Abstract
Abstract
Background
The involvement of male partners in the care and treatment of HIV-positive pregnant women is essential for improving health outcomes and ensuring optimal adherence to antiretroviral therapy (ART). Although ART has been shown to be effective in preventing mother-to-child transmission of HIV, maintaining adherence to the prescribed triple ART regimen remains a significant challenge. However, there has been a lack of research on the role of male partners in supporting ART adherence during pregnancy.
Objective
To assess male partner involvement in triple ART drug adherence and associated factors among HIV-positive pregnant women in government hospitals of the North Gojjam Zone, Amhara Region, Northwest Ethiopia, 2023.
Design
An institution-based cross-sectional study was conducted.
Setting
The study was carried out in hospitals located in the North Gojjam Zone of Northwest Ethiopia.
Participants
The study was conducted among 410 male partners of HIV-positive pregnant women from 1 April 2023 to 30 May 2023.
Primary and secondary outcomes
The primary outcome was to assess the involvement of male partners in triple ART adherence, while the secondary outcome was to identify factors associated with the involvement of male partners on triple ART adherence among HIV-positive pregnant women. The association between variables was assessed using bivariate and multivariable logistic regression models, and a p value <0.05 with a 95% CI was considered statistically significant.
Results
A total of 410 participants were included, with a response rate of 97.2%. The prevalence of male partner involvement in triple ART drug adherence among HIV-positive pregnant women was 21.2%. Multivariable logistic regression showed that educational status (AOR (Adjusted Odds Ratio)=2.5, 95% CI 1.26 to 4.96), place of residence (AOR=4.8, 95% CI 3.17 to 7.27), and the time taken to travel from home to the facility (AOR=3.1, 95% CI 1.51 to 6.36) were significantly associated with male partner involvement.
Conclusion
This study demonstrates that compared with a study conducted in Malawi, male partner involvement in triple ART drug adherence was lower. Male partner involvement in triple ART adherence among HIV-positive pregnant women was strongly associated with educational status, place of residence and the time taken to travel from home to the health facility. Empowering men to actively participate in healthcare decisions and treatment plans for their partners can foster a sense of responsibility and enhance commitment to adherence.
Keywords: Chronic Disease, Health, INFECTIOUS DISEASES, Public health, Midwifery, Pregnancy
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study highlights the critical role of male involvement in antiretroviral therapy adherence.
The study captures real-world experiences and barriers by engaging participants directly.
The study’s cross-sectional nature prevents establishing causal relationships.
Self-reported responses may be influenced by participants’ recall ability.
Future studies should explore male involvement in diverse cultural contexts.
Introduction
Adherence is critical to the success of antiretroviral therapy (ART). Optimal adherence is essential to achieve favourable ART outcomes, including reduced drug resistance, slowed disease progression, fewer hospitalisations, delayed mortality and improved overall health, longevity and quality of life.1 Male involvement (MI) is crucial in maternal and child health (MCH) and the prevention of mother-to-child transmission (PMTCT) of HIV in Sub-Saharan Africa (SSA). Given men’s significant role in household decision-making, their involvement directly affects women’s access to healthcare, contraception, nutrition, employment and pregnancy outcomes. 2ART is a key component of the prevention of the PMTCT service package, known as the WHO-pronged approach to PMTCT. Among its prongs, prong 3 focuses on preventing HIV transmission from an HIV-positive mother to her child through ART and other interventions during pregnancy, childbirth and breastfeeding. This approach aims to reduce vertical transmission and is part of a broader strategy that includes HIV prevention for women of reproductive age, family planning and long-term HIV care and treatment.3
The success of ART is undermined by inadequate long-term adherence, which leads to subtherapeutic drug levels and drug resistance, potentially transmissible to others. As a result, maintaining adherence has become a critical concern, requiring ongoing attention to prevent or delay resistance.4
Although women are retained in care, adherence to ART remains a challenge. England has faced significant obstacles that impact treatment adherence during pregnancy.5 MI has been identified as a key priority in the prevention of PMTCT of HIV programmes.6 In addition to preventing mother-to-child transmission of HIV, MI in PMTCT plays a crucial role in promoting family health and ensuring adherence to HIV treatment and prevention strategies.7
Evidence indicates that increasing MI can improve maternal ART uptake, infant prophylaxis and HIV testing rates and reduce infant HIV infections. Additionally, it strengthens couple relationships by enhancing communication, relationship quality and shared decision-making. Interventions in Tanzania and Zimbabwe have shown that fostering love and intimacy leads to greater male support in MCH and domestic responsibilities. Furthermore, male partner support helps mitigate social and economic challenges related to the disease and promotes adherence to treatment.8
Partner attendance at antenatal care (ANC) has been linked to a reduced risk of infant HIV transmission and lower infant mortality.9 MI is linked to improved social support, including men’s ability to provide advice on HIV testing, financial assistance for transportation and other pregnancy-related needs, accompaniment to ANC, and emotional encouragement.10 Studies have shown that the utilisation of PMTCT services by pregnant women is influenced both by factors related to the health system such as accessibility of voluntary counselling and testing services and by individual factors such as fear of disclosure of HIV results, lack of male partner support, fear of domestic violence, abandonment and stigmatisation.11
The lack of MI is a commonly reported barrier to initiating ART and maintaining retention in care.12 Studies in Tanzania have found that men are often marginalised in the context of PMTCT services.13 One of the challenges facing PMTCT programmes in SSA is the lack of support from male partners.14
In Africa, MI in PMTCT services is generally low due to several factors, including low overall health service utilisation, limited knowledge among men about PMTCT compared with women, reluctance to know their HIV status, conflicts between ANC/PMTCT schedules and men’s work hours and women’s fear of domestic violence if they test HIV-positive.14 Fear of stigmatisation and the belief that men should not be involved in female reproductive health are significant barriers to male participation.15
The WHO and other public health organisations advocate for male partner involvement as a strategy to enhance women’s adherence.16 However, little is known about how women themselves view and experience male partner support.
In Ethiopia, as well as across Africa and globally, the role of male partner involvement in triple ART drug adherence among HIV-positive women remains unclear. The findings of this study provide new insights into male partner involvement in ART adherence. This research has the potential to improve the effectiveness of PMTCT programmes in Ethiopia, contributing to the elimination of mother-to-child transmission in the study area and other regions of the country. It may also benefit health professionals and service administrators by providing evidence-based practices and guiding interventions for the identified factors. Additionally, this study will serve as a valuable reference and foundation for future research on male partner involvement in ART adherence among HIV-positive pregnant women. Therefore, the aim of this study was to assess male partner involvement in triple ART drug adherence and associated factors among HIV-positive pregnant women in government hospitals of the North Gojjam Zone, Amhara Region, Northwest Ethiopia.
Methods and materials
Study design and period
An institution-based cross-sectional study was conducted from 1 April 2023 to 30 May 2023.
Study area
The study was conducted in government hospitals within the North Gojjam Zone, one of the 15 zones in the Amhara region. The administrative centre of the North Gojjam Zone is Bahir Dar, located 562 km from Addis Ababa. According to the 2023 population projection, the zone has a total population of 1 539 874 people. It is served by five government hospitals and 57 health centres.
Source population
The study included all HIV-positive men who are partners of HIV-positive pregnant women and are receiving ART follow-up at government hospitals in the North Gojjam Zone.
Study population
The study included selected all HIV-positive men who are partners of HIV-positive pregnant women and received ART follow-up at government hospitals in the North Gojjam Zone during the study period.
Inclusion criteria
The study included HIV-positive men who are partners of HIV-positive pregnant women and are receiving ART follow-up at government hospitals in the North Gojjam Zone.
Exclusion criteria
All HIV-positive men who are partners of HIV-positive breastfeeding women and are undergoing ART follow-up were excluded from the study.
Sample size determination
The sample size was calculated using a single-population proportion formula with a 95% CI, a 5% margin of error and a 50% proportion, as no prior study data were available.
n=Z2 p (1 p)/w2=(1.96)2(0.871×0.129)/(0.05)2=384. After accounting for a 10% non-response rate, the final sample size was adjusted to 422.
Sampling technique and procedure
The study included all five hospitals in the North Gojjam Zone. The sample was proportionally distributed across these health facilities as follows: Merawi Primary Hospital (92 participants), Adet Primary Hospital (84 participants), Duribetie Primary Hospital (71 participants), Goji Kondela Primary Hospital (79 participants) and Liban Primary Hospital (84 participants). The ART registration book served as the sampling frame, and a lottery-style random sampling method was used to select the participants. Interviews were conducted at the government hospitals in the North Gojjam Zone during participants’ follow-up visits.
Variables
Dependent variable
Male partner involvement on triple ART drug adherence.
Independent variables
-
Sociodemographic characteristics
Place of residence
Level of education
Occupational status
Marital status
-
Health system-related factors
Type of health facility
Distance
HIV disclosure status
Operational definition of variables
Adherence
Adherence measures the extent to which individuals follow medical treatments and health recommendations17). It is often assessed using self-reported questionnaires or interviews. Adherence scores are classified as:
Good adherence (≥95%)
Moderate adherence (80%–94%)
Poor adherence (<80%)
Male partner involvement
In terms of male partner support, involvement was deemed good for those who scored ≥50% and poor for those who scored <50%.18
Data collection tools and procedures
Data were collected through face-to-face interviews using a standardised, structured questionnaire, which was adapted from a previously validated instrument.18 19 To ensure consistency in the questions, the questionnaire was initially written in English, then translated into Amharic, and subsequently retranslated into English by language specialists. The questionnaire included sections on sociodemographic information, male partner involvement and HIV disclosure status. Five diploma-trained midwives served as data collectors, while five midwives with bachelor’s degrees acted as supervisors during the administration of the structured questionnaire.
Supplementary materials
The tools are in the supplementary material (online supplemental file 1).
Data quality control
A pretest of the questionnaire was conducted at the Chara Centre, which was not part of the study, using 5% of the sample population. This was done to ensure the questions were clear, organised, comprehensive and easy to understand. Based on the pretest results, the questionnaire was revised as needed.
Before the actual data collection began, the data collectors were trained in sampling methods and data collection techniques. Supervisors and investigators reviewed the completed questionnaires daily to ensure the accuracy and consistency of the data.
Data analysis and presentation
After being coded, cleaned and imported into EPI (Epidemiological and Public Health Information)-Data .4.1, the data were exported to SPSS V.27 for analysis. Descriptive analysis was conducted, summarising the data using frequency tables and graphs.
Variables with a p value <0.25 in the bivariate analysis were included in a multivariate logistic regression model to examine their relationship with the dependent variable. An adjusted OR and a p value ≤0.05 with a 95% CI were used to determine statistically significant associations between the independent predictors and the outcome variable.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Results
Sociodemographic characteristics of the respondents
The study included 410 male partners, with a response rate of 97.2%. Of these men, 285 (69.5%) were aged between 36 and 45 years, with a mean age of 27.82 years and an SD of approximately ±5.45 years. Furthermore, 274 (66.8%) were married, and 285 (69.5%) had received formal education (table 1).
Table 1. Sociodemographic characteristics of participants in government hospitals of North Gojjam Zone, Northwest Ethiopia, 1 April–30 May 2023 (N=410).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age of male partners | ||
| 25–35 | 78 | 19.0 |
| 36–45 | 285 | 69.5 |
| 46–60 | 47 | 11.5 |
| Place of residence | ||
| Urban | 246 | 60.0 |
| Rural | 164 | 40.0 |
| What is your religion? | ||
| Orthodox Christian | 315 | 76.9 |
| Muslim | 46 | 11.2 |
| Protestant Christian | 32 | 7.8 |
| Catholic | 17 | 4.1 |
| What is your marital status? | ||
| Single | 16 | 3.9 |
| Married | 274 | 66.8 |
| Divorced | 78 | 19.1 |
| Widowed | 42 | 10.2 |
| Level of education | ||
| No formal education | 125 | 30.5 |
| Have formal education | 285 | 69.5 |
| Current occupation | ||
| Merchant | 201 | 49.0 |
| Private employee | 54 | 13.2 |
| Governmental employee | 94 | 22.9 |
| Farmer | 61 | 14.9 |
| Time taken to reach home to facility | ||
| <1 hour | 332 | 81.0 |
| >1 hour | 78 | 19.0 |
HIV status disclosure of the respondents
Among the total participants, the majority had disclosed their HIV status. Specifically, 74.5% had shared their status with their wives, 14.4% had informed family members, and 10.9% had disclosed it to their friends (table 2).
Table 2. HIV status disclosure of male partners in governmental hospitals of North Gojjam Zone, Northwest Ethiopia, 1 April–30 May 2023 (N=410).
| Question | Frequency | Percentage (%) |
|---|---|---|
| Did you disclose your status to anyone? | ||
| Yes | 275 | 69.1 |
| No | 135 | 32.9 |
| For whom you disclose? (n=275) | ||
| Wife | 204 | 74.2 |
| Family | 41 | 14.9 |
| Friend | 30 | 10.9 |
| Did you help your partner take her pills regularly on time? | ||
| Yes | 298 | 72.7 |
| No | 112 | 27.3 |
| Did you fear stigma and discrimination? | ||
| Yes | 77 | 18.8 |
| No | 333 | 81.2 |
| Did you know ways of MTCT of HIV? | ||
| Yes | 228 | 55.6 |
| No | 182 | 44.4 |
MTCT, mother-to-child transmission.
Male partners' involvement in triple ART drug adherence
Most respondents shared household decision-making with their wives (64.9%) and were aware of the frequency of taking PMTCT drugs (75.9%). However, more than half of the respondents were unaware of the dosage (92%) or the names (90%) of the PMTCT drugs (table 3).
Table 3. Male partners' involvement in triple ART drug adherence in governmental hospitals of North Gojjam Zone, Northwest Ethiopia, 1 April–30 May 2023 (N=410).
| S.no | Male involvement activities | YesN (%) | NoN (%) |
|---|---|---|---|
| 401 | Shares his wife decisions on household issues | 266 (64.9) | 144 (35.1) |
| 402 | Discusses with his wife on use of condom during sex | 102 (24.9) | 308 (75.1) |
| 403 | Knows the frequency of taking PMTCT drug | 311 (75.9) | 99 (24.1) |
| 404 | Visits PMTCT clinic with his wife to bring ARV drugs | 62 (15.1) | 348 (84.9) |
| 405 | Knows the name of PMTCT drugs | 41 (10.0) | 369 (90.0) |
| 406 | Knows the doses of PMTCT drugs | 33 (8.0) | 377 (92.0) |
| 407 | Discusses the advantages of ANC/PNC appointment | 74 (18.0) | 336 (82.0) |
| 408 | Supports his wife financially to visit ANC/PNC PMTCT | 70 (17.1) | 340 (82.9) |
| 409 | Attends PMTCT with his wife | 66 (16.1) | 344 (83.9) |
| 410 | Reminds his wife about ANC/PNC PMTCT appointment | 80 (19.5) | 330 (80.5) |
ANC, antenatal care; ART, antiretroviral therapy; ARV, antiretroviral therapy; PMTCT, prevention of mother-to-child transmission; PNC, post natal care.
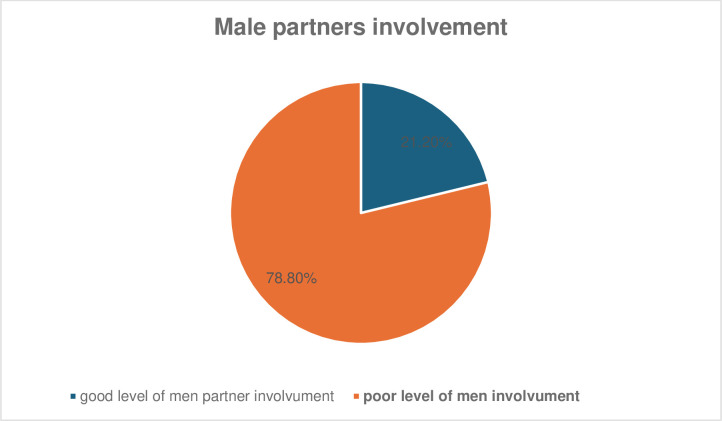
Of the total respondents, 21.2% reported low levels of partner involvement in triple ART adherence (figure 1). Prevalence of male partner involvement in triple ART drug adherence and associated factors among HIV-positive pregnant women in government hospitals of the North Gojjam Zone, Amhara Region, Northwest Ethiopia, 2023: a multicentre cross-sectional study.
Figure 1. Prevalence of male partner involvement in triple ART drug adherence and associated factors among HIV-positive pregnant women in government hospitals of the North Gojjam Zone, Amhara Region, Northwest Ethiopia, 2023: a multicentre cross-sectional study. ART, antiretroviral therapy.
Factors associated with men partner involvement in triple ART drug adherence
Bivariate logistic regression analysis revealed that educational status, place of residence, marital status, fear of stigma and discrimination, time taken to reach health facilities and disclosure status were significantly associated with male partner involvement in Option B+ PMTCT drug adherence. However, in the multivariable logistic regression analysis, educational status, place of residence and travel time to health facilities were found to be significantly associated with male partner involvement in triple ART drug adherence.
Participants with formal education were 2.5 times more likely to engage in triple ART adherence compared with those without formal education (AOR=2.5, 95% CI 1.26–4.96).
Participants who took <60 min to reach health facilities were 3.1 times more likely to engage in triple ART adherence compared with those who travelled 60 min or more (AOR=3.1, 95% CI 1.51–6.36).
Study participants living in urban areas were 4.8 times more likely to be involved in triple ART adherence compared with those living in rural areas (AOR=4.8, 95% CI 3.17 to 7.27) (table 4).
Table 4. Bivariate and multivariate logistic regression analysis for factors associated with men partner involvement in triple ART drugs adherence in government hospitals of North Gojjam Zone, Northwest Ethiopia, 1 April–30 May 2023 (N=410).
| Variables | Men partner involvement | OR | P value | ||
|---|---|---|---|---|---|
| Goodn (%) | Poorn (%) | COR (95% CI) | AOR (95% CI) | ||
| Educational level | |||||
| Have formal education | 249 (60.7) | 36 (8.8) | 4.6 (1.86–11.38) | 2.5 (1.26 to 4.96) | 0.01* |
| No formal education | 75 (18.3) | 50 (12.2) | 1 | 1 | 1 |
| Place of residence | |||||
| Urban | 190 (46.3) | 56 (13.7) | 2.9 (1.17–7.19) | 4.8 (3.17 to 7.27) | 0.02* |
| Rural | 89 (21.7) | 75 (18.3) | 1 | 1 | 1 |
| Time taken to reach from home to facility | |||||
| <60 min | 275 (67.1) | 57 (13.9) | 3.5 (2.65–4.62) | 3.1 (1.51 to 6.36) | 0.002* |
| ≥60 min | 45 (11.0) | 33 (8.0) | 1 | 1 | 1 |
| Marital status | |||||
| Single | 7 (1.7) | 9 (2.2) | 0.3 (0.13–0.69) | 0.6 (0.32 to 1.12) | 0.33 |
| Married | 246 (60.0) | 28 (6.8) | 3.5 (2.81–4.36) | 2.4 (0.72 to 7.58) | 0.09 |
| Divorced | 51 (12.4) | 27 (6.6) | 0.8 (0.65–0.98) | 0.9 (0.52 to 1.56) | 0.06 |
| Widowed | 30 (7.3) | 12 (2.9) | 1 | 1 | 1 |
| Fear of stigma and discrimination | |||||
| No | 279 (68.0) | 54 (13.2) | 4.8 (3.65–6.31) | 3.4 (0.91 to 12.70) | 0.6 |
| Yes | 40 (9.8) | 37 (9.0) | 1 | 1 | 1 |
| Disclosure status to anyone? | |||||
| Yes | 248 (60.5) | 40 (9.8) | 3.2 (1.32–7.76) | 3.5 (0.98 to 12.50) | 0.73 |
| No | 80 (19.5) | 42 (10.2) | 1 | 1 | 1 |
P value ≤0.05 is statistically significant.
AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio.
Discussion
Our study found that the prevalence of male partner involvement in triple ART drug adherence was 21.2% (95% CI 17.2% to 23.72%). Women whose partners were actively involved were more likely to adhere to their triple ART regimen. This involvement was significantly associated with improved adherence to triple ART drugs among HIV-positive pregnant women in the North Gojjam Zone.
Our study found a lower prevalence of male partner involvement (2%)20 compared to studies conducted in East Africa21 and in Malawi (60%)20. This discrepancy may be due to differences in study settings, where the impact of MI was less pronounced, possibly due to varying social dynamics and access to healthcare.
However, this study found higher male partner involvement compared to research conducted in Kampala, Uganda, where male participation in PMTCT activities was reported to be low (16%).22 This difference may be attributed to variations in sample size, study period, as well as differences in the participants’ awareness and knowledge.
In this study, having formal education (AOR=2.5, 95% CI 1.26 to 4.96, p=0.01) was significantly associated with male partner involvement in triple ART drug adherence among HIV-positive pregnant women. This finding is consistent with results from previous studies in East Shewa, Ethiopia,23 Kenya and Ghana.24 25 A possible explanation for this finding is that men with formal education have better access to information about the importance of adhering to triple ART therapy for HIV-positive pregnant women. Education may empower them to make informed decisions regarding healthcare and help them understand the benefits of adherence in preventing transmission of the virus to the baby. Educated individuals are also more likely to be proactive in seeking healthcare and involving their family members, including partners, in health-related activities.
Research indicates that higher education levels among women are associated with better adherence to triple ART services, due to improved health literacy and decision-making skills. Educated women are also more likely to involve their partners in healthcare processes, which can enhance adherence to PMTCT programmes. However, some studies suggest that the impact of education on health outcomes may vary depending on local contexts and the availability of supportive resources.26
Participants in urban areas were 4.8 times more likely to be involved in triple ART drug adherence for HIV-positive pregnant women compared to those living in rural areas. This finding is consistent with a study conducted in the eastern zone of Tigray, Ethiopia.27 This could be because urban areas typically offer better access to healthcare facilities, information and resources compared to rural areas in Ethiopia. Men living in urban areas may have easier access to HIV treatment services, including triple ART drugs, and are more likely to be aware of the importance of adherence due to better education and greater exposure to health campaigns. Additionally, urban areas often have more support systems and infrastructure in place to assist individuals in adhering to their treatment regimens. Studies suggest that rural residents face more significant barriers to healthcare access, which can negatively impact adherence rates.28
Participants who travelled <60 minutes to reach health facilities were 3.1 times more likely to be involved in triple ART drugs adherence on HIV-positive pregnant women compared to those who travelled 60 minutes or more to reach these facilities. This finding is also supported by the study conducted in South Africa.29 The proximity of healthcare facilities improves accessibility, reduces costs, minimises disruptions and enhances patient-provider relationships, all of which contribute to higher rates of male partner involvement in triple ART drug adherence. The time and distance required to reach health facilities can influence the frequency of healthcare visits and adherence to PMTCT drug regimens. Longer travel times may discourage consistent attendance and participation
Conclusion
This study shows that compared with a study conducted in Malawi, male partner involvement in triple ART drug adherence was lower. Male partner involvement in ART adherence among HIV-positive pregnant women was strongly associated with educational status, place of residence and the time taken to reach health facilities. Addressing these factors through targeted interventions can enhance MI and improve adherence rates, ultimately leading to better health outcomes for HIV-positive pregnant women. By encouraging greater male partner involvement, we can strengthen the effectiveness of PMTCT programmes and improve health outcomes for HIV-positive pregnant women.
Supplementary material
jAcknowledgements
We would like to thank Debre Tabor University for its ethical letter and financial support. Our gratitude is also great to all data collectors and study participants. We are also glad to North Gojjam public health institutions for writing a permission letter.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-096713).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Consent obtained directly from patient(s).
Ethics approval: This study involves human participants and was approved by the Ethical Review Committee (ERC) of Debre Tabor University, College of Health Science with the reference number DTU 0792/2023. Written informed consent was obtained from all study participants. They were informed about the purpose and procedures of the study, as well as its potential advantages and disadvantages. Participation was entirely voluntary, and all personal information was kept confidential. Participants were also made aware of their right to withdraw from the study at any time. To ensure confidentiality, no personal identifiers, such as names or phone numbers, were recorded. Written informed consent was obtained before data collection commenced. Participants gave informed consent to participate in the study before taking part.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Data availability statement
Data are available upon reasonable request.
References
- 1.Aluisio A, Richardson BA, Bosire R, et al. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr . 2011;56:76–82. doi: 10.1097/QAI.0b013e3181fdb4c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amano A, Musa A. Male involvement in PMTCT and associated factors among men whom their wives had ANC visit 12 months prior to the study in Gondar town, North west Ethiopia, December, 2014. Pan Afr Med J . 2014;24 doi: 10.11604/pamj.2016.24.239.8460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayuo P, Musick B, Liu H, et al. Frequency and factors associated with adherence to and completion of combination antiretroviral therapy for prevention of mother to child transmission in western Kenya. J Int AIDS Soc. 2013;16 doi: 10.7448/IAS.16.1.17994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boateng D, Kwapong GD, Agyei-Baffour P. Knowledge, perception about antiretroviral therapy (ART) and prevention of mother-to-child-transmission (PMTCT) and adherence to ART among HIV positive women in the Ashanti Region, Ghana: a cross-sectional study. BMC Womens Health . 2013;13:2. doi: 10.1186/1472-6874-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter MW. “Because he loves me”: Husbands’ involvement in maternal health in Guatemala. Cult Health Sex. 2002;4:259–79. doi: 10.1080/13691050110112784. [DOI] [Google Scholar]
- 6.De Allegri M, Agier I, Tiendrebeogo J, et al. Factors Affecting the Uptake of HIV Testing among Men: A Mixed-Methods Study in Rural Burkina Faso. PLoS One. 2015;10:e0130216. doi: 10.1371/journal.pone.0130216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebuy H, Yebyo H, Alemayehu M. Level of adherence and predictors of adherence to the Option B+ PMTCT programme in Tigray, northern Ethiopia. Int J Infect Dis. 2015;33:123–9. doi: 10.1016/j.ijid.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Elias M, Mmbaga EJ, Mohamed AA, et al. Male partner involvement in the prevention of mother to child transmission of HIV infection in Mwanza Region, Tanzania. Pan Afr Med J. 2017;27:90. doi: 10.11604/pamj.2017.27.90.8901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falnes EF, Moland KM, Tylleskär T, et al. “It is her responsibility”: partner involvement in prevention of mother to child transmission of HIV programmes, northern Tanzania. J Int AIDS Soc. 2011;14:21. doi: 10.1186/1758-2652-14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gebremedhin H, Degefa H, Tsegay A. Male partner involvement among HIV positive women receiving option b+ prevention of mother to child transmission of HIV and its associated factors, Eastern zone, Tigray, Ethiopia. Int J Dev Res. 2019;9:29014–8. [Google Scholar]
- 11.Gourlay A, Birdthistle I, Mburu G, et al. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16:18588. doi: 10.7448/IAS.16.1.18588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalembo FW, Zgambo M, Mulaga AN, et al. Association between male partner involvement and the uptake of prevention of mother-to-child transmission of HIV (PMTCT) interventions in Mwanza district, Malawi: a retrospective cohort study. PLoS One. 2013;8:e66517. doi: 10.1371/journal.pone.0066517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lencha M. Adherence to option B+ and associated factors among pregnant women on PMTCT Services at Public Health Facilities of east Shawa zone, Oromia, Ethiopia. J Womens Health Reprod Med. 2018:2. doi: 10.1016/j.srhc.2019.100459. [DOI] [PubMed] [Google Scholar]
- 14.Mandelbrot L, Tubiana R, Le Chenadec J, et al. No perinatal HIV-1 transmission from women with effective antiretroviral therapy starting before conception. Clin Infect Dis. 2015;61:1715–25. doi: 10.1093/cid/civ578. [DOI] [PubMed] [Google Scholar]
- 15.Morfaw F, Mbuagbaw L, Thabane L, et al. Male involvement in prevention programs of mother to child transmission of HIV: a systematic review to identify barriers and facilitators. Syst Rev. 2013;2:1–13. doi: 10.1186/2046-4053-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nachega JB, Uthman OA, Anderson J, et al. Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries: a systematic review and meta-analysis. AIDS . 2012;26:2039–52. doi: 10.1097/QAD.0b013e328359590f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakatani H, Mafubelu D. Preventing mother‑to‑child transmission of HIV to reach the UNGASS and millennium development goals, 2015. PMTCT Strategic Vision; 2010. [Google Scholar]
- 18.Ngianga-Bakwin K, Lawrence K. Statistical modelling of complex correlated and clustered data household surveys in Africa. New York: NOVA; 2019. [Google Scholar]
- 19.Organization WH Global update on HIV treatment 2013: results, impact and opportunities. 2013
- 20.Osman RJ, Unkels R, Aliyu U, et al. Barriers to male involvement in uptake of Prevention-of-Mother-to-Child-Transmission (PMTCT) of HIV in Sub-Saharan Africa. Medico Research Chronicles. 2014;1:21–9. [Google Scholar]
- 21.Organization WH Implementation of option b+ for prevention of mother-to-child transmission of HIV. 2014
- 22.Ramadhani HO, Thielman NM, Landman KZ, et al. Predictors of incomplete adherence, virologic failure, and antiviral drug resistance among HIV-infected adults receiving antiretroviral therapy in Tanzania. Clin Infect Dis. 2007;45:1492–8. doi: 10.1086/522991. [DOI] [PubMed] [Google Scholar]
- 23.Semrau K, Kuhn L, Vwalika C, et al. Women in couples antenatal HIV counseling and testing are not more likely to report adverse social events. AIDS. 2005;19:603–9. doi: 10.1097/01.aids.0000163937.07026.a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skinner D, Mfecane S, Gumede T, et al. Barriers to accessing PMTCT services in a rural area of South Africa. Afr J AIDS Res. 2005;4:115–23. doi: 10.2989/16085900509490350. [DOI] [PubMed] [Google Scholar]
- 25.Steel G, Nwokike J, Joshi MP. Development of a multi-method tool to measure ART adherence in resource-constrained settings: the South Africa experience. RPM Plus. 2007;6 [Google Scholar]
- 26.Triulzi I, Somerville C, Sangwani S, et al. Understanding the meanings of male partner support in the adherence to therapy among HIV-positive women: a gender analysis. Glob Health Action. 2022;15:2051223. doi: 10.1080/16549716.2022.2051223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vermeulen E, Solnes Miltenburg A, Barras J, et al. Opportunities for male involvement during pregnancy in Magu district, rural Tanzania. BMC Pregnancy Childbirth. 2016;16:66. doi: 10.1186/s12884-016-0853-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wesevich A, Mtande T, Saidi F, et al. Role of male partner involvement in ART retention and adherence in Malawi’s Option B+ program. AIDS Care. 2017;29:1417–25. doi: 10.1080/09540121.2017.1308464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO U The interagency task team (IATT) on prevention of HIV. Guidance on global scale-up of the prevention of mother-to-child transmission of HIV towards universal access for women, infants and young children and eliminating HIV and AIDS among children. 2007