Abstract
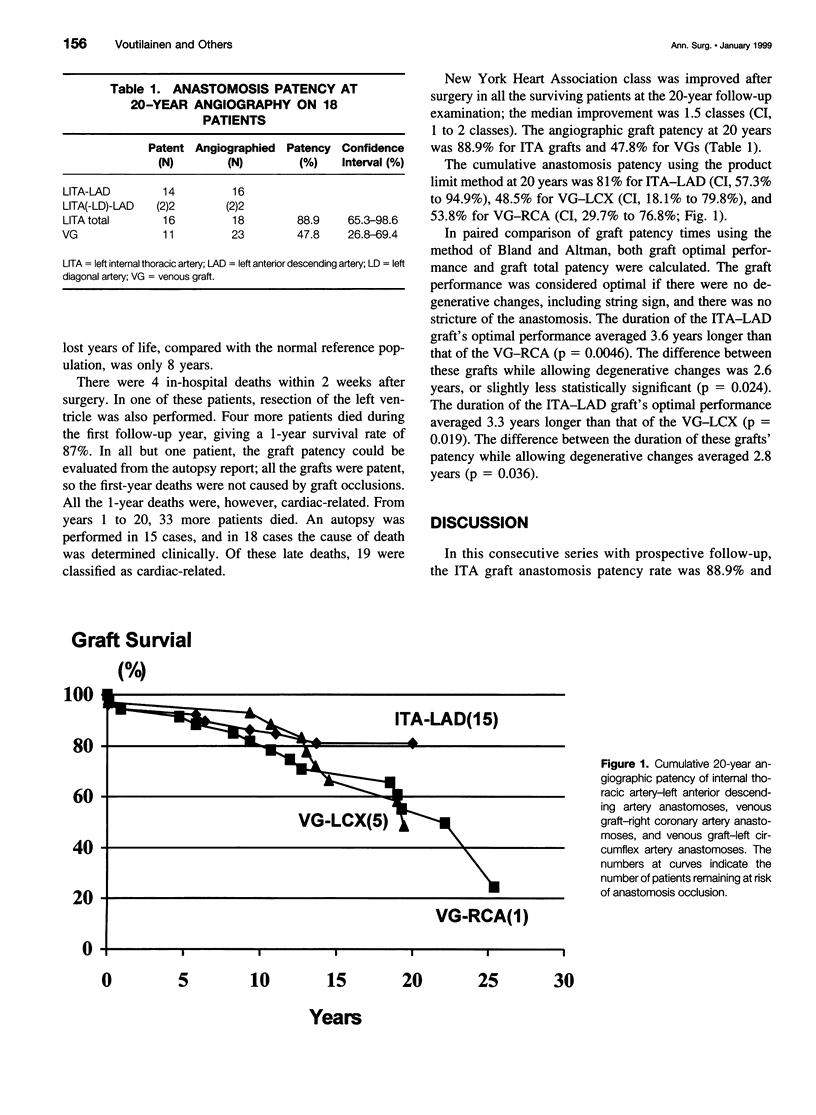
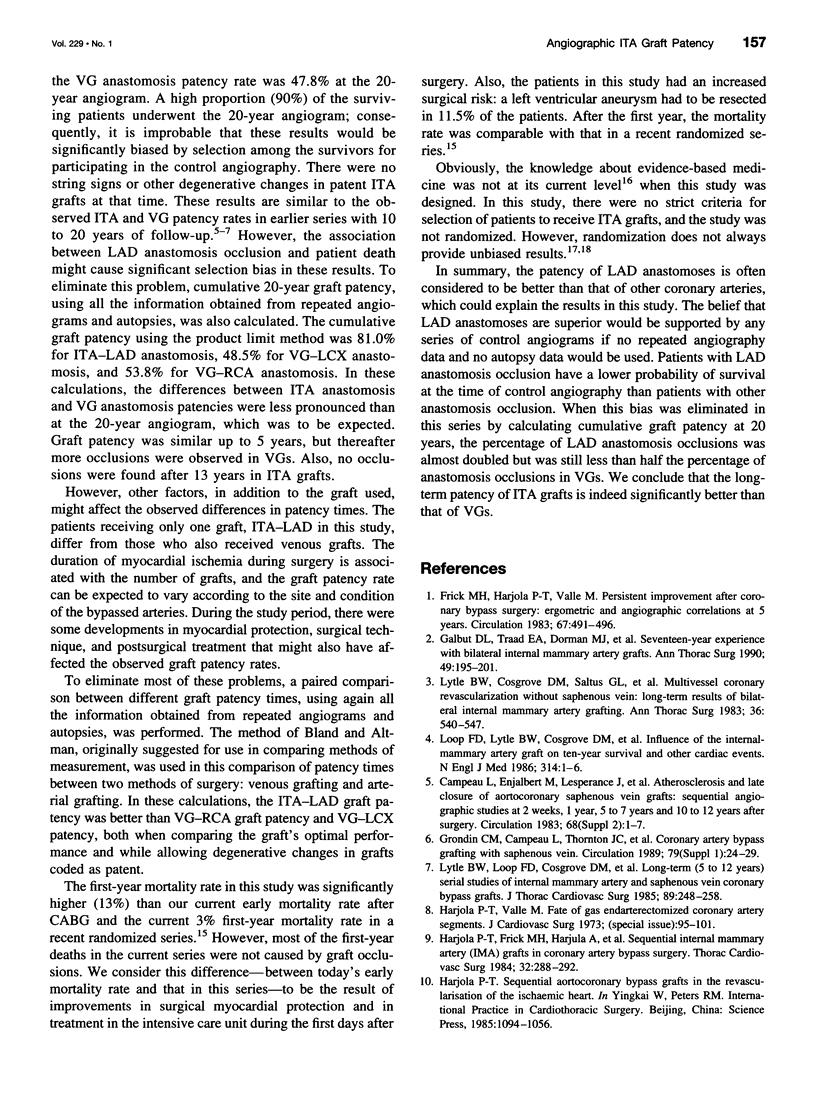
OBJECTIVE: To assess the behavior of internal thoracic artery (ITA) grafts versus venous grafts in repeated angiograms up to 20 years. SUMMARY BACKGROUND DATA: Use of ITA grafts to bypass left anterior descending artery stenosis has been shown to be associated with improved survival in patients undergoing coronary artery bypass grafting. METHODS: Sixty-one consecutive patients who received one or two ITA grafts and who underwent surgery from Oct. 5, 1971, to Dec. 18, 1973, in Helsinki University Central Hospital, Finland, were included in this prospective follow-up series. Fifty-six of the patients (92%) also received at least one venous graft. The number of distal anastomoses was 157, of which 47.7% (75) were performed with ITA grafts. The median age of the patients was 47.7 years (range 30.0 to 63.1), and 85% (52) were men. RESULTS: After 20 years of follow-up, 18/20 (90%) of the survivors underwent angiography; the patency rate was 88.9% for ITA grafts and 47.8% for venous grafts. Cumulative graft patency at 20 years, using all the information obtained from repeated angiographic examinations and autopsies, was also calculated to eliminate selection bias. The cumulative 20-year patency rate was 81% for ITA-left anterior descending artery anastomoses, 53.8% for venous graft-right coronary artery anastomoses, and 48.5% for venous graft-left circumflex artery anastomoses. In paired comparisons between anastomoses, the patency time of the ITA-left anterior descending artery anastomoses was on average 2.8 years longer than the venous graft-left circumflex artery patency time and 2.6 years longer than the venous graft-right coronary artery. CONCLUSIONS: Internal thoracic artery grafts, especially in left anterior descending artery anastomoses, should be considered as a primary solution in coronary artery bypass grafting surgery in patients with >10 years of life expectancy; if venous grafting is preferred, further evidence is needed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Begg C., Cho M., Eastwood S., Horton R., Moher D., Olkin I., Pitkin R., Rennie D., Schulz K. F., Simel D. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA. 1996 Aug 28;276(8):637–639. doi: 10.1001/jama.276.8.637. [DOI] [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995 Oct 21;346(8982):1085–1087. doi: 10.1016/s0140-6736(95)91748-9. [DOI] [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Frick M. H., Harjola P. T., Valle M. Persistent improvement after coronary bypass surgery: ergometric and angiographic correlations at 5 years. Circulation. 1983 Mar;67(3):491–496. doi: 10.1161/01.cir.67.3.491. [DOI] [PubMed] [Google Scholar]
- Galbut D. L., Traad E. A., Dorman M. J., DeWitt P. L., Larsen P. B., Kurlansky P. A., Button J. H., Ally J. M., Gentsch T. O. Seventeen-year experience with bilateral internal mammary artery grafts. Ann Thorac Surg. 1990 Feb;49(2):195–201. doi: 10.1016/0003-4975(90)90138-v. [DOI] [PubMed] [Google Scholar]
- Hakulinen T., Abeywickrama K. H. A computer program package for relative survival analysis. Comput Programs Biomed. 1985;19(2-3):197–207. doi: 10.1016/0010-468x(85)90011-x. [DOI] [PubMed] [Google Scholar]
- Harjola P. T., Frick M. H., Harjula A., Järvinen A., Meurala H., Valle M. Sequential internal mammary artery (IMA) grafts in coronary artery bypass surgery. Thorac Cardiovasc Surg. 1984 Oct;32(5):288–292. doi: 10.1055/s-2007-1023406. [DOI] [PubMed] [Google Scholar]
- Harjola P. T., Valle M. Fate of gas endarterectomized coronary artery segments. J Cardiovasc Surg (Torino) 1973;Spec No:95–101. [PubMed] [Google Scholar]
- Loop F. D., Lytle B. W., Cosgrove D. M., Stewart R. W., Goormastic M., Williams G. W., Golding L. A., Gill C. C., Taylor P. C., Sheldon W. C. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986 Jan 2;314(1):1–6. doi: 10.1056/NEJM198601023140101. [DOI] [PubMed] [Google Scholar]
- Lytle B. W., Cosgrove D. M., Saltus G. L., Taylor P. C., Loop F. D. Multivessel coronary revascularization without saphenous vein: long-term results of bilateral internal mammary artery grafting. Ann Thorac Surg. 1983 Nov;36(5):540–547. doi: 10.1016/s0003-4975(10)60684-4. [DOI] [PubMed] [Google Scholar]
- Lytle B. W., Loop F. D., Cosgrove D. M., Ratliff N. B., Easley K., Taylor P. C. Long-term (5 to 12 years) serial studies of internal mammary artery and saphenous vein coronary bypass grafts. J Thorac Cardiovasc Surg. 1985 Feb;89(2):248–258. [PubMed] [Google Scholar]
- Schulz K. F., Chalmers I., Hayes R. J., Altman D. G. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995 Feb 1;273(5):408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]


