Abstract
Background
The traditional approach to talocalcaneal tarsal coalition (TCC) excision is medial through the deltoid ligament. Unfortunately, there are few anatomic markers to guide the surgeon. Preoperative planning includes radiographs and advanced imaging; these currently provide little help guiding the excision. Our method of mapping the coalition on advanced imaging accurately defines where to make osteotomies in the operating room.
Methods
A retrospective review was conducted of TCC patients with preoperative computed tomography (CT) at a single institution from 2010 to 2022. Three independent raters reported sagittal TCC length relative to the talus. Raters further quantified TCC coronal depth and height across distal, middle, and proximal thirds of the TCC relative to the sustentaculum talus. This guidance directs two osteotomy cuts through the coalition directly into the normal lateral subtalar joint for complete and accurate excision of the coalition. CT measurement inter-rater reliability was determined using intra-class correlation.
Results
Twenty-seven patients (16 male), average age 13.9 ± 2.4, met study criteria. TCCs were located on the right lower extremity in 10/27 cases. Sixteen/twenty-seven coalitions were horizontal, 10/27 was down sloping, and 1/27 was upsloping relative to the joint line. Substantial agreement was achieved between three raters (mean average measures intraclass correlation 0.781). The mean coalition length in the sagittal plane was 21.2 ± 6.0 mm, covering 49.6 ± 23.2% of the talar length.
Conclusion
This study describes a 3D preoperative mapping technique with high reproducibility among the present raters to resect the TCC with direct vision of the normal subtalar joints. Alternative approaches, such as obtaining CT imaging intraoperatively, expose the patient to increased radiation and anesthesia, incurring higher financial and time costs. We report a concise, readily applicable, and systematic method to map TCCs on preoperative CT and provide direct vision of the normal subtalar (talar and calcaneal) joints, as well as close to normal subtalar motion.
Key Concepts
-
(1)
To date, very little in the way of intraoperative planning for TCCs has been proposed in the literature, even though advanced imaging has been widely used preoperatively.
-
(2)
Our method of mapping coalitions on preoperative CT may assist with intraoperative resection. Additionally, this method demonstrates the three-dimensional variety that can be expected in surgical excision of these coalitions.
-
(3)
Neither the medial to lateral depth nor the distance proximal from the sustentaculum talus was uniform as the coalitions were thickest centrally and tapered both proximally and distally.
Level of Evidence
IV
Keywords: Talocalcaneal tarsal coalition, Preoperative CT, Subtalar joint, Talus
Introduction
Talocalcaneal coalitions (TCCs) of the medial facet are developmental malformations in which the talus and calcaneus fail complete separation during fetal development and a persistent tissue bridge remains. With age, the tissue between these two bones will ossify, progressively reducing the motion about the subtalar joint [1]. In the case of a symptomatic coalition, open surgical resection is indicated [2]. Excision is well established in the literature and traditionally requires a medial approach through the deltoid ligament [3]. Unfortunately, there are few anatomic landmarks to guide the surgeon through resection [3,4].
Previously, Rozansky’s classification of TCC from computed tomography (CT) scans emphasized the value of preoperative CT in defining coalition size, location, and orientation [4,5]. Similarly, preoperative magnetic resonance imaging now offers a way to gauge TCC width [6]. Although these advanced imaging analyses and subsequent categorizations are recommended for surgical guidance; it is difficult to transpose these measurements to the actual surgical intervention.
Therefore, as some authors have called for a tailored approach to excision based on symptoms and size of the coalition seen on pre-operative imaging, the following study seeks to offer this guidance [7]. This study describes a method of mapping coalitions on pre-operative CT imaging that may assist with intra-operative resection. Additionally, this method demonstrates the three-dimensional variety that can be expected in surgical excision of these coalitions.
Materials and methods
Following Institutional Review Board approval at a single, tertiary care children's hospital, a retrospective review was conducted of TCC patients undergoing surgical excision from 2010 to 2022. Those included were ≤18 years old at the time of surgical excision with preoperative computed tomography (CT) scans. Patients with neuromuscular comorbidities or recurrent TCC were excluded.
Demographic data, including race, ethnicity, and age, were recorded from the electronic medical record. Postoperative complications according to the modified Clavien-Dindo-Sink (M-CDS) classification system were collected.
Two CT raters were pediatric orthopaedic foot and ankle surgeons, each with several decades of experience. One additional rater was a pediatric orthopaedic research fellow with less than one year of experience performing advanced imaging measurements. Each of the three independent raters reported TCC location relative to the talus and calcaneus on the most prominent sagittal slice (Fig. 1A). The location was noted to be posterior third, middle third, or distal third. This sagittal CT cut showing the maximum length of the coalition from posterior to distal was chosen for measurement of the maximum length of the coalition, “h,” from distal to posterior and compared to the length of the talus from posterior to anterior, “j” (Fig. 1A).
Figure 1.
A. The sagittal CT cut chosen demonstrates the maximum length and location of the coalition with respect to the sagittal length of the talus. Note: “h” is the measured length of the coalition and its location posterior to distal with respect to “j,” the length of the talus. B–D. Posterior, middle, anterior coronal aspects of the coalition on CT. Three parallel lines are drawn. Line “a” is along the inferior aspect of the sustentaculum talus. A second, “b” is at the level of the calcaneal subtalar joint. A third, “c” is along the talar aspect of the subtalar joint. The distance “y” between “a” and “b” and the distance “x” between “a” and “c” are measured. A third measure, “z” is the measured depth of the coalition from medial to the normal lateral subtalar joint. E, F. Using the measurements of 1A-D above the dashes and arrows demonstrate the suggested osteotomy cuts to be used intraoperatively. CT, computed tomography.
Then, at least three coronal cuts were chosen at the distal (Fig. 1D), middle (thickest, Fig. 1C), and posterior (Fig. 1B) portions of the coalition as the shape of the coalition varies along its length. The inferior aspect of the sustentaculum talus was chosen as it is the only intraoperative location easily identifiable in a medial approach to a TCC. The goal of surgery is to excise the entire coalition from medial to lateral and posterior to distal, exposing the typical lateral portions of the subtalar joint. To accomplish this, three parallel lines are drawn on each of the three CT coronal cuts. One is drawn parallel to the inferior aspect of the sustentaculum talus (“a”), one through the lateral subtalar surface of the calcaneus (“b”) and another through the lateral subtalar surface of the talus (“c”), as seen in Fig. 1B–D. The orthogonal distance of these lines from the inferior sustentaculum talus is measured as “y” and “x” as in Fig. 1B–D. The medial to lateral depth of the coalition (“z”) is measured. It should be noted that measurements “x, y, and z” will vary along the length of the coalition, explaining the need for measurements of at least three coronal cuts along the coalition.
Measurements were repeated by each rater a month apart. CT measurement inter-rater and intrarater reliability were determined using two-way mixed average measures intraclass correlation. Descriptive statistics were performed to summarize demographics and TCC characteristics. All analyses were performed in IBM SPSS v29.0.
Osteotomies along these measurements (as described in Fig. 1E and F) guide the intraoperative excision. Operatively, the patient was placed in the supine position and underwent general anesthesia. A medial incision was made from the posteromedial subtalar/ankle joint through a point halfway between the medial malleolar tip and the plantar aspect of the sustentaculum talus to the medial aspect of the navicular.
The posterior tibial tendon is identified and released from its tendon sheath distal to the tip of the medial malleolus to its distal insertion at the navicular and retracted dorsally. Next, the flexor digitorum tendon is released from its sheath from the tip of the medial malleolus to the sustentaculum talus. Blunt dissection with a hemostat (tips against the deltoid ligament) continues under the fat-covered neuromuscular bundle and deep to the flexor hallucis tendon, exposing the deltoid ligament from the posteromedial corner of the subtalar joint to under the neck of the talus distally. The posterior tibialis tendon is retracted dorsally. A retractor is gently placed under the flexor digitorum, the neurovascular bundle and the flexor hallucis tendon to the posterior aspect of the subtalar joint. Ankle plantarflexion is utilized to remove tension from the tendons and the neurovascular bundle and increase exposure.
The exposed deltoid is divided from posterior to anterior in line with the skin incision. The plantar portion is sharply dissected from this line to the plantar medial aspect of the sustentaculum talus. The dorsal portion of the deltoid is sharply dissected from this line toward the tip of the medial malleolus. This dissection exposes the coalition from the posteromedial aspect of the subtalar joint to under the neck of the talus distally (please note these halves of the deltoid will be repaired after resection of the coalition).
Visibly, at this point, the coalition appears to be a “wall” of bone and/or fibrous tissue with no distinct landmarks. The plantar aspect of the sustentaculum talus is identified as are the posterior medial aspect of the subtalar joint and the inferior talar neck.
As evidenced in Fig. 1A, the length of the coalition from the posterior subtalar joint to under the neck of the talus is length “h.” The normal subtalar joint has two surfaces, the talar and the calcaneal. These are parallel to the inferior surface of the sustentaculum talus at distances of “x” and “y” as measured from the inferior aspect of the sustentaculum talus (Fig. 1B–D). The medial-to-lateral thickness of the coalition is measured as “z” (Fig. 1B–D). The TCC often tapers posteriorly and anteriorly (Fig. 1B). Multiple measurements should be made along the coalition to identify the tapering with respect to the inferior surface of the sustentaculum talus.
Using these guidance measurements (Fig. 1A–D), a 1-cm osteotome is used to make a cut into the coalition from medial to lateral to a depth of “z” at a distance “y” from the inferior aspect of the sustentaculum talus (Fig. 1B–D). The depth (“z”) can be determined by using a cleaned osteotome for each pass and measuring the amount of fat on the osteotome, similar to using a “dipstick” in measuring the oil level in a car.
A second, parallel cut using the osteotome, but at a distance of “x” (Fig. 1B–D) from the sustentaculum talus is made from posterior to under the talar neck at a medial to lateral depth of “z” (Fig. 1B–D). Please note that when the osteotome cuts through the lateral aspect of the coalition the sound of the tapping will dull. Curettes are then used to remove the TCC, often as one piece, completely exposing the normal articular surfaces of the talar and calcaneal aspects of the subtalar joint (see Fig. 1E and F, lines of the osteotomy). Local fat or bone wax is placed and interposed between the raw bone surfaces. No interposition is placed the where normal joint surfaces of the talus and calcaneus are opposing. A freer elevator can now easily pass from the posteromedial aspect of the subtalar joint to under the talar neck. The interosseous ligament is also now visible. Rotational motion of the subtalar joint, absent prior to excision of the coalition, is readily apparent confirming complete removal of the coalition.
Intraoperatively, the endpoint of successful excision of a talocalcaneal coalition should be: 1) the ability to pass a freer elevator from the posterior talocalcaneal joint to the interosseous talocalcaneal ligament (the entire length of the subtalar joint), then from the talocalcaneal ligament to below the talar neck, 2) Visualizing both sides of the subtalar joint throughout endpoint 1, and 3) the ability to wedge open the subtalar joint medially (valgus opening).
Results
Study criteria identified 27 patients with preoperative CT scans undergoing TCC ostectomy during the study period. Patients were predominantly male (59%) with a mean chronological age of 13.9 ± 2.4 years. Postoperative complications were rare, with two superficial incisional infections resolving with antibiotics and dressing changes and one asymptomatic incidental osteophyte. Demographic characteristics are further detailed in Table 1, while operative outcomes are detailed in Table 2.
Table 1.
Demographic characteristics.
| Variable | M ± SD or N (%) |
|---|---|
| Age (years) | 13.9 ± 2.4 |
| Sex | |
| Male | 16 (59) |
| Female | 11 (41) |
| Race | |
| White | 24 (89) |
| Black | 2 (7) |
| Other | 1 (4) |
| Ethnicity | |
| Hispanic | 2 (9) |
| Non-hispanic | 21 (91) |
Table 2.
Treatment outcomes and complications.
| M-CDS Complications | N (%) | Description |
|---|---|---|
| None | 24 (88) | |
|
Type 1 Deviation from normal course not requiring treatment |
1 (4) | Incidental osteophyte development |
|
Type 2 Deviation from normal course requiring outpatient treatment |
1 (4) | Superficial wound requiring antibiotics |
|
Type 3 Deviation from normal course requiring admission |
1 (4) | Superficial wound requiring incision and drainage |
TCCs were more commonly located on the left lower extremity (63%). The majority of TCCs (59%) were centralized along the medial third of the talocalcaneal joint line (Fig. 1A), while 41% also involved the posterior third. None were located along the anterior third.
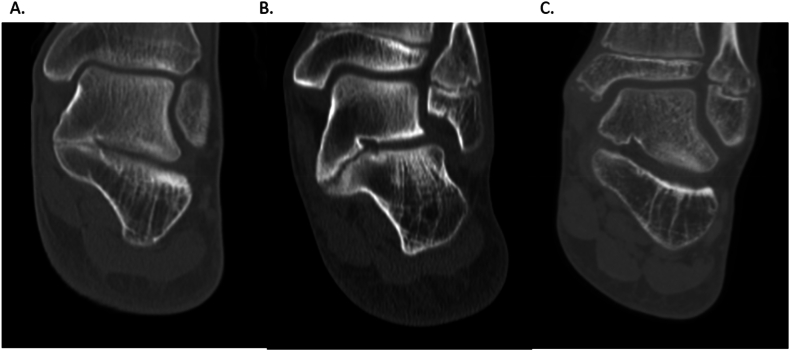
With fibrous connections, 59% of coalitions were horizontal, or parallel to the joint line (Fig. 2A). Thirty-seven percent of TCCs were medially down sloping or angulated inferiorly relative to the joint line (Fig. 2B), while 4% were medially upsloping relative to the joint line (Fig. 2C). For the sloping fibrous coalitions, bone was removed to the fibrous connection so that no small, ununited fragments were left behind at the time of surgery. It is uncertain what happens to the fibrous tissue with time following resection.
Figure 2.
A–C. The alignment of the TCC, while usually horizontal (A), may slope inferiorly relative to the joint line (B) or slope upward relative to the joint line (C). TCC, talocalcaneal coalitions.
The mean coalition length in the sagittal plane was 21.2 ± 6.0 mm, covering 49.6 ± 23.2% of the talar length. The mean coalition height and breadth in the coronal plane were 5.9 ± 0.8 mm and 13.7 ± 2.8 mm, respectively. Notably, neither the medial to lateral depth nor the distance proximal from the sustentaculum talus was uniform as the coalitions were thickest centrally and tapered both proximally and distally. Anatomic characteristics are further detailed in Table 3.
Table 3.
Overall coalition characteristics.
| Variable | N (%) |
|---|---|
| Sagittal location | |
| Anterior | 0 (0) |
| Middle | 16 (59) |
| Posterior | 11 (41) |
| Slope r/t joint line | |
| Horizontal | 16 (59) |
| Inferior | 10 (37) |
| Superior | 1 (4) |
| Laterality | |
| Right | 10 (37) |
| Left | 17 (63) |
| Sagittal length (mm) | 21.2 ± 6.0 |
| Percent talar length | 49.6 ± 23.2 |
| Coronal height (mm) | 5.9 ± 0.8 |
| Coronal width (mm) | 13.7 ± 2.8 |
Good agreement was achieved between three raters across measurements performed in this study. The mean two-way mixed average measures intraclass correlation coefficient was 0.781. Raters agreed the most on talar length measurements in the sagittal plane and agreed the least on TCC height in the coronal plane. Coalition measurements with two-way mixed intraclass correlation results are further detailed in Table 4., Table 5..
Table 4.
Stratified coalition characteristics with intraclass correlation results.
| Measurement (mm or %) | Rater 1 | Rater 2 | Rater 3 | ICC |
|---|---|---|---|---|
| Saggital TCC length | 21.5 ± 6.8 | 22.3 ± 7.3 | 23.3 ± 6.6 | 0.881 |
| Saggital talus length | 49.3 ± 5.3 | 47.5 ± 5.9 | 50.4 ± 5.5 | 0.955 |
| Saggital length ratio | 43.8 ± 13.9 | 46.8 ± 14.4 | 46.6 ± 13.8 | 0.897 |
| Coronal TCC height | 7.8 ± 2.4 | 7.8 ± 2.5 | 8.9 ± 2.3 | 0.477 |
| Coronal TC joint height | 15.2 ± 4.3 | 12.9 ± 3.0 | 14.1 ± 2.8 | 0.635 |
| Coronal TCC depth | 12.9 ± 3.2 | 13.1 ± 3.7 | 15.3 ± 3.6 | 0.838 |
TCC, talocalcaneal coalition; ICC, intraclass correlation.
Table 5.
Intrarater reliability results.
| Measurement (mm or %) | Rater 1 | Rater 2 | Rater 3 |
|---|---|---|---|
| Saggital TCC length | 0.537 | 0.865 | 0.854 |
| Saggital talus length | 0.903 | 0.883 | 0.948 |
| Saggital length ratio | 0.453 | 0.873 | 0.705 |
| Coronal TCC height | 0.869 | 0.776 | 0.510 |
| Coronal TC joint height | 0.666 | 0.789 | 0.888 |
| Coronal TCC depth | 0.900 | 0.927 | 0.943 |
TCC, talocalcaneal coalition.
Discussion
To date, very little in the way of intraoperative planning for TCCs has been proposed in the literature, even though advanced imaging has been widely used preoperatively. Alternative approaches, such as intraoperative CT, expose the patient to increased radiation and anesthesia, potentially incurring higher financial and time costs. By using the sustentaculum talus as an orienting landmark and measuring the coalition on preoperative CT scans, surgeons can approach TCC excision more accurately and with less damage to normal structures.
This study is not meant to represent the overall incidence and presentation of TCC in the general population, but rather what was seen in this consecutive, limited series. Understanding the location, orientation, and size of talocalcaneal coalitions is useful for any surgeon. Previous classification systems have described location and orientation, with 40–70% parallel to and 70–90% involving the middle one-third of the joint line [5,8,9]. With respect to location, this study suggests the majority of coalitions may be found along the posterior two-thirds of the talocalcaneal joint, most often the medial one-third, in agreement with the literature. With respect to orientation, this study suggests the majority of coalitions appear oriented parallel to the joint line; when a slope occurs, it tends to be oriented anteromedially, which is consistent with literature. With respect to size, less has been reported. The results of this study show TCCs tended to be over twice as deep as they were tall, and almost twice as long as they were deep. Of note, these measurements were not uniform—reinforcing the notion that a systematic method for mapping coalitions may be beneficial for successful surgical excision of TCCs.
Limitations of this study include the availability of advanced imaging, as not every patient with a talocalcaneal coalition will undergo CT or magnetic resonance imaging. Further, the quality of the advanced imaging can affect the accuracy of the planning, as slice thickness and clarity with respect to patient adherence to remaining still during image acquisition may influence the ability to measure coalition dimensions. Similarly, our small sample size is underpowered to show true epidemiological differences in coalition presentation and characteristics, such as laterality. Moreover, the margin of error between raters when selecting slices to measure on, as well as initiation, termination, and orientation of imaging lines was shown to be low but present. While only fair agreement was achieved between raters on the least agreed-upon measure, the mean difference between raters was just over 1 mm, which should not significantly alter the usefulness of this technique. Lastly, reproducing the imaging measurements intraoperatively, even with an orienting landmark, requires spatial orientation as well as accurate osteotome depth measurements, both of which have the potential to introduce error.
This investigation describes a concise, readily applicable, and systematic method to map talocalcaneal coalitions to facilitate better intraoperative guidance for surgical excision using readily identifiable anatomic landmarks. The cumulative expense and radiation exposure from intraoperative CT are not required as part of this system. This study also characterizes the size, shape, location, and orientation of tarsal coalitions in studied patients, adding to the current body of literature.
Consent for publication
The author(s) declare that no patient consent was necessary as no images or identifying information are included in the article.
Author contributions
Nathan Chaclas: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization. Carter E. Hall: Writing – review & editing, Writing – original draft, Methodology, Data curation. Bernard D. Horn: Writing – review & editing, Supervision, Conceptualization. Richard S. Davidson: Writing – review & editing, Writing – original draft, Visualization, Supervision, Conceptualization.
Funding
This research study received no direct funding.
Declaration of competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Docquier P.L., Maldaque P., Bouchard M. Tarsal coalition in paediatric patients. Orthop Traumatol Surg Res. 2019;105(1S):S123–S131. doi: 10.1016/j.otsr.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 2.Murphy J.S., Mubarak S.J. Talocalcaneal coalitions. Foot Ankle Clin. 2015;20(4):681–691. doi: 10.1016/j.fcl.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Bonasia D.E., Phisitkul P., Saltzman C.L., Barg A., Amendola A. Arthroscopic resection of talocalcaneal coalitions. Arthrosc J Arthrosc Relat Surg. 2011;27(3):430–435. doi: 10.1016/j.arthro.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 4.Knörr J., Soldado F., Menendez M.E., Domenech P., Sanchez M., Sales de Gauzy J. Arthroscopic talocalcaneal coalition resection in children. Arthroscopy. 2015;31(12):2417–2423. doi: 10.1016/j.arthro.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Rozansky A., Varley E., Moor M., Wenger D.R., Mubarak S.J. A radiologic classification of talocalcaneal coalitions based on 3D reconstruction. J Child Orthop. 2010;4(2):129–135. doi: 10.1007/s11832-009-0224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ellsworth B.K., Kehoe C., Defrancesco C.J., Bogner E., Mintz D.N., Scher D.M. Talocalcaneal tarsal coalition size: evaluation and reproducibility of MRI measurements. J Pediatr Orthop. 2022;42(6):E612–E615. doi: 10.1097/BPO.0000000000002129. [DOI] [PubMed] [Google Scholar]
- 7.Mosca V.S., Bevan W.P. Talocalcaneal tarsal coalitions and the calcaneal lengthening osteotomy: the role of deformity correction. J Bone Joint Surg Am. 2012;94(17):1584–1594. doi: 10.2106/JBJS.K.00926. [DOI] [PubMed] [Google Scholar]
- 8.Wang A., Shi W., Gao L., et al. A new classification of talocalcaneal coalitions based on computed tomography for operative planning. BMC Muscoskelet Disord. 2021;22(1):678. doi: 10.1186/s12891-021-04567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim S., Lee H.K., Bae S., Rim N.J., Cho J. A radiological classification system for talocalcaneal coalition based on a multi-planar imaging study using CT and MRI. Insights Imaging. 2013;4(5):563–567. doi: 10.1007/s13244-013-0267-3. [DOI] [PMC free article] [PubMed] [Google Scholar]