Abstract
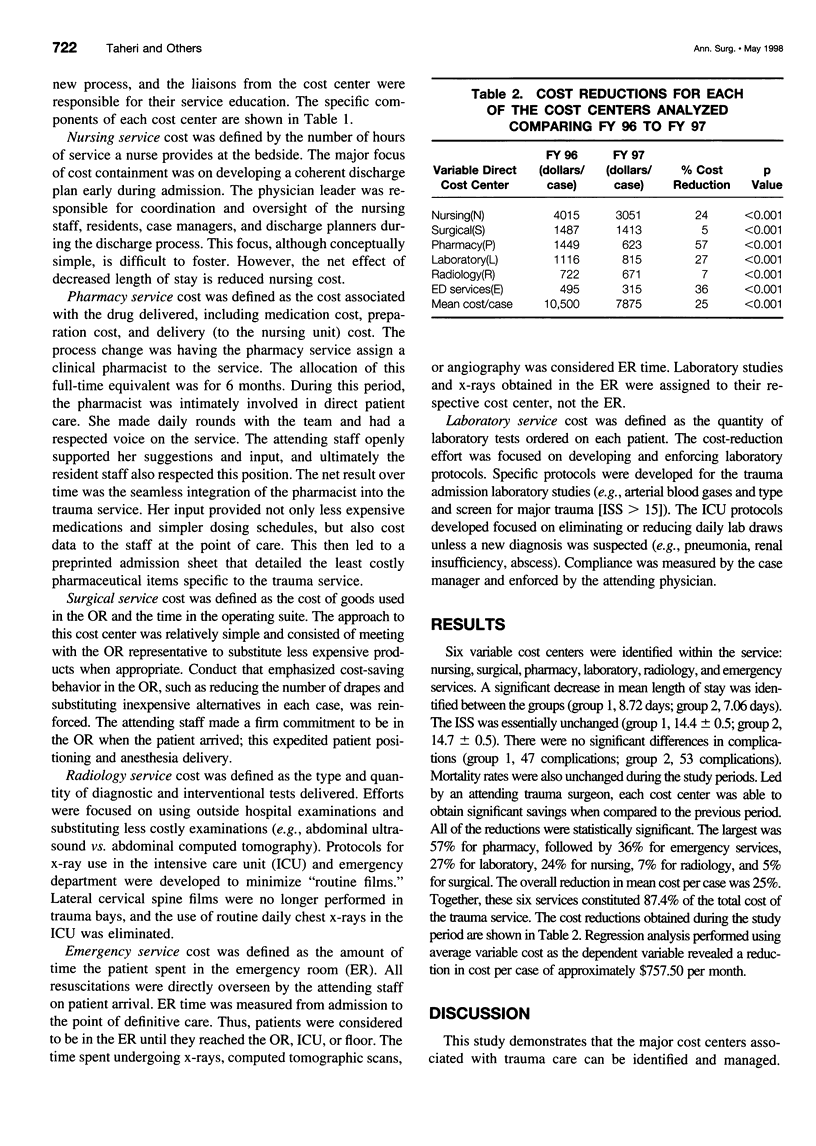
OBJECTIVE: The objective was to define and characterize the costs associated with trauma care at a level I trauma center. Once the costs were identified, attending physician-led teams were designed to reduce costs within each cost center. SUMMARY BACKGROUND DATA: The location and magnitude of the costs on a trauma service remain largely unknown. Focused cost-containment strategies remain difficult to implement because the expected return on these interventions is unknown. METHODS: Cost center data were reviewed for the 40 major DRGs admitted for the first 6 months of the fiscal years 1996 and 1997. Data were obtained from the hospital finance department using the Transition Systems Inc. accounting system. We focused on variable direct costs, those that vary with patient volume (e.g., staff nursing expense and medical/surgical supplies). To address issues of inflation, pay raises, and changing costs, a proxy value was created for 1996 and costs were held constant for the 1997 calculation. The major services that constitute cost centers identified in the system were nursing, surgical, pharmacy, laboratory, radiology, and emergency services. Attendings were assigned to develop and oversee customized cost-reduction modalities specific to each cost center. The cost-reduction modalities used to achieve significant savings were as follows: nursing, case management approach focusing on early discharge; surgical, meeting with operating room (OR) purchasing to modify expensive behavior patterns; pharmacy, integrating clinical pharmacist with direct attending support; laboratory, enforcing protocol for lab draws; radiology, increasing the use of emergency room ultrasound and accepting outside x-rays; and emergency services, 24-hour in-house attending staff to reduce emergency room time. The surgical and emergency services cost centers predominately generate costs by the length of time care is delivered in that area. RESULTS: For each period, data from 363 patients were compared. Mean length of stay decreased between the study periods from 8.72 to 7.06 days, while the average injury severity score was unchanged. Together, these cost centers constituted 87.4% of the total cost of care delivered. Significant cost reduction was achieved in all six variable cost centers: nursing (24%), surgical (5%), pharmacy (57%), laboratory (27), radiology (7%), and emergency (36). The mean cost per case was reduced by 25%. CONCLUSIONS: Identification of the true cost centers and directed attending surgeon involvement are essential to the development and implementation of a successful cost-reduction process.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blackstone M. E., Miller R. S., Hodgson A. J., Cooper S. S., Blackhurst D. W., Stein M. A. Lowering hospital charges in the trauma intensive care unit while maintaining quality of care by increasing resident and attending physician awareness. J Trauma. 1995 Dec;39(6):1041–1044. doi: 10.1097/00005373-199512000-00004. [DOI] [PubMed] [Google Scholar]
- Campbell A. R., Vittinghoff E., Morabito D., Paine M., Shagoury C., Praetz P., Grey D., McAninch J. W., Schecter W. P. Trauma centers in a managed care environment. J Trauma. 1995 Aug;39(2):246–253. doi: 10.1097/00005373-199508000-00010. [DOI] [PubMed] [Google Scholar]
- Civetta J. M., Hudson-Civetta J. A. Maintaining quality of care while reducing charges in the ICU. Ten ways. Ann Surg. 1985 Oct;202(4):524–532. doi: 10.1097/00000658-198510000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen I. L., Booth F. V. Cost containment and mechanical ventilation in the United States. New Horiz. 1994 Aug;2(3):283–290. [PubMed] [Google Scholar]
- Eastman A. B., Bishop G. S., Walsh J. C., Richardson J. D., Rice C. L. The economic status of trauma centers on the eve of health care reform. J Trauma. 1994 Jun;36(6):835–846. [PubMed] [Google Scholar]
- Eastman A. B., Rice C. L., Bishop G., Richardson J. D. An analysis of the critical problem of trauma center reimbursement. J Trauma. 1991 Jul;31(7):920–926. doi: 10.1097/00005373-199107000-00007. [DOI] [PubMed] [Google Scholar]
- Elliott D. C., Rodriguez A. Cost effectiveness in trauma care. Surg Clin North Am. 1996 Feb;76(1):47–62. doi: 10.1016/s0039-6109(05)70421-7. [DOI] [PubMed] [Google Scholar]
- Helling T. S., Watkins M., Robb C. V. Improvement in cost recovery at an urban level I trauma center. J Trauma. 1995 Nov;39(5):980–983. doi: 10.1097/00005373-199511000-00027. [DOI] [PubMed] [Google Scholar]
- Joy S. A., Lichtig L. K., Knauf R. A., Martin K., Yurt R. W. Identification and categorization of and cost for care of trauma patients: a study of 12 trauma centers and 43,219 statewide patients. J Trauma. 1994 Aug;37(2):303–313. doi: 10.1097/00005373-199408000-00024. [DOI] [PubMed] [Google Scholar]
- Kizer K. W., Vassar M. J., Harry R. L., Layton K. D. Hospitalization charges, costs, and income for firearm-related injuries at a university trauma center. JAMA. 1995 Jun 14;273(22):1768–1773. [PubMed] [Google Scholar]
- Miller T. R., Levy D. T. The effect of regional trauma care systems on costs. Arch Surg. 1995 Feb;130(2):188–193. doi: 10.1001/archsurg.1995.01430020078014. [DOI] [PubMed] [Google Scholar]
- O'Keefe G. E., Maier R. V., Diehr P., Grossman D., Jurkovich G. J., Conrad D. The complications of trauma and their associated costs in a level I trauma center. Arch Surg. 1997 Aug;132(8):920–925. doi: 10.1001/archsurg.1997.01430320122021. [DOI] [PubMed] [Google Scholar]
- Roberts D. E., Bell D. D., Ostryzniuk T., Dobson K., Oppenheimer L., Martens D., Honcharik N., Cramp H., Loewen E., Bodnar S. Eliminating needless testing in intensive care--an information-based team management approach. Crit Care Med. 1993 Oct;21(10):1452–1458. doi: 10.1097/00003246-199310000-00011. [DOI] [PubMed] [Google Scholar]
- Rogers F. B., Osler T. M., Shackford S. R., Cohen M., Camp L. Financial outcome of treating trauma in a rural environment. J Trauma. 1997 Jul;43(1):65–73. doi: 10.1097/00005373-199707000-00016. [DOI] [PubMed] [Google Scholar]
- Shapiro M. J., Keegan M., Copeland J. The misconception of trauma reimbursement. Arch Surg. 1989 Oct;124(10):1237–1240. doi: 10.1001/archsurg.1989.01410100143025. [DOI] [PubMed] [Google Scholar]
- Siegel J. H., Shafi S., Goodarzi S., Dischinger P. C. A quantitative method for cost reimbursement and length of stay quality assurance in multiple trauma patients. J Trauma. 1994 Dec;37(6):928–937. doi: 10.1097/00005373-199412000-00010. [DOI] [PubMed] [Google Scholar]
- Silverstein D. S., Livingston D. H., Elcavage J., Kovar L., Kelly K. M. The utility of routine daily chest radiography in the surgical intensive care unit. J Trauma. 1993 Oct;35(4):643–646. doi: 10.1097/00005373-199310000-00022. [DOI] [PubMed] [Google Scholar]
- Waller J. A., Payne S. R., McClallen J. M. Trauma centers and DRGs--inherent conflict? J Trauma. 1989 May;29(5):617–622. doi: 10.1097/00005373-198905000-00016. [DOI] [PubMed] [Google Scholar]


