. Gauci. 1990. The efficacy of intranasal interferon alpha-2a in respiratory syncytial virus infection in volunteers. Antiviral Res. 14:3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill, D. A., S. Baron, and R. M. Chanock. 1969. Sensitivity of common respiratory viruses to an interferon inducer in human cells. Lancet ii:187-188. [DOI] [PubMed] [Google Scholar]
- 25.Honda, K., H. Yanai, H. Negishi, M. Asagiri, M. Sato, T. Mizutani, N. Shimada, Y. Ohba, A. Takaoka, N. Yoshida, and T. Taniguchi. 2005. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature 434:772-777. [DOI] [PubMed] [Google Scholar]
- 26.Howe, M. 2002. Australian find suggests worldwide reach for metapneumovirus. Lancet Infect. Dis. 2:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jartti, T., B. G. van den Hoogen, R. P. Garofalo, A. D. Osterhaus, and O. Ruuskanen. 2002. Metapneumovirus and acute wheezing in children. Lancet 360:1393-1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawade, Y., J. Fujisawa, S. Yonehara, Y. Iwakura, and Y. Yamamoto. 1981. Purification of L cell interferon. Methods Enzymol. 78:522-535. [DOI] [PubMed] [Google Scholar]
- 29.Kawai, T., S. Sato, K. J. Ishii, C. Coban, H. Hemmi, M. Yamamoto, K. Terai, M. Matsuda, J. Inoue, S. Uematsu, O. Takeuchi, and S. Akira. 2004. Interferon-alpha induction through Toll-like receptors involves a direct interaction of IRF7 with MyD88 and TRAF6. Nat. Immunol. 5:1061-1068. [DOI] [PubMed] [Google Scholar]
- 30.Kisch, A. L., and K. M. Johnson. 1963. A plaque assay for respiratory syncytial virus. Proc. Soc. Exp. Biol. Med. 112:583. [DOI] [PubMed] [Google Scholar]
- 31.Krieg, A. M., A. K. Yi, S. Matson, T. J. Waldschmidt, G. A. Bishop, R. Teasdale, G. A. Koretzky, and D. M. Klinman. 1995. CpG motifs in bacterial DNA trigger direct B-cell activation. Nature 374:546-549. [DOI] [PubMed] [Google Scholar]
- 32.Laham, F. R., V. Israele, J. M. Casellas, A. M. Garcia, C. M. L. Prugent, S. J. Hoffman, D. Hauer, B. Thumar, M. I. Name, A. Pascual, N. Taratutto, M. T. Ishida, M. Balduzzi, M. Maccarone, S. Jackli, R. Passarino, R. A. Gaivironsky, R. A. Karron, N. R. Polack, and F. P. Polack. 2004. Differential production of inflammatory cytokines in primary infection with human metapneumovirus and with other common respiratory viruses of infancy. J. Infect. Dis. 189:2047-2056. [DOI] [PubMed] [Google Scholar]
- 33.Langford, M. P., D. A. Weigent, G. J. Stanton, and S. Baron. 1981. Virus plaque-reduction assay for interferon: microplaque and regular macroplaque reduction assays. Methods Enzymol. 78:339-346. [DOI] [PubMed] [Google Scholar]
- 34.Le Bon, A., G. Schiavoni, G. D'Agostino, I. Gresser, F. Belardelli, and D. F. Tough. 2001. Type i interferons potently enhance humoral immunity and can promote isotype switching by stimulating dendritic cells in vivo. Immunity 14:461-470. [DOI] [PubMed] [Google Scholar]
- 35.Le Bon, A., and D. F. Tough. 2002. Links between innate and adaptive immunity via type I interferon. Curr. Opin. Immunol. 14:432-436. [DOI] [PubMed] [Google Scholar]
- 36.Maggon, K., and S. Barik. 2004. New drugs and treatment for respiratory syncytial virus. Rev. Med. Virol. 14:149-168. [DOI] [PubMed] [Google Scholar]
- 37.Maniatis, T., J. V. Falvo, T. H. Kim, T. K. Kim, C. H. Lin, B. S. Parekh, and M. G. Wathelet. 1998. Structure and function of the interferon-beta enhanceosome. Cold Spring Harb. Symp. Quant. Biol. 63:609-620. [DOI] [PubMed] [Google Scholar]
- 38.Marrack, P., J. Kappler, and T. Mitchell. 1999. Type I interferons keep activated T cells alive. J. Exp. Med. 189:521-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McIntosh, K. 1978. Interferon in nasal secretions from infants with viral respiratory tract infections. J. Pediatr. 93:33-36. [DOI] [PubMed] [Google Scholar]
- 40.Merolla, R., N. A. Rebert, P. T. Tsiviste, S. P. Hoffmann, and R. Panuska. 1995. Respiratory syncytial virus replication in human lung epithelial cells: inhibition by tumor necrosis factor alpha and interferon beta. Am. J. Respir. Crit. Care Med. 152:1358-1366. [DOI] [PubMed] [Google Scholar]
- 41.Mogensen, T. H., and S. R. Paludan. 2005. Reading the viral signature by Toll-like receptors and other pattern recognition receptors. J. Mol. Med. 83:180-192. [DOI] [PubMed] [Google Scholar]
- 42.Olszewska-Pazdrak, B., A. Casola, T. Saito, R. Alam, S. E. Crowe, F. Mei, P. L. Ogra, and R. P. Garofalo. 1998. Cell-specific expression of RANTES, MCP-1, and MIP-1alpha by lower airway epithelial cells and eosinophils infected with respiratory syncytial virus. J. Virol. 72:4756-4764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peret, T. C., G. Boivin, Y. Li, M. Couillard, C. Humphrey, A. D. Osterhaus, D. D. Erdman, and L. J. Anderson. 2002. Characterization of human metapneumoviruses isolated from patients in North America. J. Infect. Dis. 185:1660-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sato, M., H. Suemori, N. Hata, M. Asagiri, K. Ogasawara, K. Nakao, T. Nakaya, M. Katsuki, S. Noguchi, N. Tanaka, and T. Taniguchi. 2000. Distinct and essential roles of transcription factors IRF-3 and IRF-7 in response to viruses for IFN-alpha/beta gene induction. Immunity 13:539-548. [DOI] [PubMed] [Google Scholar]
- 45.Schlender, J., B. Bossert, U. Buchholz, and K. K. Conzelmann. 2000. Bovine respiratory syncytial virus nonstructural proteins NS1 and NS2 cooperatively antagonize alpha/beta interferon-induced antiviral response. J. Virol. 74:8234-8242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schlender, J., V. Hornung, S. Finke, M. Gunthner-Biller, S. Marozin, K. Brzozka, S. Moghim, S. Endres, G. Hartmann, and K. K. Conzelmann. 2005. Inhibition of toll-like receptor 7- and 9-mediated alpha/beta interferon production in human plasmacytoid dendritic cells by respiratory syncytial virus and measles virus. J. Virol. 79:5507-5515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schoenemeyer, A., B. J. Barnes, M. E. Mancl, E. Latz, N. Goutagny, P. M. Pitha, K. A. Fitzgerald, and D. T. Golenbock. 2005. The interferon regulatory factor, IRF5, is a central mediator of Toll-like receptor 7 signaling. J. Biol. Chem. 280:17005-17012. [DOI] [PubMed] [Google Scholar]
- 48.Sharma, S., B. R. tenOever, N. Grandvaux, G. P. Zhou, R. Lin, and J. Hiscott. 2003. Triggering the interferon antiviral response through an IKK-related pathway. Science 300:1148-1151. [DOI] [PubMed] [Google Scholar]
- 49.Spann, K. M., K. C. Tran, B. Chi, R. L. Rabin, and P. L. Collins. 2004. Suppression of the induction of alpha, beta, and lambda interferons by the NS1 and NS2 proteins of human respiratory syncytial virus in human epithelial cells and macrophages [corrected]. J. Virol. 78:4363-4369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spann, K. M., K. C. Tran, and P. L. Collins. 2005. Effects of nonstructural proteins NS1 and NS2 of human respiratory syncytial virus on interferon regulatory factor 3, NF-κB, and proinflammatory cytokines. J. Virol. 79:5353-5362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sperber, S. J., and F. G. Hayden. 1989. Comparative susceptibility of respiratory viruses to recombinant interferons-alpha 2b and -beta. J. Interferon Res. 9:285-293. [DOI] [PubMed] [Google Scholar]
- 52.Stack, A. M., R. Malley, R. A. Saladino, J. B. Montana, K. L. MacDonald, and D. C. Molrine. 2000. Primary respiratory syncytial virus infection: pathology, immune response, and evaluation of vaccine challenge strains in a new mouse model. Vaccine 18:1412-1418. [DOI] [PubMed] [Google Scholar]
- 53.Sung, R. Y., J. Yin, S. J. Oppenheimer, J. S. Tam, and J. Lau. 1993. Treatment of respiratory syncytial virus infection with recombinant interferon alfa-2a. Arch. Dis. Child. 69:440-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taniguchi, T., K. Ogasawara, A. Takaoka, and N. Tanaka. 2001. IRF family of transcription factors as regulators of host defense. Annu. Rev. Immunol. 19:623-655. [DOI] [PubMed] [Google Scholar]
- 55.Ueba, O. 1978. Respiratory syncytial virus: I. concentration and purification of the infectious virus. Acta Med. Okayama 32:265-272. [PubMed] [Google Scholar]
- 56.Valarcher, J. F., J. Furze, S. Wyld, R. Cook, K. K. Conzelmann, and G. Taylor. 2003. Role of alpha/beta interferons in the attenuation and immunogenicity of recombinant bovine respiratory syncytial viruses lacking NS proteins. J. Virol. 77:8426-8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van den Hoogen, B. G., T. M. Bestebroer, A. D. Osterhaus, and R. A. Fouchier. 2002. Analysis of the genomic sequence of a human metapneumovirus. Virology 295:119-132. [DOI] [PubMed] [Google Scholar]
- 58.van den Hoogen, B. G., G. J. van Doornum, J. C. Fockens, J. J. Cornelissen, W. E. Beyer, R. de Groot, A. D. Osterhaus, and R. A. Fouchier. 2003. Prevalence and clinical symptoms of human metapneumovirus infection in hospitalized patients. J. Infect. Dis. 188:1571-1577. [DOI] [PubMed] [Google Scholar]
- 59.Williams, B. R. 3July2001. Signal integration via PKR. Sci. STKE 2001:RE2. [Online.] www.stke.org [DOI] [PubMed] [Google Scholar]
- 60.Yoneyama, M., M. Kikuchi, T. Natsukawa, N. Shinobu, T. Imaizumi, M. Miyagishi, K. Taira, S. Akira, and T. Fujita. 2004. The RNA helicase RIG-I has an essential function in double-stranded RNA-induced innate antiviral responses. Nat. Immunol. 5:730-737. [DOI] [PubMed] [Google Scholar]
- 61.Zhang, W., H. Yang, X. Kong, S. Mohapatra, H. S. Juan-Vergara, G. Hellermann, S. Behera, R. Singam, R. F. Lockey, and S. S. Mohapatra. 2005. Inhibition of respiratory syncytial virus infection with intranasal siRNA nanoparticles targeting the viral NS1 gene. Nat. Med. 11:56-62. [DOI] [PubMed] [Google Scholar]