Abstract
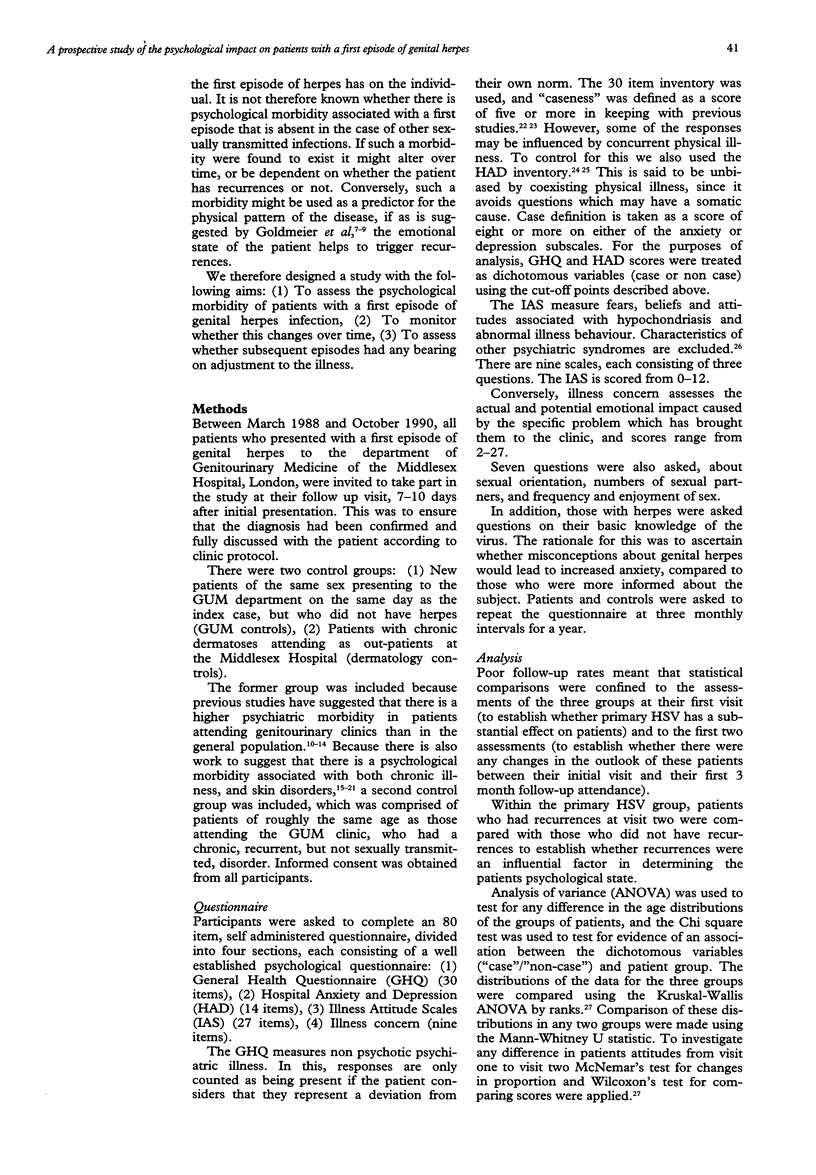
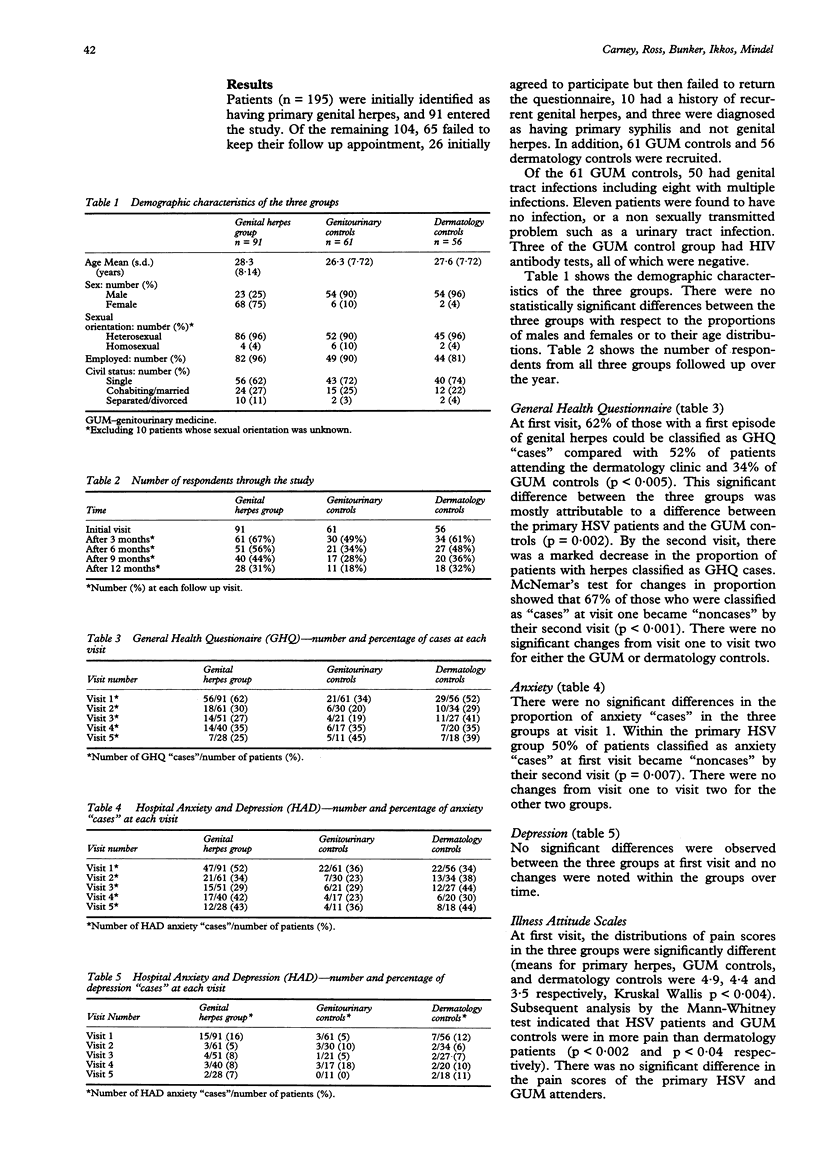
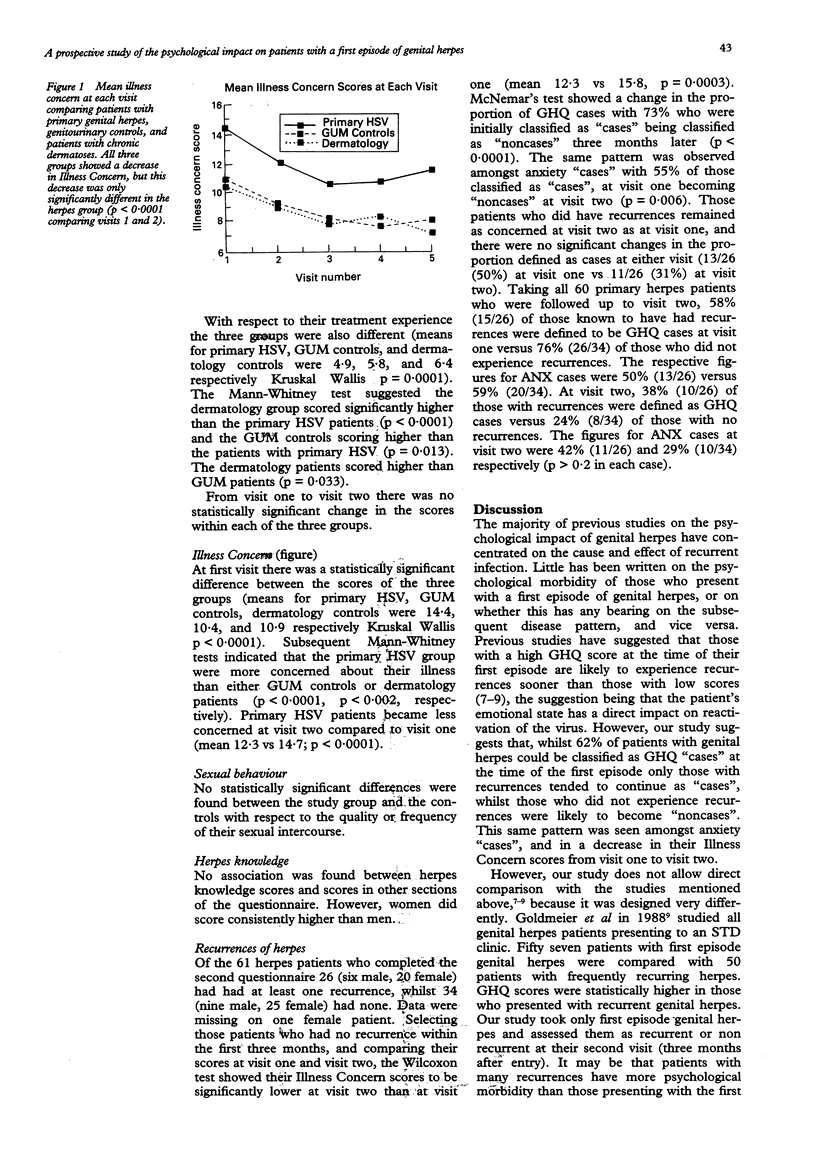
OBJECTIVES--To assess the psychological impact of first episode of genital herpes, and to determine whether this changes over time. SETTING AND SUBJECTS--The Departments of Genitourinary Medicine (GUM), and Dermatology, Middlesex Hospital London. The study group consisted of patients attending the department of GUM with a clinically proven first episode of genital herpes. Two control groups were recruited; firstly patients without herpes attending the GUM Department and secondly patients attending the Dermatology Department out patients with chronic dermatoses. METHODS--Patients and controls completed an 87 item, self-administered psychological questionnaire at 3 monthly intervals for a year. The questionnaire consisted of the General Health Questionnaire (GHQ); the Hospital Anxiety and Depression Questionnaire (HADQ); Illness Attitude Scales and Illness Concern. Patients were also asked questions about their sexual behaviour. RESULTS--Ninety one patients (68 women, 23 men) with genital herpes, 61 GUM controls (42 women, 19 men) and 56 dermatology controls (36 women, 20 men) participated. There were no statistically significant demographic differences between patients and controls. At first visit the proportion of patients classified as "cases" by the GHQ (GHQ cases) were similar for primary herpes patients 62% (56/91) and Dermatology controls 52% (29/56) while a significantly smaller proportion of GUM controls 34% (21/61) were classified as GHQ cases. The primary herpes group were significantly more concerned about their illness than either the GUM controls or the Dermatology controls (p < 0.002). The proportion of primary herpes patients classified as "cases" by the GHQ reduced significantly over the initial three month period with 67% of patients classified as "cases" at their first visit becoming "noncases" after three months (p < 0.0001). Also 50% of those classified as "cases" at first visit by the HADQ become "noncases" after the initial three months (p = 0.007). The illness concern scores also decreased significantly from visit one to visit two (means 14.7 vs. 12.3; p < 0.0001). CONCLUSION--The diagnosis of a first episode of genital herpes has a profound emotional effect on patients. If they do not have recurrent episodes, their emotional state improves. For those who do have recurrences, the level of anxiety and concern remains as high as at the time of their first diagnosis. Clinicians must be sensitive to the emotional impact such a diagnosis may bring.
Full text
PDF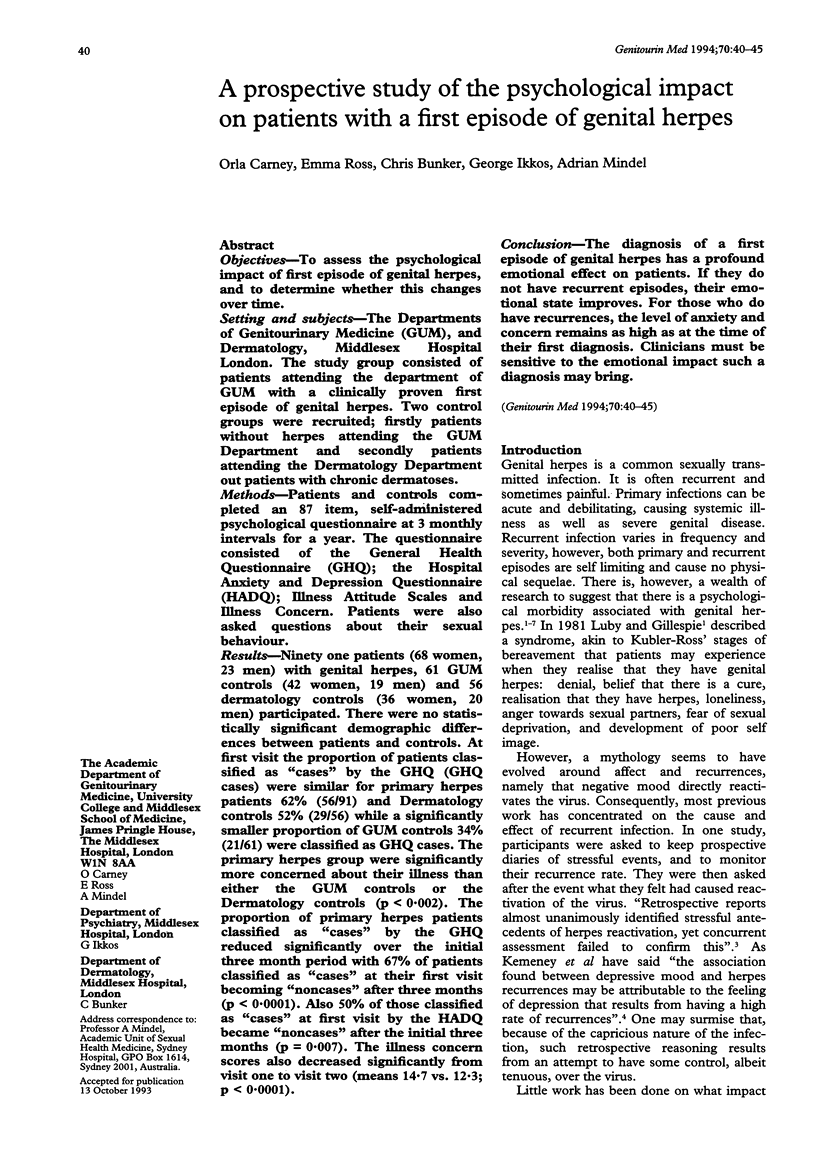

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barczak P., Kane N., Andrews S., Congdon A. M., Clay J. C., Betts T. Patterns of psychiatric morbidity in a genito-urinary clinic. A validation of the Hospital Anxiety Depression scale (HAD). Br J Psychiatry. 1988 May;152:698–700. doi: 10.1192/bjp.152.5.698. [DOI] [PubMed] [Google Scholar]
- Beaman K., Luzzatto P. Psychological approaches to the treatment of skin diseases. Nursing (Lond) 1988 Aug-Sep;3(29):1061–1063. [PubMed] [Google Scholar]
- Benjamin S., Decalmer P., Haran D. Community screening for mental illness: a validity study of the General Health Questionnaire. Br J Psychiatry. 1982 Feb;140:174–180. doi: 10.1192/bjp.140.2.174. [DOI] [PubMed] [Google Scholar]
- Bombardier C. H., D'Amico C., Jordan J. S. The relationship of appraisal and coping to chronic illness adjustment. Behav Res Ther. 1990;28(4):297–304. doi: 10.1016/0005-7967(90)90081-s. [DOI] [PubMed] [Google Scholar]
- Catalan J., Bradley M., Gallwey J., Hawton K. Sexual dysfunction and psychiatric morbidity in patients attending a clinic for sexually transmitted diseases. Br J Psychiatry. 1981 Apr;138:292–296. doi: 10.1192/bjp.138.4.292. [DOI] [PubMed] [Google Scholar]
- Cotterill J. A. Psychiatry and the skin. Br J Hosp Med. 1989 Nov;42(5):401–404. [PubMed] [Google Scholar]
- Fulford K. W., Catterall R. D., Hoinville E., Lim K. S., Wilson G. D. Social and psychological factors in the distribution of STD in male clinic attenders. II Personality disorders, psychiatric illness, and abnormal sexual attitudes. Br J Vener Dis. 1983 Dec;59(6):381–385. doi: 10.1136/sti.59.6.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmeier D., Johnson A., Byrne M., Barton S. Psychosocial implications of recurrent genital herpes simplex virus infection. Genitourin Med. 1988 Oct;64(5):327–330. doi: 10.1136/sti.64.5.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmeier D., Johnson A., Jeffries D., Walker G. D., Underhill G., Robinson G., Ribbans H. Psychological aspects of recurrences of genital herpes. J Psychosom Res. 1986;30(5):601–608. doi: 10.1016/0022-3999(86)90033-4. [DOI] [PubMed] [Google Scholar]
- Hardy G. E., Cotterill J. A. A study of depression and obsessionality in dysmorphophobic and psoriatic patients. Br J Psychiatry. 1982 Jan;140:19–22. doi: 10.1192/bjp.140.1.19. [DOI] [PubMed] [Google Scholar]
- Hughes J. E., Barraclough B. M., Hamblin L. G., White J. E. Psychiatric symptoms in dermatology patients. Br J Psychiatry. 1983 Jul;143:51–54. doi: 10.1192/bjp.143.1.51. [DOI] [PubMed] [Google Scholar]
- Kemeny M. E., Cohen F., Zegans L. S., Conant M. A. Psychological and immunological predictors of genital herpes recurrence. Psychosom Med. 1989 Mar-Apr;51(2):195–208. doi: 10.1097/00006842-198903000-00008. [DOI] [PubMed] [Google Scholar]
- Lewis G., Wessely S. Comparison of the General Health Questionnaire and the Hospital Anxiety and Depression Scale. Br J Psychiatry. 1990 Dec;157:860–864. doi: 10.1192/bjp.157.6.860. [DOI] [PubMed] [Google Scholar]
- Logan R. A. Self help groups for patients with chronic skin diseases. Br J Dermatol. 1988 Apr;118(4):505–507. doi: 10.1111/j.1365-2133.1988.tb02459.x. [DOI] [PubMed] [Google Scholar]
- Luby E. D., Klinge V. Genital herpes. A pervasive psychosocial disorder. Arch Dermatol. 1985 Apr;121(4):494–497. [PubMed] [Google Scholar]
- Manne S., Sandler I. Coping and adjustment to genital herpes. J Behav Med. 1984 Dec;7(4):391–410. doi: 10.1007/BF00845272. [DOI] [PubMed] [Google Scholar]
- Mayou R. Psychological morbidity in a clinic for sexually transmitted disease. Br J Vener Dis. 1975 Feb;51(1):57–60. doi: 10.1136/sti.51.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedder J. R., Goldberg D. P. A survey by questionnaire of psychiatric disturbance in patients attending a venereal diseases clinic. Br J Vener Dis. 1970 Feb;46(1):58–61. doi: 10.1136/sti.46.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand K. H., Hoon E. F., Massey J. K., Johnson J. H. Daily stress and recurrence of genital herpes simplex. Arch Intern Med. 1990 Sep;150(9):1889–1893. [PubMed] [Google Scholar]
- VanderPlate C., Aral S. O. Psychosocial aspects of genital herpes virus infection. Health Psychol. 1987;6(1):57–72. doi: 10.1037//0278-6133.6.1.57. [DOI] [PubMed] [Google Scholar]
- Wells W. P. Personality study of V.D. patients. Using the psychoticism, extroversion, neuroticism inventory. Br J Vener Dis. 1970 Dec;46(6):498–501. doi: 10.1136/sti.46.6.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessely S. C., Lewis G. H. The classification of psychiatric morbidity in attenders at a dermatology clinic. Br J Psychiatry. 1989 Nov;155:686–691. doi: 10.1192/s0007125000018201. [DOI] [PubMed] [Google Scholar]


