Abstract
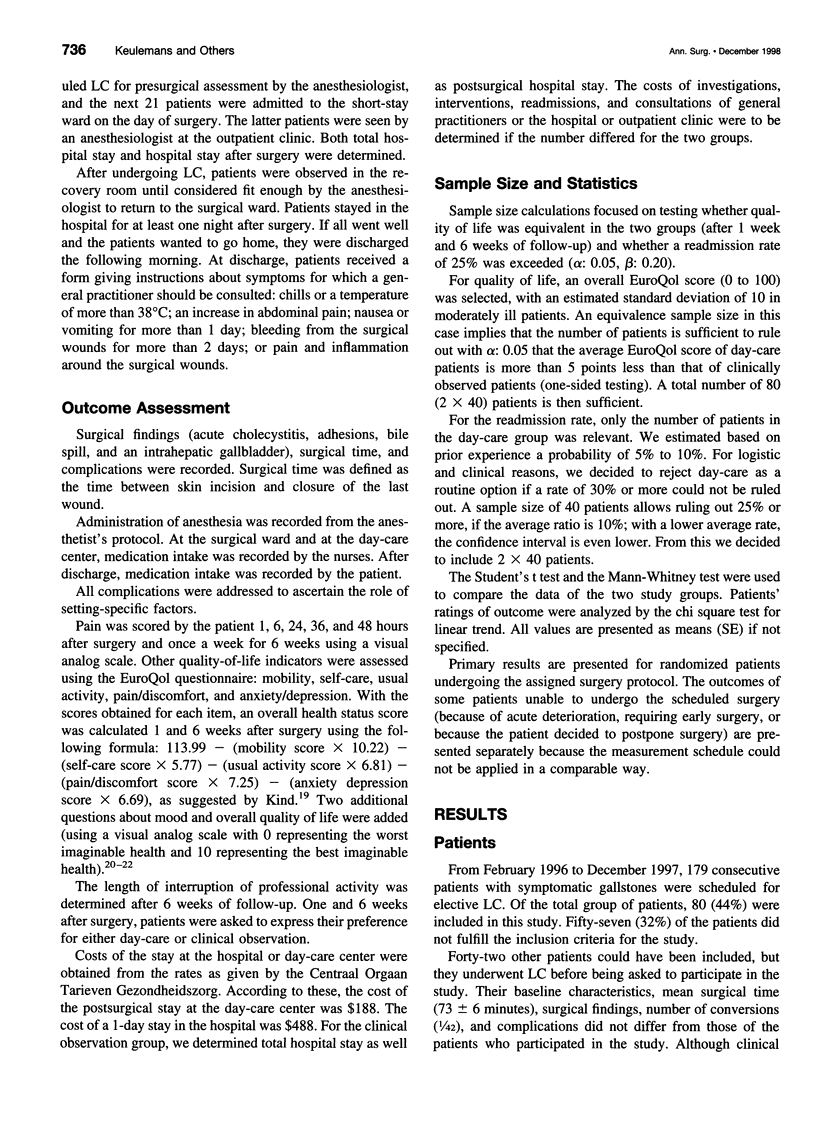
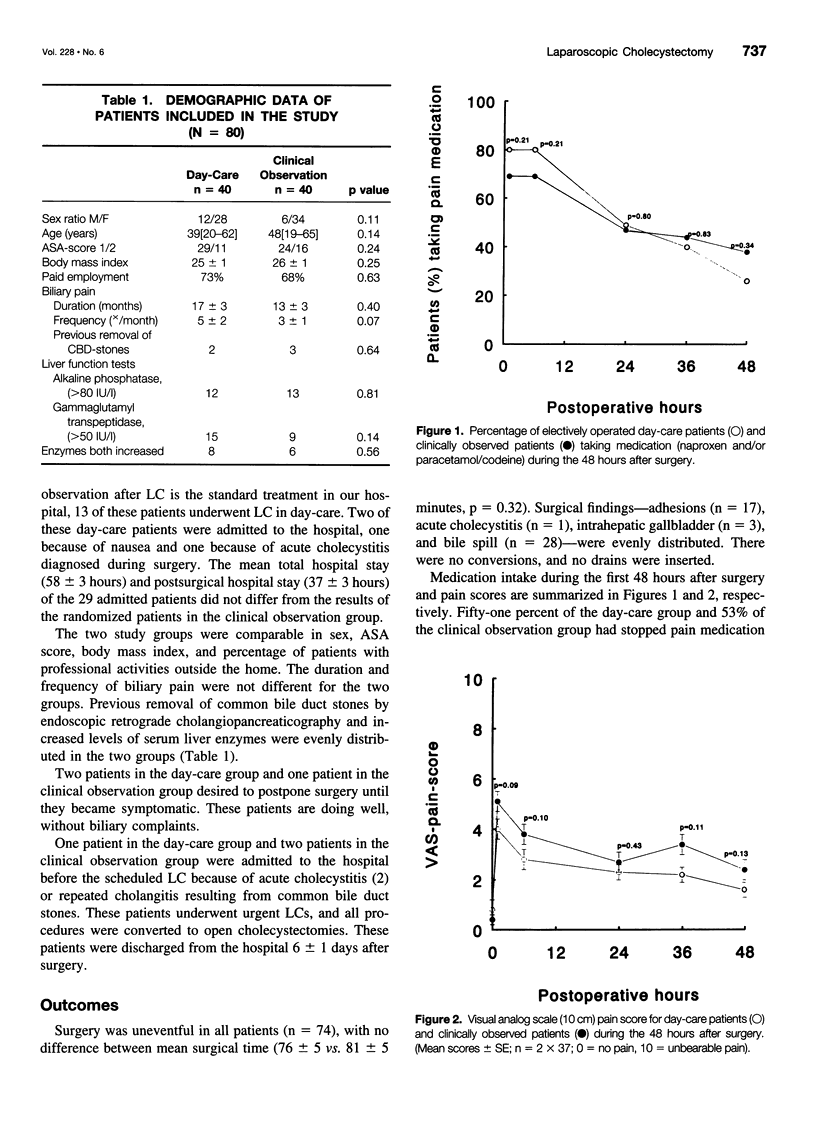
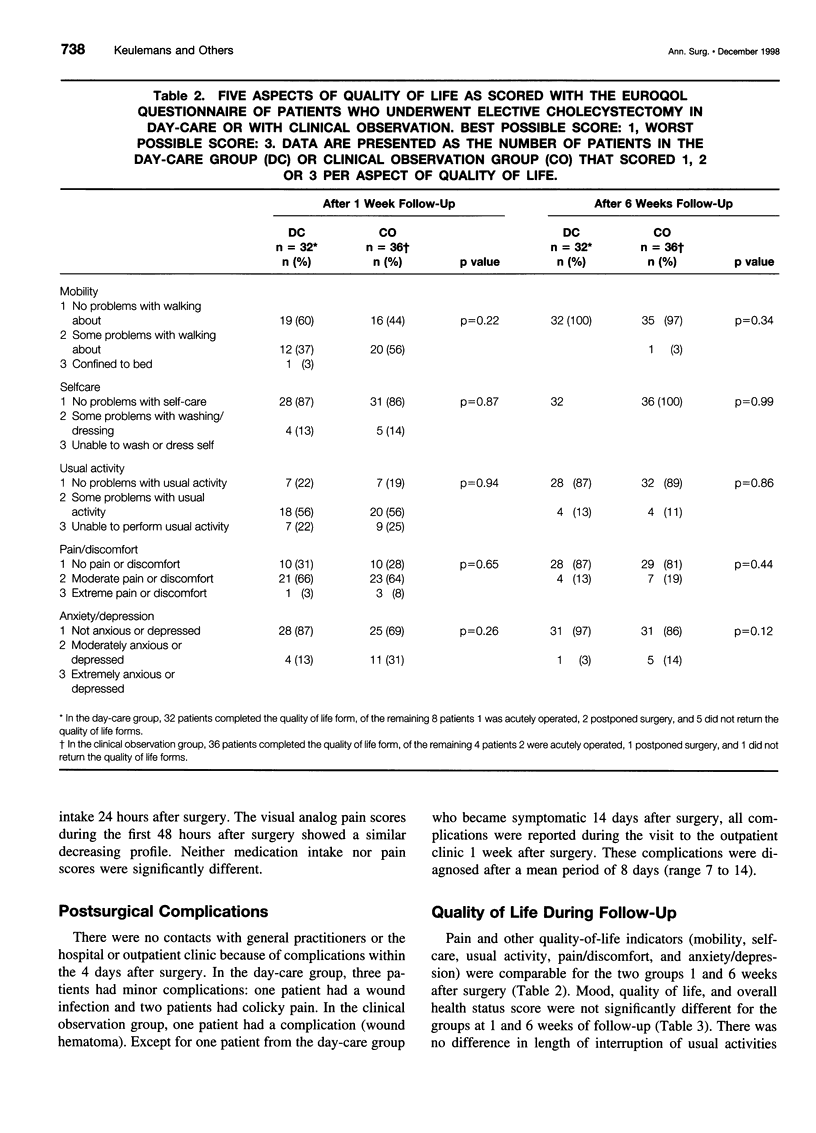
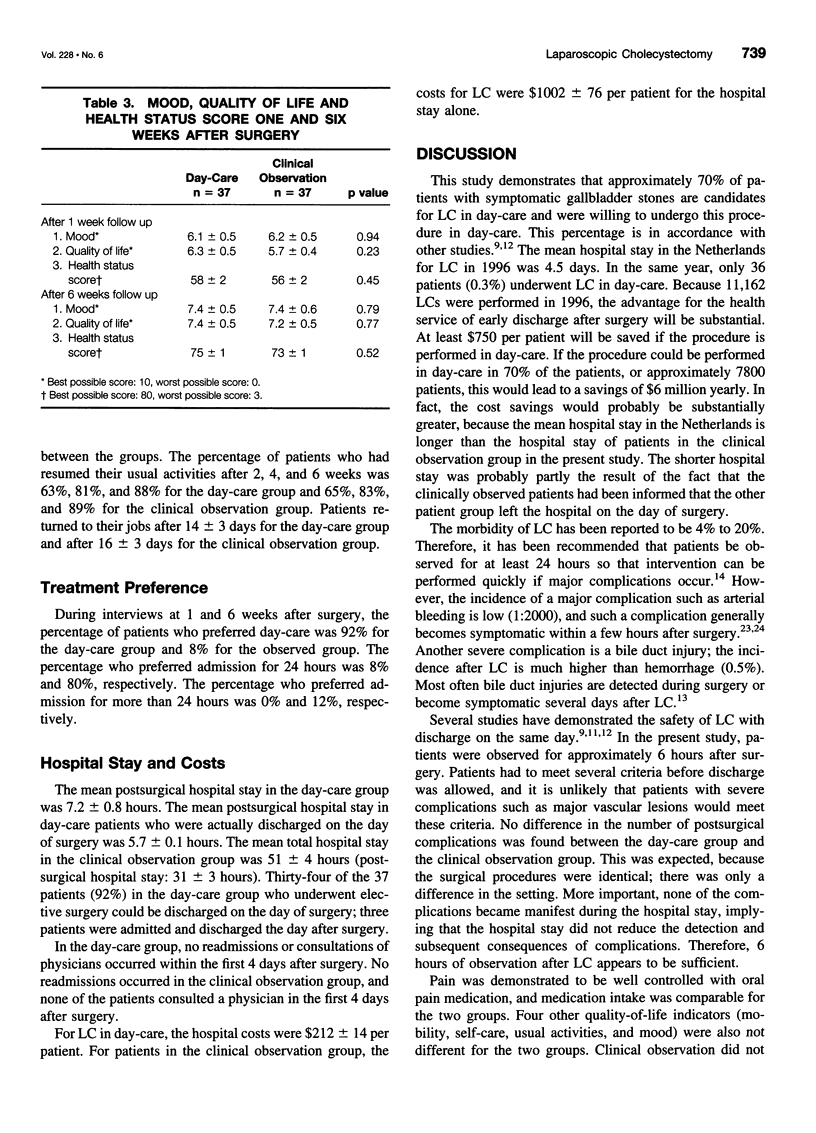
OBJECTIVE: To determine the feasibility and desirability of laparoscopic cholecystectomy (LC) in day-care versus LC with clinical observation. SUMMARY BACKGROUND DATA: Laparoscopic cholecystectomy has been performed regularly as outpatient surgery in patients with uncomplicated gallstone disease in the United States, but this has not been generally accepted in Europe. The main objections are the risk of early severe complications (bleeding) or other reasons for readmission, and the argument that patients might feel safer when observed for one night. Quality-of-life differences hitherto have not been investigated. METHODS: Eighty patients (American Society of Anesthesiology [ASA] I/II) with symptomatic gallstones were randomized to receive LC either in day-care or with clinical observation. Complications, (re)admissions, consultations of general practitioners or the day-care center within 4 days after surgery, use of pain medication, quality of life, convalescence period, time off from professional activities, and treatment preference were assessed. The respective costs of day-care and clinical observation were determined. RESULTS: Of the 37 patients assigned to the day-care group who underwent elective surgery, 92% were discharged successfully after an observation period of 5.7+/-0.2 hours. The remainder of the patients in this group were admitted to the hospital and clinically observed for 24 hours. For the 37 patients in the clinical observation group who underwent elective surgery, the observation time after surgery was 31+/-3 hours. Three patients in the day-care group and one patient in the clinical observation group had complications after surgery. None of the patients in either group consulted a general practitioner or the hospital during the first week after surgery. Use of pain medication was comparable in both groups over the first 48 hours after surgery. There were no differences in pain and other quality-of-life indicators between the groups during the 6 weeks of follow-up. Of the patients in the day-care group, 92% preferred day-care to clinical observation. The same percentage of patients in the clinical observation group preferred at least 24 hours of observation to day-care. Costs for the day-care patients were substantially lower (approximately $750/patient) than for the clinical observation patients. CONCLUSION: Effectiveness was equal in both patient groups, and both groups appeared to be satisfied with their treatment. Because no differences were found with respect to the other outcomes, day-care is the preferred treatment in most ASA I and II patients because it is less expensive.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berggren U., Gordh T., Grama D., Haglund U., Rastad J., Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994 Sep;81(9):1362–1365. doi: 10.1002/bjs.1800810936. [DOI] [PubMed] [Google Scholar]
- Cameron J. L., Gadacz T. R. Laparoscopic cholecystectomy. Ann Surg. 1991 Jan;213(1):1–2. doi: 10.1097/00000658-199101000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collet D. Laparoscopic cholecystectomy in 1994. Results of a prospective survey conducted by SFCERO on 4,624 cases. Société Française de Chirurgie Endoscopique et Radiologie Opératoire. Surg Endosc. 1997 Jan;11(1):56–63. doi: 10.1007/s004649900295. [DOI] [PubMed] [Google Scholar]
- DRIPPS R. D., LAMONT A., ECKENHOFF J. E. The role of anesthesia in surgical mortality. JAMA. 1961 Oct 21;178:261–266. doi: 10.1001/jama.1961.03040420001001. [DOI] [PubMed] [Google Scholar]
- Deziel D. J., Millikan K. W., Economou S. G., Doolas A., Ko S. T., Airan M. C. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993 Jan;165(1):9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- Essink-Bot M. L., Krabbe P. F., Bonsel G. J., Aaronson N. K. An empirical comparison of four generic health status measures. The Nottingham Health Profile, the Medical Outcomes Study 36-item Short-Form Health Survey, the COOP/WONCA charts, and the EuroQol instrument. Med Care. 1997 May;35(5):522–537. doi: 10.1097/00005650-199705000-00008. [DOI] [PubMed] [Google Scholar]
- Go P. M., Schol F., Gouma D. J. Laparoscopic cholecystectomy in The Netherlands. Br J Surg. 1993 Sep;80(9):1180–1183. doi: 10.1002/bjs.1800800938. [DOI] [PubMed] [Google Scholar]
- Grace P. A., Quereshi A., Coleman J., Keane R., McEntee G., Broe P., Osborne H., Bouchier-Hayes D. Reduced postoperative hospitalization after laparoscopic cholecystectomy. Br J Surg. 1991 Feb;78(2):160–162. doi: 10.1002/bjs.1800780209. [DOI] [PubMed] [Google Scholar]
- Keulemans Y. C., Bergman J. J., de Wit L. T., Rauws E. A., Huibregtse K., Tytgat G. N., Gouma D. J. Improvement in the management of bile duct injuries? J Am Coll Surg. 1998 Sep;187(3):246–254. doi: 10.1016/s1072-7515(98)00155-0. [DOI] [PubMed] [Google Scholar]
- Keulemans Y. C., Eshuis J. H., Leeuwenberg A., de Wit L. T., Gouma D. J. Ervaringen met poliklinische laparoscopische cholecystectomie. Ned Tijdschr Geneeskd. 1997 Apr 5;141(14):686–689. [PubMed] [Google Scholar]
- McDonald P. T., Rich N. M., Collins G. J., Jr, Andersen C. A., Kozloff L. Vascular trauma secondary to diagnostic and therapeutic procedures: laparoscopy. Am J Surg. 1978 May;135(5):651–655. doi: 10.1016/0002-9610(78)90129-0. [DOI] [PubMed] [Google Scholar]
- McMahon A. J., Russell I. T., Baxter J. N., Ross S., Anderson J. R., Morran C. G., Sunderland G., Galloway D., Ramsay G., O'Dwyer P. J. Laparoscopic versus minilaparotomy cholecystectomy: a randomised trial. Lancet. 1994 Jan 15;343(8890):135–138. doi: 10.1016/s0140-6736(94)90932-6. [DOI] [PubMed] [Google Scholar]
- Michaloliakou C., Chung F., Sharma S. Preoperative multimodal analgesia facilitates recovery after ambulatory laparoscopic cholecystectomy. Anesth Analg. 1996 Jan;82(1):44–51. doi: 10.1097/00000539-199601000-00009. [DOI] [PubMed] [Google Scholar]
- Peters J. H., Ellison E. C., Innes J. T., Liss J. L., Nichols K. E., Lomano J. M., Roby S. R., Front M. E., Carey L. C. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991 Jan;213(1):3–12. doi: 10.1097/00000658-199101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad A., Foley R. J. Day case laparoscopic cholecystectomy: a safe and cost effective procedure. Eur J Surg. 1996 Jan;162(1):43–46. [PubMed] [Google Scholar]
- Reddick E. J., Olsen D. O. Outpatient laparoscopic laser cholecystectomy. Am J Surg. 1990 Nov;160(5):485–489. doi: 10.1016/s0002-9610(05)81009-8. [DOI] [PubMed] [Google Scholar]
- Saltzstein E. C., Mercer L. C., Peacock J. B., Dougherty S. H. Twenty-four hour hospitalization after cholecystectomy. Surg Gynecol Obstet. 1991 Nov;173(5):367–370. [PubMed] [Google Scholar]
- Sawyers J. L. Current status of conventional (open) cholecystectomy versus laparoscopic cholecystectomy. Ann Surg. 1996 Jan;223(1):1–3. doi: 10.1097/00000658-199601000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Haes J. C., van Knippenberg F. C., Neijt J. P. Measuring psychological and physical distress in cancer patients: structure and application of the Rotterdam Symptom Checklist. Br J Cancer. 1990 Dec;62(6):1034–1038. doi: 10.1038/bjc.1990.434. [DOI] [PMC free article] [PubMed] [Google Scholar]


