Abstract
Objectives
To assess the prevalence of enamel hypomineralisation (EH), molar-incisor hypomineralisation (MIH), and hypomineralisation affecting the first permanent molars and incisors (M + IH). It was hypothesized that MIH prevalence had not changed significantly over the last two decades.
Methods
Published literature was screened via PubMed, Embase, Google Scholar, and an extensive hand search. A risk of bias assessment (RoB) was conducted. Prevalence estimates were synthesised in a random-effects meta-analysis and reported at the country-level, continent-level, and globally. Subgroup analyses between different MIH diagnosis indices were conducted. Global MIH prevalence trends between 2000 and 2020 were analysed at 5-year intervals.
Results
Among the 746 retrieved references, 174 were eligible. However, 138 low-to-moderate RoB studies were included. EH global prevalence was estimated at 25.3% (20.0–30.6) across 21 studies from 15 countries. MIH prevalence was 15.5% (14.4–16.6) across 135 studies from 53 countries, with estimates ranging from 0.6 to 46.6%. Among these studies, 60 reported M + IH prevalence, estimated at 6.9% (6.0–7.7). The global MIH prevalence as analysed in 5-year intervals showed a relatively constant prevalence rate with no significant differences across the years. Similarly, MIH prevalence did not differ significantly based on the diagnostic index used.
Conclusion
EH phenotypes remain globally widespread with uneven distributions. Data doesn’t support the postulated change in MIH prevalence. Assessments of all EH phenotypes and data from underrepresented countries are needed for effective dental health monitoring.
Clinical relevance
Oral health professionals should systematically and routinely screen for EH/MIH and discuss it with patients, particularly in high prevalence populations.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00784-025-06411-4.
Keywords: Epidemiology, Dental enamel, Diagnostic techniques, Oral health, Cross-sectional studies, Health surveys
Introduction
Enamel hypomineralisation (EH) encompasses various qualitative defects in enamel mineralisation [1]. The demarcated opacities characteristic of EH often present as well-defined asymmetrically distributed lesions with distinct boundaries from the adjacent normal enamel, in contrast to the diffuse, symmetrical appearance of fluorosis lesions which typically follow a chronological distribution pattern. A prevalent form of EH is molar-incisor hypomineralisation (MIH) which manifests either as demarcated opacities, enamel breakdown, atypical restorations, and/or extractions. An MIH diagnosis is established when at least one first permanent molar is affected, with or without the involvement of the incisors [1–3]. In some cases, MIH affects both the permanent molars and incisors simultaneously, leading to an extensive form of the disease that is referred to as M + IH [4]. Beyond the aforementioned ‘index teeth’, EH can principally occur in any other primary or permanent tooth. Consequently, another viable epidemiological measure is the number of individuals with at least one tooth showing EH, regardless of its distribution. As a result, the prevalence of EH is inherently greater than that of MIH or M + IH [4, 5].
One of the earliest systematic reviews on the global prevalence of MIH estimated that it ranges from 2.4 to 40.2% [6]. These findings were later corroborated by a review reporting global prevalences in the same range [7]. Recent meta-analyses have refined these calculations yielding close-ranging prevalence estimates ranging from 12.8% (11.5–14.1) to 14.2% (12.6–15.8) [7–12]. Over the past two decades, the number of cross-sectional studies examining the prevalence of EH, MIH, and M + IH has increased noticeably [13], raising speculation about a potential global rise in MIH prevalence [11, 13, 14]. It remains unclear whether the surge in MIH research has influenced prevalence estimates or whether the global prevalence may have actually changed over time. Additionally, inconsistencies may arise from the use of various diagnostic indices, since several indices are widely available and employed.
Existing reviews often summarize data at the continental or broader regional levels [7–9, 11], frequently overlooking insightful country-specific details. Moreover, the quality of the studies included was frequently not appraised [6–8]. Furthermore, meta-analyses reporting on the prevalence of other phenotypes such as EH or M + IH are lacking in the literature. These knowledge gaps highlight the need for an updated, critical evaluation. Therefore, this systematic review and meta-analysis aimed to: (1) provide a comprehensive update on the global status of EH, MIH, and M + IH with emphasis on study quality assessment, detailed reporting of continent- and country-specific estimates, and various diagnostic indices; and (2) explore the epidemiological trends in global MIH prevalence in cross-sectional studies. The null hypothesis was that there would be no significant difference in the global MIH prevalence over the last two decades.
Materials and methods
This systematic review was reported according to the PRISMA guidelines [15] and aimed to answer the following research question: “What is the global prevalence of children and young adults affected by EH, MIH, and M + IH?”. This review’s protocol was registered (10.17605/OSF.IO/YEXCQ).
Literature search
The PubMed, Embase, and Google Scholar databases were searched with no restrictions using relevant keywords for studies published until the end of June 2024. The search queries and results can be found in Appendix I in the supplementary materials. Additionally, an extensive hand search was conducted by reviewing reference lists of included studies, previously published reviews, and journals of interest. Any reviews retrieved through the search were screened for references to additional eligible studies. Articles identified through the hand search were added to the database results All records were exported to the Rayyan platform for the removal of duplicates and screening [16]. Owing to the inconsistent MIH diagnosis criteria in studies published before 2000 and given that they had already been summarized in a systematic review by Jälevik in 2010 [6], these studies were excluded from the review. Thus, this systematic review included studies published from 2000 to June 2024.
Study screening and eligibility criteria
After removing duplicate references, two independent reviewers screened the titles and abstracts of all identified references. The reviewers evaluated the references for eligibility based on the predefined inclusion and exclusion criteria. Eligible studies were those that reported on the prevalence of EH, MIH, and/or M + IH in the permanent dentition. Only cross-sectional and population-based studies that recruited a representative sample were included. In contrast, studies which recruited participants from a convenience sample, or targeted highly specific nonrepresentative populations were excluded. Studies which exclusively reported on other hypomineralisation phenotypes, including deciduous molar hypomineralisation, hypomineralisation on second primary molars, or rare dental diseases were excluded. Studies that did not mention the index used for diagnosis were not considered. Reviews and conference proceedings were also excluded. If a study’s eligibility could not be determined from the abstract, the full text was obtained. The full texts of the eligible publications were retrieved and assessed according to the inclusion criteria.
Furthermore, to avoid duplicate representation and prevent artificially inflated results, all eligible studies were thoroughly examined for redundant reporting. If multiple publications originated from the same study project, the version with the most comprehensive epidemiological data was included. The reviewers were not blinded to the authors, institutions, or publishing journals of the studies under consideration. Any disagreements were resolved in the work group and all studies were included in consensus.
Risk of bias assessment
A critical appraisal and risk of bias assessment (RoB) were conducted by two reviewers independently. The RoB assessment followed the recommended Critical Appraisal Tool for prevalence studies from the Joanna Briggs Institute (JBI) [17, 18]. This tool allows comprehensive appraisal of the methodological quality of studies reporting prevalence using nine signalling questions that cover study design, conduct, and data analysis (Appendix II). Each question could be answered as yes, no, unclear, or not applicable. In detail, the questions assessed the sampling frame, participant recruitment, sample size calculations, description of the study participants and setting, coverage of the sample, target condition identification/diagnosis methods, use of the identification methods, data analysis, and response rates. An overall appraisal and a recommendation (include, exclude, or seek further information) were given to each study. Studies that showed high RoB in core appraisal items which included failing to use a reliable/standardized MIH diagnosis method, recruiting participants from a convenience sample, or targeting highly specified nonrepresentative populations were excluded (Appendix III). Recognized MIH indices included the European Academy of Paediatric Dentistry (EAPD) index, Developmental Dental Defects of Enamel (DDE) index, Ghanim et al., and other indices that align with that of the EAPD: including the criteria by Cho et al., Wetzel and Reckel, Molar-Incisor Hypomineralisation Severity Scoring System (MIH-SSS), Mathu-Muju and Wright criteria, Kemoli 2008, Cabral 2017, Alaluusua et al., MIH treatment need index (MIH-TNI), and Koch et al. All included studies underwent the RoB assessment. Any study for which the full text was inaccessible was excluded from further analysis.
Data extraction
Only studies that met the inclusion criteria and showed low or moderate RoB were considered for further analysis. Two reviewers independently extracted the data from the included studies in a structured extraction form in Excel (Excel 2019, Microsoft, Redmond, WA, USA). If necessary, the study authors were contacted for clarification or missing information. In brief, the following data were extracted: bibliographic information, country, continent, examination year, sample size, sample age, study setting, diagnostic index used for scoring, and prevalence results for EH, MIH, and M + IH. The forms were cross-checked between the reviewers, and any disagreements or inconsistent findings were resolved by discussion with the principal investigator.
Statistical analysis
A systematic approach to the statistical analysis was adopted. Three independent random effects meta-analyses of prevalence for EH, MIH, and M + IH were conducted, and forest plots were created. Owing to the large number of cross-sectional studies, prevalence data were aggregated in subgroup analyses at the country, continent, and global level, respectively. The global prevalence of the different hypomineralisation phenotypes by country was depicted using a heatmap, and the temporal distribution of studies was presented in a scatterplot. Furthermore, a subgroup analysis comparing the MIH prevalence rates reported in studies using the EAPD index [3], the DDE index [19], or other scoring indices was performed.
To investigate trends in MIH prevalence over time, a three-pronged strategy was developed. The included studies were structured into three categories on the basis of publication year, reported examination year, and estimated examination year. Since the exploratory data analysis revealed that only 65 (47.1%) of the studies reported the actual examination year, an estimation was necessary to avoid excluding the majority of the dataset from this analysis. The examination year was estimated based on an average time lag of 3 years between study conduct and publication, as calculated from studies that reported their examination year. Therefore, for studies lacking these data, the estimated examination year was assumed to be 3 years prior to the publication year. For each of the three categories, a random-effects meta-analysis was conducted with subgroups based on four 5-years intervals. Each interval’s meta-analytic MIH prevalence estimate, along with its 95% confidence interval (95% CI), was reported. The p-values for each meta-analysis were also provided. A line graph featuring the meta-analytic estimates for the time intervals across categories was created to illustrate the trends and fluctuations. Sensitivity analyses were conducted. Analyses and illustrations were done using Stata (StataCorp. 2019, release 16, College Station, TX: StataCorp LLC, USA) along with the statistical package metaprop [20].
Results
The literature search yielded 746 records to be screened. After examination of the titles and abstracts 539 did not meet the inclusion criteria. Upon reading the full texts of eligible studies another 33 studies were excluded: 27 articles were found to report on the same study population as another eligible article, four studies were published before 2000 and two articles could not be accessed. At this selection stage 174 cross-sectional epidemiological studies were identified (Fig. 1). In addition, the RoB assessment revealed that 36 (20.7%) studies showed high RoB and were thus excluded. The reasons for study exclusion are summarized in Appendix III. Finally, 138 studies were considered for data extraction and meta-analysis [21–157]. Appendix IV summarizes the data extracted from the included studies.
Fig. 1.
Flowchart of the study selection process.
The majority of studies examined children or adolescents with mixed dentition, where participants’ age ranged from 3 to 18 years old. The sample size ranged from 77 to 32,142. MIH prevalence varied widely across the included studies, with estimates as low as 0.6% in Poland [158] and up to 46.6% in Brazil [22] (Fig. 2). Asia (N = 44) and Europe (N = 45) were the two continents with the highest number of publications (Table 1). All 138 studies were included in the meta-analyses, aggregating the data from a total of 199,662 participants. In summary, 21 studies from 15 countries reported on the prevalence of EH. While 135 studies from 53 countries reported on MIH prevalence, only 60 studies (across 33 countries) reported the M + IH prevalence concomitantly (Fig. 1).
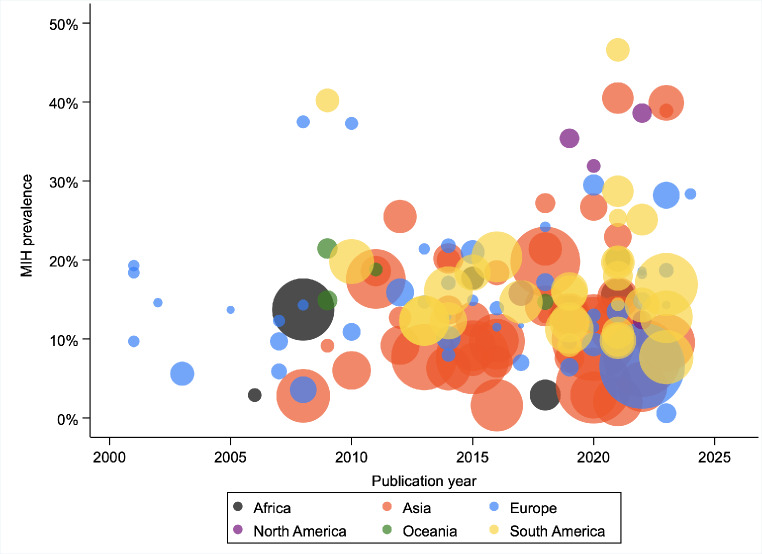
Fig. 2.
Scatterplot of the temporal spread of publications with reported MIH prevalence as categorized by continent. The size of the circles corresponds to the sample size.
Table 1.
Meta-analysis results for the prevalence of EH, MIH, and M + IH in included studies per country, continent, and globally. The number of studies reporting on MIH prevalence is indicated for each country and continent next to its name
| Continent | Country | EH prevalence | MIH prevalence | M + IH prevalence |
|---|---|---|---|---|
|
Europe (N = 45) |
Switzerland (N = 2) | 0.075 (0.072–0.078) | 0.077 (0.074–0.079) | |
| Netherlands (N = 2) | 0.114 (0.094–0.135) | 0.030 (0.018–0.049) | ||
| Bulgaria (N = 1) | 0.036 (0.030–0.043) | |||
| Norway (N = 2) | 0.238 (0.225–0.251) | 0.058 (0.044–0.076) | ||
| United Kingdom (N = 2) | 0.165 (0.152–0.177) | |||
| Germany (N = 6) | 0.276 (0.021–0.532) | 0.111 (0.075–0.147) | 0.050 (0.027–0.074) | |
| Lithuania (N = 1) | 0.144 (0.126–0.164) | 0.094 (0.080–0.111) | 0.021 (0.015–0.031) | |
| Austria (N = 2) | 0.087 (0.076–0.098) | 0.035 (0.027–0.042) | ||
| Sweden (N = 1) | 0.333 (0.294–0.375) | 0.184 (0.153–0.220) | 0.087 (0.066–0.115) | |
| Romania (N = 1) | 0.143 (0.106–0.190) | |||
| Italy (N = 2) | 0.269 (0.215–0.330) | 0.161 (0.131–0.192) | 0.057 (0.038–0.076) | |
| France (N = 1) | 0.187 (0.162–0.214) | |||
| Spain (N = 4) | 0.459 (0.433–0.485) | 0.205 (0.105–0.306) | 0.141 (0.122–0.160) | |
| Poland (N = 4) | 0.131 (0.117–0.145) | 0.077 (0.021–0.133) | 0.040 (0.032–0.049) | |
| Slovenia (N = 1) | 0.220 (0.185–0.259) | 0.104 (0.080–0.135) | ||
| Bosnia and Herzegovina (N = 4) | 0.291 (0.257–0.324) | 0.120 (0.102–0.138) | 0.086 (0.056–0.116) | |
| Greece (N = 1) | 0.213 (0.197–0.230) | 0.114 (0.102–0.128) | ||
| Croatia (N = 1) | 0.130 (0.108–0.157) | 0.066 (0.050–0.086) | ||
| Belgium (N = 1) | 0.217 (0.174–0.268) | 0.186 (0.146–0.235) | ||
| Denmark (N = 3) | 0.345 (0.287–0.403) | 0.097 (0.077–0.122) | ||
| Finland (N = 3) | 0.161 (0.119–0.202) | 0.063 (0.040–0.097) | ||
| Europe estimate | 0.246 (0.184–0.309) | 0.154 (0.134–0.174) | 0.071 (0.057–0.085) | |
|
Asia (N = 44) |
United Arab Emirates (N = 3) | 0.243 (0.057–0.429) | 0.094 (0.067–0.129) | |
| Iran (N = 3) | 0.530 (0.490–0.569) | 0.172 (0.127–0.217) | ||
| Syria (N = 1) | 0.397 (0.369–0.426) | |||
| Saudi Arabia (N = 2) | 0.212 (0.196–0.227) | 0.121 (0.106–0.138) | ||
| Lebanon (N = 2) | 0.264 (0.240–0.288) | 0.169 (0.150–0.189) | ||
| India (N = 19) | 0.213 (0.201–0.225) | 0.081 (0.065–0.098) | 0.038 (0.024–0.052) | |
| Turkey (N = 3) | 0.104 (0.054–0.154) | 0.059 (0.031–0.108) | ||
| Singapore (N = 1) | 0.125 (0.106–0.146) | 0.028 (0.020–0.040) | ||
| South Korea (N = 1) | 0.060 (0.049–0.074) | |||
| Thailand (N = 1) | 0.196 (0.163–0.234) | 0.019 (0.010–0.035) | ||
| Japan (N = 1) | 0.198 (0.187–0.210) | |||
| Iraq (N = 1) | 0.186 (0.161–0.214) | 0.090 (0.072–0.111) | ||
| Nepal (N = 1) | 0.137 (0.114–0.163) | 0.116 (0.095–0.141) | ||
| China (N = 3) | 0.116 (0.044–0.189) | 0.021 (0.018–0.024) | ||
| Jordan (N = 2) | 0.160 (0.150–0.171) | 0.060 (0.053–0.069) | ||
| Asia estimate | 0.326 (0.138–0.514) | 0.137 (0.119–0.155) | 0.061 (0.049–0.073) | |
|
South America (N = 29) |
Peru (N = 1) | 0.198 (0.162–0.240) | ||
| Brazil (N = 19) | 0.178 (0.150–0.207) | 0.077 (0.040–0.115) | ||
| Argentina (N = 1*) | 0.161 (0.140–0.184) | |||
| Uruguay (N = 1*) | 0.123 (0.100–0.151) | |||
| Ecuador (N = 1) | 0.092 (0.062–0.135) | |||
| Chile (N = 2) | 0.136 (0.121–0.152) | |||
| Colombia (N = 3) | 0.169 (0.068–0.270) | |||
| Venezuela (N = 1) | 0.254 (0.189–0.331) | |||
| South America estimate | 0.171 (0.151–0.192) | 0.077 (0.040–0.115) | ||
|
North America (N = 6) |
United States of America (N = 1) | 0.096 (0.070–0.130) | 0.051 (0.033–0.078) | |
| Mexico (N = 5) | 0.268 (0.161–0.374) | |||
| North America estimate | 0.239 (0.144–0.334) | 0.051 (0.033–0.078) | ||
|
Africa (N = 7) |
Sudan (N = 1) | 0.201 (0.170–0.236) | 0.125 (0.100–0.155) | |
| Kenya (N = 1) | 0.137 (0.126–0.149) | 0.092 (0.083–0.102) | ||
| Nigeria (N = 2) | 0.076 (0.060–0.096) | 0.044 (0.033–0.054) | 0.098 (0.074–0.128) | |
| Libya (N = 2) | 0.091 (0.055–0.147) | 0.136 (0.117–0.155) | 0.076 (0.062–0.094) | |
| Egypt (N = 1) | 0.131 (0.114–0.150) | |||
| Africa estimate | 0.078 (0.061–0.095) | 0.128 (0.079–0.177) | 0.095 (0.079–0.111) | |
|
Oceania (N = 4) |
Australia (N = 2) | 0.428 (0.397–0.460) | 0.184 (0.159–0.210) | |
| New Zealand (N = 2) | 0.153 (0.125–0.186) | 0.160 (0.134–0.186) | 0.037 (0.023–0.050) | |
| Oceania estimate | 0.323 (0.081–0.565) | 0.174 (0.139–0.208) | 0.037 (0.023–0.050) | |
| Global estimate | 0.253 (0.200–0.306) | 0.155 (0.144–0.166) | 0.069 (0.060–0.077) | |
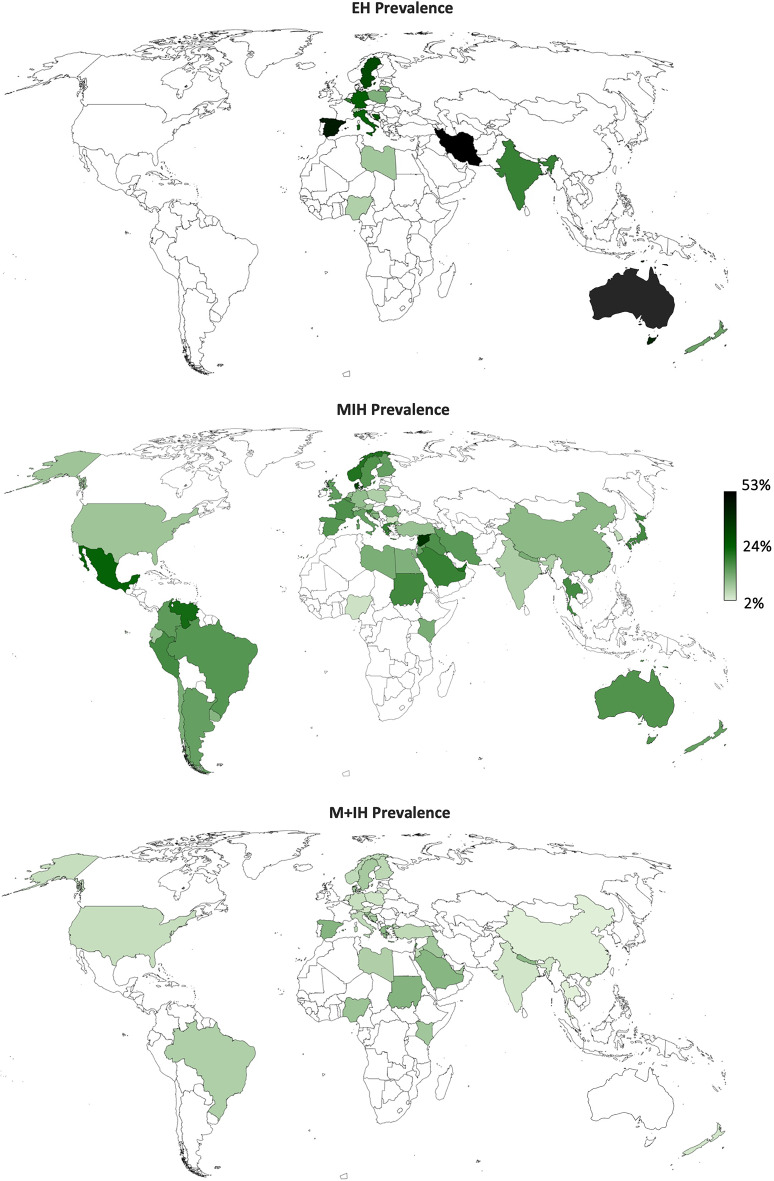
*Results for these countries were reported in a single study but were treated as distinct datasets in the meta-analysis
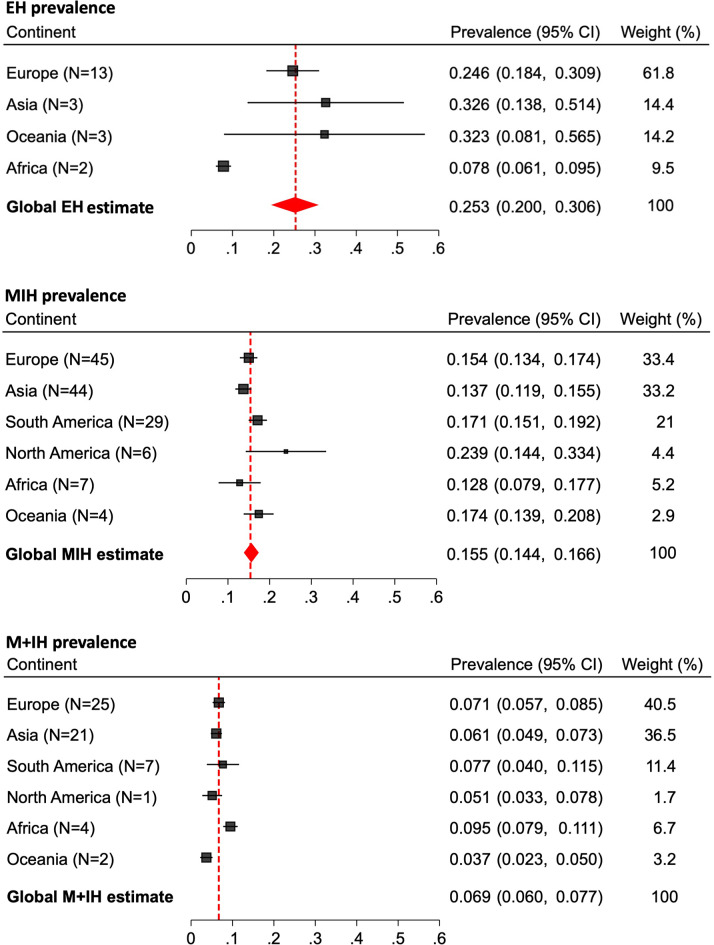
Pooled meta-analysis results for EH, MIH, and M + IH at the country- and continent-levels can be found in Table 1; Fig. 3; the world map (Fig. 4) further facilitates comparison between countries. The pooled global prevalence of EH, MIH, and M + IH were estimated at 25.3% (20.0–30.6), 15.5% (14.4–16.6), and 6.9% (6.0–7.7), respectively. Subgroup analysis by continent (Fig. 3) revealed that Africa had the lowest MIH prevalence at an estimated 12.8% (7.9–17.7), whereas North America had the highest prevalence at 23.9% (14.44–33.4).
Fig. 3.
Forest plots for the subgroup analyses of EH, MIH, and M + IH prevalence per continent.
Fig. 4.
World map showing the estimated prevalence of EH (15 countries), MIH (53 countries), and M + IH (33 countries) per country.
The EAPD criteria were the most frequently used MIH diagnostic index (N = 99 studies) followed by the DDE (N = 12). The remaining studies (N = 24) utilized various other indices, with some incorporating multiple indices in their diagnostic process. These included: Ghanim et al. (N = 12), Cho et al. (N = 2), Wetzel and Reckel (N = 2), Molar-Incisor Hypomineralisation Severity Scoring System (MIH-SSS) (N = 2), Mathu-Muju and Wright criteria (N = 1), Kemoli 2008 (N = 1), Cabral 2017 (N = 1), Alaluusua et al. (N = 1), MIH treatment need index (MIH-TNI) (N = 1), and Koch et al. (N = 1). The subgroup comparison between studies using the EAPD, DDE, or other scoring indices revealed no significant differences in the MIH prevalence among studies (15.9% (14.4–17.3), 16.2% (12.7–19.7), and 14.4% (12.1–16.6), respectively; p = 0.496).
The examination of the epidemiological trends over the past two decades revealed harmonious trends across the three scenarios (Table 2). When categorized according to year of publication, the prevalence of MIH showed non-significant variation, starting at 15.1% in 2000–2005 and ending at 13.7% in 2016–2020. Similarly, when the reported year of examination was considered, the prevalence initially declined from 19.2% in 2000–2005 to 14.1% in 2011–2015, before increasing to 17.8%. Finally, for studies grouped by the estimated year of examination, the MIH prevalence fluctuated the least, with values ranging from 15.7 to 16.1% (Table 2). These meta-analytic findings showed that while there are minor differences in prevalence over time, there has been no significant shift over the past two decades (p ≥ 0.05), as presented in Fig. 5. Sensitivity and subgroup analyses (grouping by country, continent, hypomineralisation phenotype, diagnosis index, and time intervals) were performed and confirmed the robustness of the present findings.
Table 2.
Meta-analysis results for the prevalence of MIH globally in 5-year intervals. The number of studies used to calculate each estimate is indicated in brackets
| Global MIH prevalence according to |
2000–2005 | 2006–2010 | 2011–2015 | 2016–2020 | p-value |
|---|---|---|---|---|---|
| \Year of publication (N = 92) |
15.1% (8.8–21.3) N = 6 |
15.3% (11.9–18.7) N = 17 |
14.7% (12.9–16.5) N = 31 |
13.7% (11.6–15.7) N = 38 |
0.809 |
| Reported year of examination (N = 65) |
19.2% (10.6–27.9) N = 6 |
16.6% (12.6–20.5) N = 17 |
14.1% (12.1–16.2) N = 16 |
17.8% (14.3–21.2) N = 26 |
0.221 |
| Estimated year of examination (N = 127) |
15.7% (10.0–21.5) N = 9 |
15.3% (12.6–18.1) N = 26 |
13.6% (11.7–15.4) N = 41 |
16.1% (14.3–17.8) N = 51 |
0.284 |
MIH prevalence was not calculated for studies before 2000 due to the low number of studies and inconsistent diagnosis criteria. Similarly, calculations were not performed for studies after 2020 because many clinical trials were cancelled or postponed in 20212023 due to the COVID-19 pandemic. Additionally, this interval did not meet the required 5-year observation period making it incomparable to earlier intervals
Fig. 5.
Epidemiological trends of the meta-analytic estimates for MIH prevalence in 5-year intervals as categorized by the publication, estimated examination, and reported examination year. The plotted circles reflect the fluctuations in prevalence estimates and associated 95% confidence intervals for each interval within the three categories. The 95% CI are shown with corresponding coloured error bars. The size of the circles is proportional to the number of studies in this interval. The dashed horizontal reference line and the surrounding grey area represent the estimated MIH global prevalence of 15.5% and the 95% CI (14.4–16.6) as calculated from all included studies.
Discussion
The expanding body of literature investigating the aetiology, prevalence, and management of EH/MIH in recent decades underscores the growing interest within the dental community [13]. To address the expanding body of literature, this systematic review and meta-analysis critically appraised and synthesized the global evidence on the prevalence of EH, MIH and M + IH, along with detailed reporting of continent- and country-specific data and a comparison of different diagnostic indices. Importantly, the present study explored the epidemiological trends in MIH prevalence over the past two decades, where no significant differences have been found. Thus, the present study’s hypothesis was accepted.
This key finding of the meta-analysis is the notable stability of MIH prevalence over time, contrary to prior speculations of an increasing prevalence [11, 13, 14] (Fig. 5). The random effects sub-group meta-analysis by time intervals exhibited statistically insignificant fluctuations, a trend that was consistent across estimates according to the publication year, estimated examination year, and reported examination year (Table 2). In particular, when it was calculated based on the estimated examination year, the MIH prevalence remained consistently aligned with the global prevalence (Fig. 5). These findings are in line with a recent investigation by Sluka et al. [11], who also reported no evidence of a global increase in prevalence. In contrast to the present study, Sluka et al. approached the data by grouping studies in three birth cohorts based on the ages of the study participants. They reported estimates ranging from 9 to 18% across the cohorts, with no significant differences between the subgroups. However, in one sub-group analysis of 11 studies, they observed a two-fold increase in prevalence between 2000 and 2010. Owing to the complexity of their data, Sluka et al. stated that a meta-analysis was not feasible, and prospective studies are needed to confirm these findings. Despite the different analytical approaches, the epidemiological trends documented in both the present analysis and Sluka et al.’s were consistent [11]. Based on the available cross-sectional MIH data, it can be concluded that there was no increase in the global prevalence thus far. Nevertheless, to truly confirm any changes in MIH or EH prevalence over time, prospectively designed cross-sectional studies that are repeated at standardized time intervals with highly matched cohorts are essential to ascertain such a possibility and enable dental health monitoring.
In addition to investigating epidemiologic trends, this meta-analysis synthesized the global prevalence of three prevalent hypomineralisation phenotypes (Table 2; Fig. 5). The global MIH prevalence was estimated at 15.5% (14.4–16.5). When interpreting the present data in light of the CIs and comparing them to estimates from previous systematic reviews, a consistent trend emerges: the results of the present study and prior estimates closely overlap within the same CI range. In detail, previous meta-analytic estimates include 14.2% (12.6–15.8) [8], 13.5% (12.0–15.1) [10], 13.1% (11.8–14.5) [12], 12.9% (11.7–14.3) [9], and 12.8% (11.5–14.1) [11]. This overlap in CIs reinforces the current findings. It is further supported by the data from Fig. 5, which illustrates that nearly all prevalence estimates lie within or very near the estimated 95% CI (horizontal gray bar). This global estimate is further strengthened by the inclusion of a large number of studies with acceptable RoB compared to previous analyses, as well as the conduction of multiple subgroup analyses, making it a potentially robust estimate.
Consistent with previous reviews reporting MIH prevalence [8, 11, 12], there are significant differences across continents (Fig. 3) alongside considerable variation in prevalence reported across countries (Fig. 4). This review supports previous findings in that North America has the highest MIH prevalence (23.9%) [10, 12], followed by South America (17.1%) (Fig. 3). Similarly, Zhao et al. [8] estimated the prevalence in South America at 18.0%, whereas Lopes et al. [10] reported a combined prevalence for the Americas based on 30 studies at 15.3%. For Africa, this review documented the lowest MIH prevalence at 12.8%, which is comparable to previous estimates of 10.9% and 14.5% [8, 10]. As consistently observed in earlier reviews Europe had the highest number of studies on MIH prevalence, with the present estimate at 15.4%, closely aligning with previous estimates of 14.3% and 14.4% [8, 10]. However, the unequal number of studies across continents calls for cautious interpretation of summary statistics, especially in regions with limited data and high prevalence estimates such as North America and Oceania (Table 1).
While previous reviews have focused predominantly on continent- or superregional-level data, this review uniquely presents country-level meta-analyses for the three hypomineralisation phenotypes (Table 1), which had not been previously calculated in this manner. Notably, Zhao et al. [8] had previously reported the meta-analytic MIH estimates for six countries only. These findings are highly consistent with the present findings, with both reviews’ estimates falling within ± 1%. With data from 53 countries, the present review offers a valuable reference point for assessing prevalence changes at the country level. In contrast, the most comprehensive prior reviews included data from 43 to 49 countries [8, 12].
Part of the novelty of this systematic review and meta-analysis lies in synthesizing the global prevalence of EH and M + IH in a meta-analysis and reporting these findings at the continent- and country-levels (Table 1; Fig. 3). The EH prevalence was estimated at 25.3% (20.0–30.6), with the greatest prevalence reported in Oceania (32.3%). The present search did not yield any studies on the prevalence of EH in the North or South American continents, although these continents showed the highest MIH prevalence globally. Consistent with their high MIH prevalence, the highest EH prevalence was reported in Spain (45.9%) and Iran (53.0%). The global M + IH prevalence was estimated at 6.9% (6.0–7.7). Despite having the lowest MIH prevalence, Africa had the highest prevalence of M + IH at 9.5%. Similar to the data on EH, we found only one study reporting on the prevalence of M + IH in each of North America, South America, and Oceania, which limits the generalizability of the estimates for these continents. Consequently, owing to the lack of comparable studies synthesizing the global estimates of EH or M + IH, comparison with other studies was not possible. However, data from a previous review allow for an inferred estimate of M + IH prevalence at 5.7%, which was calculated based on 36 studies [10], in contrast to the 60 studies accounted for in the present review’s estimate. By synthesizing this data, the review not only bridges a significant gap in the literature but also establishes a reference value for the EH and M + IH phenotypes.
This review analysed 138 cross-sectional studies published after 2000. As has been the case in previous MIH reviews [10–12], studies conducted before 2000 were excluded mainly because of inconsistencies in diagnostic criteria prior to the formal adoption of the EAPD index guidelines in 2003 [3]. The qualitative assessment revealed that 20.7% of the eligible studies had high RoB, which is highly similar to the results of Sluka et al. [11] who reported that 18.6% of the studies were of low quality. An examination into the body of data, as illustrated by the scatterplot in Fig. 2, reveals several key insights. Firstly, it clearly illustrates the increase in the number and size of MIH epidemiological studies over time as confirmed by a recent bibliometric analysis [13]. Moreover, studies with a larger sample size tended to report lower MIH estimates. Furthermore, studies from Asia tend to have larger sample sizes on average. Although Europe was the continent with the most epidemiological studies, the sample sizes recruited in Asian studies were approximately 1.8 times larger than those in European studies (with the exclusion of one health records-based study from Europe [37]). The scatterplot also illustrates the scarcity of data from Africa, North America, and Oceania which highlights future research needs.
The strengths of this systematic review and meta-analysis include the well-defined database search, rigorous study selection, and the critical appraisal process that aimed to minimize potential sources of bias (Appendices II and III). Furthermore, it bridges a gap in the literature by reporting the continent- and country-specific meta-analytic evaluation (Table 1; Fig. 3) as well as investigating the postulated MIH prevalence changes with an evidence-based approach (Table 2; Fig. 5). Despite the extensive efforts to include all eligible studies by thorough hand search, studies published in other languages or indexed in less commonly searched databases may have been overlooked. Methodological variations within the studies included in the review presented challenges for qualitative and quantitative data synthesis. In particular, the complexity and variability of the investigated hypomineralisation phenotypes may have complicated the interpretation of the findings. Only 44.4% of the included studies investigating MIH prevalence reported on M + IH status, often using inconsistent terminology or failing to explicitly report it, which required reviewers to deduct or calculate the needed data from tables, if possible. This highlights an issue with incomplete reporting, potentially causing trial investigators to overlook valuable data that could have been collected and reported at minimal additional effort. Clinically, discerning between the various phenotypes is challenging even for experienced epidemiologists, as it requires thorough documentation EH occurrences across the entire dentition. This comprehensive documentation is vital for accurate statistical exploration. However, for simplicity, some surveys assess only the index teeth, which limits the scope for further analysis. In principle, heterogeneity with regard to EH, MIH, and M + IH prevalence worldwide is expected due to the inherent limits of individual reports and are likely to have a potential influence on the results obtained. This can be attributed to various sources of bias, including differences in the diagnostic acuity of the investigators, inter- and intra-examiner reliability, regional deviations (urban or rural communities), and that the data– even from that from the same country– may represent diverse ethnic populations affecting generalizability of the results to a country, and investigations spanning extended time periods.
Another limitation to consider is study participants’ age. The EAPD recommends the MIH examination to occur at or after 8 years of age, to ensure the complete eruption of the index teeth [1, 3]. However, a definitive diagnosis of EH in the permanent dentition is ideally made after the age of 12, when the eruption status of the teeth is fully established. While the majority of studies used the EAPD criteria, several of which recruited children as young as 4- and 6-years-old, a period during which the index teeth may not have fully erupted, potentially causing an underestimation of the condition. Additionally, many studies assessed cohorts within a broad age range, sometimes extending up to 10 years age difference between participants [23, 117, 159], which may have influenced estimates and contributed to variability in the findings. Therefore, future cross-sectional studies should be designed in compliance with these recommendations [3].
While the EAPD criteria were used in 73.3% of the included studies, this was not always the case. For the recording of EH or MIH, several methods or indices have been recommended in recent decades. In the 2009 review by Jälevik [6], an equal number of studies used the EAPD and mDDE criteria. However, a 2018 review found that the majority of published studies employed the EAPD criteria, a trend which continues to date [12]. The use of varying diagnostic indices can complicate study comparability and potentially lead to differing prevalence estimates. Some reviews concluded that studies employing the EAPD index often report a significantly higher MIH prevalence as compared to those using other indices [10, 12]. However, the present subgroup meta-analysis found no significant differences in global MIH prevalence across different indices (p = 0.628), suggesting that overall estimates remain consistent despite variations in diagnostic criteria, and is in agreement with Sluka et al. [11] in this regard.
The present systematic review found no significant change in the global prevalence of MIH. It is plausible that the growing clinical recognition and awareness of MIH in the decades following its formal recognition by the EAPD could have contributed to perceptions of rising prevalence, without necessarily reflecting a true change in population-level epidemiology. Given the lack of data on all three hypomineralisation phenotypes from most countries worldwide (Fig. 4), future research should prioritize the data acquisition from underrepresented regions to provide a more comprehensive global assessment. For these studies, participant recruitment and diagnostic criteria should ideally align with EAPD recommendations [3]. Furthermore, clinical investigations should aim to assess the entire dentition for all enamel hypomineralisation phenotypes during dental examinations, maximizing data collection with minimal additional effort.
The considerable prevalence of enamel hypomineralisation worldwide has significant implications for dental health monitoring and clinical practice. While the current findings indicate that there were no changes in MIH prevalence, these conclusions should be ascertained by data from repeated cross-sectional studies utilizing highly matched cohorts and conducted at standardized intervals. Such studies would offer valuable insights for effective MIH monitoring. Further research is warranted to determine the most efficient epidemiological surveillance methods for MIH. In the clinical setting, dental practitioners should systematically assess patients for EH presentations using recognized diagnostic indices and aim to incorporate this assessment into routine examinations. This is especially relevant for high-risk populations, where a systematic monitoring approach will enable practitioners to better track the prevalence and incidence of EH and implement timely interventions based on individual patient needs.
EH, MIH, and M + IH remain prevalent worldwide with uneven distributions across countries and continents. The present data do not support the postulated increase in MIH prevalence rates. Future research should focus on collecting data from underrepresented countries, aligning with the EAPD recommendations for MIH diagnosis, and considering all EH phenotypes in dental examinations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Conceptualization and study design: J.K., Search of the literature: N.A, K-F.F., Formal analysis: N.A., Writing-original draft: N.A., K-F.F., J.K. Writing-review and editing: N.A.,K-F.F, J.K., F.S.
Funding
Open Access funding enabled and organized by Projekt DEAL.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
The dataset used in this study is available in the supplementary materials.
Declarations
Ethical approval
For this type of study, no ethical approval was needed.
Informed consent
For this type of study, no informed consent was needed.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weerheijm KL, Duggal M, Papagiannoulis L et al (2003) Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent 4:110–113 [PubMed] [Google Scholar]
- 2.Lygidakis NA, Garot E, Somani C et al (2022) Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an updated European academy of paediatric dentistry policy document. Eur Arch Paediatr Dent 23:3–21. 10.1007/S40368-021-00668-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lygidakis NA, Wong F, Jälevik B et al (2010) Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an EAPD policy document. Eur Arch Paediatr Dent 11:75–81. 10.1007/BF03262716 [DOI] [PubMed] [Google Scholar]
- 4.Kühnisch J, Heitmüller D, Thiering E et al (2014) Proportion and extent of manifestation of molar-incisor-hypomineralizations according to different phenotypes. J Public Health Dent 74:42–49. 10.1111/J.1752-7325.2012.00365.X [DOI] [PubMed] [Google Scholar]
- 5.Kühnisch J, Kabary L, Malyk Y et al (2018) Relationship between caries experience and demarcated hypomineralised lesions (including MIH) in the permanent dentition of 15-year-olds. Clin Oral Investig 22:2013–2019. 10.1007/S00784-017-2299-4 [DOI] [PubMed] [Google Scholar]
- 6.Jälevik B (2010) Prevalence and diagnosis of Molar-Incisor- hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent 11:59–64. 10.1007/BF03262714 [DOI] [PubMed] [Google Scholar]
- 7.Hernandez M, Boj JR, Espasa E (2016) Do we really know the prevalence of MIH? J Clin Pediatr Dentistry 40:259–263. 10.17796/1053-4628-40.4.259/HTM [DOI] [PubMed] [Google Scholar]
- 8.Zhao D, Dong B, Yu D et al (2018) The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent 28:170–179. 10.1111/IPD.12323 [DOI] [PubMed] [Google Scholar]
- 9.Schwendicke F, Elhennawy K, Krois J (2020) Prevalence, incidence, and burden of molar incisor hypomineralization. Molar Incisor Hypomineralization 21–31. 10.1007/978-3-030-31601-3_3
- 10.Lopes LB, Machado V, Mascarenhas P et al (2021) The prevalence of molar-incisor hypomineralization: a systematic review and meta-analysis. Scientific Reports 2021 11:1 11:1–20. 10.1038/s41598-021-01541-7 [DOI] [PMC free article] [PubMed]
- 11.Sluka B, Held U, Wegehaupt F et al (2024) Is there a rise of prevalence for molar incisor hypomineralization?? A meta-analysis of published data. BMC Oral Health 24. 10.1186/S12903-023-03637-0 [DOI] [PMC free article] [PubMed]
- 12.Schwendicke F, Elhennawy K, Reda S et al (2018) Global burden of molar incisor hypomineralization. J Dent 68:10–18. 10.1016/J.JDENT.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 13.da Costa Rosa T, Pintor AVB, Magno MB et al (2022) Worldwide trends on molar incisor and deciduous molar hypomineralisation research: a bibliometric analysis over a 19-year period. Eur Arch Paediatr Dent 23:133–146. 10.1007/S40368-021-00676-5 [DOI] [PubMed] [Google Scholar]
- 14.Altner S, Milutinovic I, Bekes K (2024) Possible etiological factors for the development of molar incisor hypomineralization (MIH) in Austrian children. Dentistry J 2024 12:44. 10.3390/DJ12030044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372. 10.1136/BMJ.N71 [DOI] [PMC free article] [PubMed]
- 16.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:1–10. 10.1186/S13643-016-0384-4/FIGURES/6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munn Z, Moola S, Lisy K et al (2020) Chap. 5: Systematic reviews of prevalence and incidence. In: Aromataris E, Munn Z (eds) JBI Manual for Evidence Synthesis. JBI
- 18.Munn Z, MClinSc SM, Lisy K et al (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 13:147–153. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 19.(1982) An epidemiological index of developmental defects of dental enamel (DDE Index). Commission on Oral Health, Research and Epidemiology. Int Dent J 32:159–167 [PubMed]
- 20.Nyaga VN, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Archives Public Health 72:1–10. 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haque Afzal S, Wigen TI, Skaare AB, Brusevold IJ (2023) Molar-incisor hypomineralisation in Norwegian children: prevalence and associated factors. Eur J Oral Sci 131. 10.1111/EOS.12930 [DOI] [PubMed]
- 22.Dourado DG, Lima CCB, Silva RNC et al (2021) Molar-incisor hypomineralization in quilombola children and adolescents: A study of prevalence and associated factors. J Public Health Dent 81:178–187. 10.1111/JPHD.12429 [DOI] [PubMed] [Google Scholar]
- 23.Grieshaber A, Waltimo T, Haschemi AA et al (2023) Prevalence of and factors associated with molar-incisor hypomineralisation in schoolchildren in the Canton of Basel-Landschaft, Switzerland. Clin Oral Investig 27:871–877. 10.1007/S00784-022-04648-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harz D, Catalán Gamonal B, Matute García S et al (2023) Prevalence and severity of molar-incisor hypomineralization, is there an association with socioeconomic status? A cross-sectional study in Chilean schoolchildren. Eur Archives Pediatr Dentistry 24:577–584. 10.1007/S40368-023-00820-3/FIGURES/4 [DOI] [PubMed] [Google Scholar]
- 25.Brejawi M, Venkiteswaran A, Ergieg SMO, Md Sabri BA (2024) Caries experience in children with molar–incisor hypomineralisation in Fujairah, united Arab Emirates and its association with hypomineralised teeth number. Eur Archives Pediatr Dentistry 25:211–216. 10.1007/S40368-024-00867-W/TABLES/2 [DOI] [PubMed] [Google Scholar]
- 26.Bonzanini LIL, Da Arduim AS, Lenzi TL et al (2021) Molar-incisor hypomineralization and dental caries: A hierarchical approach in a populational-based study. Braz Dent J 32:74–82. 10.1590/0103-6440202104511 [DOI] [PubMed] [Google Scholar]
- 27.Balmer R, Toumba J, Godson J, Duggal M (2012) The prevalence of molar incisor hypomineralisation in Northern England and its relationship to socioeconomic status and water fluoridation. Int J Paediatr Dent 22:250–257. 10.1111/J.1365-263X.2011.01189.X [DOI] [PubMed] [Google Scholar]
- 28.Arrow P (2009) Risk factors in the occurrence of enamel defects of the first permanent molars among schoolchildren in Western Australia. Community Dent Oral Epidemiol 37:405–415. 10.1111/J.1600-0528.2009.00480.X [DOI] [PubMed] [Google Scholar]
- 29.Arheiam A, Abbas S, Ballo L et al (2021) Prevalence, distribution, characteristics and associated factors of molar-incisor hypo-mineralisation among Libyan schoolchildren: a cross-sectional survey. Eur Archives Pediatr Dentistry 22:595–601. 10.1007/S40368-020-00594-Y/TABLES/2 [DOI] [PubMed] [Google Scholar]
- 30.Quispe DMA, De Priego GPM, Manco RAL, Portaro CP (2021) Molar incisor hypomineralization: prevalence and severity in schoolchildren of Puno, Peru. J Indian Soc Pedod Prev Dent 39:246–250. 10.4103/JISPPD.JISPPD_460_20 [DOI] [PubMed] [Google Scholar]
- 31.Amend S, Nossol C, Bausback-Schomakers S et al (2021) Prevalence of molar-incisor-hypomineralisation (MIH) among 6–12-year-old children in central Hesse (Germany). Clin Oral Investig 25:2093–2100. 10.1007/S00784-020-03519-7/TABLES/5 [DOI] [PubMed] [Google Scholar]
- 32.Almuallem Z, Alsuhaim A, Alqudayri A et al (2022) Prevalence and possible aetiological factors of molar incisor hypomineralisation in Saudi children: A cross-sectional study. Saudi Dent J 34:36–44. 10.1016/J.SDENTJ.2021.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alhowaish L, Baidas L, Aldhubaiban M et al (2021) Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children. Children 2021, Vol 8, Page 466 8:466. 10.3390/CHILDREN8060466 [DOI] [PMC free article] [PubMed]
- 34.Al-Nerabieah Z, AlKhouli M, Dashash M (2023) Prevalence and clinical characteristics of molar-incisor hypomineralization in Syrian children: a cross-sectional study. Scientific Reports 2023 13:1 13:1–8. 10.1038/s41598-023-35881-3 [DOI] [PMC free article] [PubMed]
- 35.Ahmad SH, Petrou MA, Alhumrani A et al (2019) Prevalence of Molar-Incisor hypomineralisation in an emerging community, and a possible correlation with caries, fluorosis and socioeconomic status. Oral Health Prev Dent 17:323–327. 10.3290/J.OHPD.A42725 [DOI] [PubMed] [Google Scholar]
- 36.Abo ElSoud AA, Mahfouz SM (2019) Prevalence and severity of molar incisor hypomineralization in school children of Suez Canal region: Cross-Sectional study. Egypt Dent J 65:909–915. 10.21608/EDJ.2015.71986 [Google Scholar]
- 37.Abdelaziz M, Krejci I, Banon J (2022) Prevalence of molar incisor hypomineralization in over 30,000 schoolchildren in Switzerland. J Clin Pediatr Dent 46:1–5. 10.17796/1053-4625-46.1.1 [DOI] [PubMed] [Google Scholar]
- 38.Abdalla HE, Abuaffan AH, Kemoli AM (2021) Molar incisor hypomineralization, prevalence, pattern and distribution in Sudanese children. BMC Oral Health 21:1–8. 10.1186/S12903-020-01383-1/TABLES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmadi R, Ramazani N, Nourinasab R (2012) Molar incisor hypomineralization: a study of prevalence and etiology in a group of Iranian children - PubMed. Iran J Pediatr 22:245–251 [PMC free article] [PubMed] [Google Scholar]
- 40.Dietrich G, Sperling S, Hetzer G (2003) Molar incisor hypomineralisation in a group of children and adolescents living in Dresden (Germany). Eur J Paediatr Dent 4:133–137 [PubMed] [Google Scholar]
- 41.Davenport M, Welles AD, Angelopoulou MV et al (2019) Prevalence of molar-incisor hypomineralization in Milwaukee, Wisconsin, USA: a pilot study. Clin Cosmet Investig Dent 11:109–117. 10.2147/CCIDE.S172736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.da Costa-Silva CM, Jeremias F, de Souza JF et al (2010) Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent 20:426–434. 10.1111/J.1365-263X.2010.01097.X [DOI] [PubMed] [Google Scholar]
- 43.Cho SY, Ki Y, Chu V (2008) Molar incisor hypomineralization in Hong Kong Chinese children. Int J Paediatr Dent 18:348–352. 10.1111/J.1365-263X.2008.00927.X [DOI] [PubMed] [Google Scholar]
- 44.Buchgraber B, Kqiku L, Ebeleseder KA (2018) Molar incisor hypomineralization: proportion and severity in primary public school children in Graz, Austria. Clin Oral Investig 22:757–762. 10.1007/S00784-017-2150-Y/TABLES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calderara PC, Gerthoux PM, Mocarelli P et al (2005) The prevalence of molar incisor hypomineralisation (MIH) in a group of Italian school children. Eur J Paediatr Dent 6:79–83 [PubMed] [Google Scholar]
- 46.Ciocan B, Săndulescu M, Luca R (2023) Real-World evidence on the prevalence of molar incisor hypomineralization in school children from Bucharest. Romania Child 10. 10.3390/CHILDREN10091563 [DOI] [PMC free article] [PubMed]
- 47.Hamdan M, Abu-Ghefreh EA, Al-Abdallah M, Rajab LD (2020) The prevalence and severity of molar incisor hypomineralization (MIH) among 8 year-old children in Amman, Jordan. Egypt Dent J 66:1989–1997. 10.21608/EDJ.2020.35468.1182 [Google Scholar]
- 48.Gurrusquieta B, Núñez V, López M (2017) Prevalence of molar incisor hypomineralization in Mexican children. J Clin Pediatr Dentistry 14:1 [DOI] [PubMed] [Google Scholar]
- 49.Grošelj M, Jan J (2013) Molar incisor hypomineralisation and dental caries among children in Slovenia - PubMed. Eur J Paediatr Dent 14:241–245 [PubMed] [Google Scholar]
- 50.Głódkowska N, Emerich K (2020) The impact of environmental air pollution on the prevalence of molar incisor hypomineralization in schoolchildren: A cross-sectional study. Adv Clin Exp Med 29:1469–1477. 10.17219/ACEM/128227 [DOI] [PubMed] [Google Scholar]
- 51.Glodkowska N, Emerich K (2019) Molar incisor hypomineralization: prevalence and severity among children from nothern Poland. Eur J Paediatr Dent 20:59–66. 10.23804/EJPD.2019.20.01.12 [DOI] [PubMed] [Google Scholar]
- 52.Ghanim A, Bagheri R, Golkari A, Manton D (2014) Molar-incisor hypomineralisation: a prevalence study amongst primary schoolchildren of Shiraz, Iran. Eur Arch Paediatr Dent 15:75–82. 10.1007/S40368-013-0067-Y [DOI] [PubMed] [Google Scholar]
- 53.Ghanim A, Morgan M, Mariño R et al (2011) Molar-incisor hypomineralisation: prevalence and defect characteristics in Iraqi children. Int J Paediatr Dent 21:413–421. 10.1111/J.1365-263X.2011.01143.X [DOI] [PubMed] [Google Scholar]
- 54.García-Pérez A, Pineda ÁEGA, Gutiérrez TV et al (2022) Impact of diseases of the hard tissues of teeth on oral health-related quality of life of schoolchildren in area with a high concentration of fluoride in drinking water. Community Dent Health 39:240–246. 10.1922/CDH_00078GARCIA-PEREZ07 [DOI] [PubMed] [Google Scholar]
- 55.Garcia-Margarit M, Catalá-Pizarro M, Montiel-Company JM, Almerich-Silla JM (2014) Epidemiologic study of molar-incisor hypomineralization in 8-year-old Spanish children. Int J Paediatr Dent 24:14–22. 10.1111/IPD.12020 [DOI] [PubMed] [Google Scholar]
- 56.Gambetta-Tessini K, Mariño R, Ghanim A et al (2019) The impact of MIH/HSPM on the carious lesion severity of schoolchildren from Talca. Chile Eur Archives Pediatr Dentistry 20:417–423. 10.1007/S40368-019-00416-W/TABLES/3 [DOI] [PubMed] [Google Scholar]
- 57.Gambetta-Tessini K, Mariño R, Ghanim A et al (2018) Carious lesion severity and demarcated hypomineralized lesions of tooth enamel in schoolchildren from Melbourne, Australia. Aust Dent J 63:365–373. 10.1111/ADJ.12626 [DOI] [PubMed] [Google Scholar]
- 58.Fteita D, Ali A, Alaluusua S (2006) Molar-incisor hypomineralization (MIH) in a group of school-aged children in Benghazi, Libya. Eur Arch Paediatr Dent 7:92–95. 10.1007/BF03320821 [DOI] [PubMed] [Google Scholar]
- 59.Folayan MO, Chukwumah NM, Popoola BO et al (2018) Developmental defects of the enamel and its impact on the oral health quality of life of children resident in Southwest Nigeria. BMC Oral Health 18:1–10. 10.1186/S12903-018-0622-3/TABLES/5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fernandes IC, Forte FDS, Sampaio FC (2021) Molar-incisor hypomineralization (MIH), dental fluorosis, and caries in rural areas with different fluoride levels in the drinking water. Int J Paediatr Dent 31:475–482. 10.1111/IPD.12728 [DOI] [PubMed] [Google Scholar]
- 61.Freitas Fernandes LH, Laureano ICC, Farias L et al (2021) Incisor molar hypomineralization and quality of life: A Population-Based study with Brazilian schoolchildren. Int J Dent 2021(6655771). 10.1155/2021/6655771 [DOI] [PMC free article] [PubMed]
- 62.Farias L, Laureano ICC, Fernandes LHF, et al (2021) Presence of molar-incisor hypomineralization is associated with dental caries in Brazilian schoolchildren. Braz Oral Res 35:e13. 10.1590/1807-3107BOR-2021.VOL35.0013 [DOI] [PubMed]
- 63.Estivals J, Fahd C, Baillet J et al (2023) The prevalence and characteristics of and the association between MIH and HSPM in South-Western France. Int J Paediatr Dent 33:298–304. 10.1111/IPD.13040 [DOI] [PubMed] [Google Scholar]
- 64.Emmatty T, Eby A, Joseph M et al (2020) The prevalence of molar incisor hypomineralization of school children in and around Muvattupuzha, Kerala. J Indian Soc Pedod Prev Dent 38:14–19. 10.4103/JISPPD.JISPPD_152_18 [DOI] [PubMed] [Google Scholar]
- 65.Elzein R, Chouery E, Abdel-Sater F et al (2021) Relation between molar-incisor hypomineralization (MIH) occurrence and war pollutants in bombarded regions: epidemiological pilot study in Lebanon. Niger J Clin Pract 24:1808–1813. 10.4103/NJCP.NJCP_702_20 [DOI] [PubMed] [Google Scholar]
- 66.Elzein R, Chouery E, Abdel-Sater F et al (2020) Molar incisor hypomineralisation in Lebanon: prevalence and clinical characteristics. Eur Archives Pediatr Dentistry 21:609–616. 10.1007/S40368-019-00505-W/FIGURES/3 [DOI] [PubMed] [Google Scholar]
- 67.Duarte MBS, Carvalho VR, Hilgert LA et al (2021) Is there an association between dental caries, fluorosis, and molar-incisor hypomineralization? J Appl Oral Sci 29:e20200890. 10.1590/1678-7757-2020-0890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Figueiredo APDR, Ribeiro APD, Dos Santos-Pinto LAM et al (2017) Are hypomineralized primary molars and canines associated with Molar-Incisor Hypomineralization? - PubMed. Pediatr Dent 39:445–449 [PubMed] [Google Scholar]
- 69.Lima M, de DM MJB, Dantas-Neta NB et al (2015) Epidemiologic study of Molar-incisor hypomineralization in schoolchildren in North-eastern Brazil - PubMed. Pediatr Dent 37:513–519 [PubMed] [Google Scholar]
- 70.Leppäniemi A, Lukinmaa PL, Alaluusua S (2001) Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res 35:36–40. 10.1159/000047428 [DOI] [PubMed] [Google Scholar]
- 71.Li L, Li J (2012) Investigation of molar-incisor hypomineralization among children from 6 to 11 years in Lucheng district, Wenzhou City. Shanghai Kou Qiang Yi Xue 21:576–579 [PubMed] [Google Scholar]
- 72.Damares Lago J, Restrepo M, Girotto Bussaneli D et al (2022) Molar-Incisor Hypomineralization: Prevalence Comparative Study in 6 Years of Interval. The Scientific World Journal 2022:4743252. 10.1155/2022/4743252 [DOI] [PMC free article] [PubMed]
- 73.Kukleva M, Petrova S, Kondeva V, Nihtyanova TI (2008) Molar incisor hypomineralisation in 7-to-14-year old children in Plovdiv, Bulgaria–an epidemiologic study. Folia Med (Plovdiv [PubMed]
- 74.Kuscu OO, Çaglar E, Aslan S et al (2009) The prevalence of molar incisor hypomineralization (MIH) in a group of children in a highly polluted urban region and a windfarm-green energy Island. Int J Paediatr Dent 19:176–185. 10.1111/J.1365-263X.2008.00945.X [DOI] [PubMed] [Google Scholar]
- 75.Kühnisch J, Kabary L, Malyk Y et al (2018) Relationship between caries experience and demarcated hypomineralised lesions (including MIH) in the permanent dentition of 15-year-olds. Clin Oral Investig 22:2013–2019. 10.1007/S00784-017-2299-4/FIGURES/1 [DOI] [PubMed] [Google Scholar]
- 76.Krishnan R, Ramesh M, Chalakkal P (2015) Prevalence and characteristics of MIH in school children residing in an endemic fluorosis area of India: an epidemiological study. Eur Arch Paediatr Dent 16:455–460. 10.1007/S40368-015-0194-8 [DOI] [PubMed] [Google Scholar]
- 77.Koruyucu M, Özel S, Tuna EB (2018) Prevalence and etiology of molar-incisor hypomineralization (MIH) in the City of Istanbul. J Dent Sci 13:318. 10.1016/J.JDS.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kirthiga M, Poornima P, Praveen R et al (2015) Prevalence and severity of molar incisor hypomineralization in children aged 11–16 years of a City in Karnataka, Davangere. J Indian Soc Pedod Prev Dent 33:213–217. 10.4103/0970-4388.160366 [DOI] [PubMed] [Google Scholar]
- 79.Kevrekidou A, Kosma I, Konstantinos A, Nikolaos K (2015) Molar incisor hypomineralization of Eight- and 14-year-old children: prevalence, severity, and defect characteristics. Pediatr Dent 37:455–461 [PubMed] [Google Scholar]
- 80.Khan A, Garg N, Mayall SS et al (2022) Prevalence, pattern, and severity of molar incisor hypomineralization in 8-12-year-old schoolchildren of Moradabad City. Int J Clin Pediatr Dent 15:168–174. 10.5005/JP-JOURNALS-10005-2362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kemoli AM (2008) Prevalence of molar incisor hypomineralisation in six to eight Year-Olds in two rural divisions in Kenya. East Afr Med J 85:514–520. 10.4314/EAMJ.V85I10.9668 [DOI] [PubMed] [Google Scholar]
- 82.Jurlina D, Uzarevic Z, Ivanisevic Z et al (2020) Prevalence of Molar–Incisor hypomineralization and caries in Eight-Year-Old children in Croatia. Int J Environ Res Public Health 2020 17:6358. 10.3390/IJERPH17176358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jeremias F, Souza JF, De, Costa Silva CM, Da et al (2013) Dental caries experience and Molar-Incisor hypomineralization. Acta Odontol Scand 71:870–876. 10.3109/00016357.2012.734412 [DOI] [PubMed] [Google Scholar]
- 84.López Jordi M, del Cortese C, Álvarez SG L, et al (2014) Comparison of the prevalence of molar incisor hypomineralization among children with different health care coverage in the cities of Buenos Aires (Argentina) and Montevideo (Uruguay). Salud Colect 10:243–251. 10.18294/SC.2014.225 [DOI] [PubMed] [Google Scholar]
- 85.Jasulaityte L, Weerheijm KL, Veerkamp JS (2008) Prevalence of molar-incisor-hypomineralisation among children participating in the Dutch National epidemiological survey (2003). Eur Arch Paediatr Dent 9:218–223. 10.1007/BF03262638 [DOI] [PubMed] [Google Scholar]
- 86.Jasulaityte L, Veerkamp JS, Weerheijm KL (2007) Molar incisor hypomineralization: review and prevalence data from the study of primary school children in Kaunas/Lithuania. Eur Arch Paediatr Dent 8:87–94. 10.1007/BF03262575 [DOI] [PubMed] [Google Scholar]
- 87.Janković S, Ivanović M, Davidović B, Lečić J (2014) Distribution and characteristics of molar-incisor hypomineralization. Vojnosanit Pregl 71:730–734. 10.2298/VSP1408730J [DOI] [PubMed] [Google Scholar]
- 88.Jälevik B, Klingberg G, Barregård L, Norén JG (2001) The prevalence of demarcated opacities in permanent first molars in a group of Swedish children. Acta Odontol Scand 59:255–260. 10.1080/000163501750541093 [DOI] [PubMed] [Google Scholar]
- 89.Irigoyen-Camacho ME, Villanueva-Gutierrez T, Castano-Seiquer A et al (2020) Evaluating the changes in molar incisor hypomineralization prevalence: A comparison of two cross-sectional studies in two elementary schools in Mexico City between 2008 and 2017. Clin Exp Dent Res 6:82–89. 10.1002/CRE2.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hussein AS, Faisal M, Haron M et al (2015) Distribution of molar incisor hypomineralization in Malaysian children attending university dental clinic. J Clin Pediatr Dentistry 39:219–223. 10.17796/1053-4628-39.3.219 [DOI] [PubMed] [Google Scholar]
- 91.Hernández Juyol M, Muñoz S, López F et al (2020) Prevalencia de La Hipomineralización incisivo molar En Una muestra de 772 escolares de La provincia de Barcelona. Articles Publicats En Revistes (Odontoestomatologia) 22:115–125 [Google Scholar]
- 92.Heitmüller D, Thiering E, Hoffmann U et al (2013) Is there a positive relationship between molar incisor hypomineralisations and the presence of dental caries? Int J Paediatr Dent 23:116–124. 10.1111/J.1365-263X.2012.01233.X [DOI] [PubMed] [Google Scholar]
- 93.Hasenauer L, Vogelsberger M, Bürkle V et al (2010) Prävalenz und Ausprägung der molar incisor hypomineralisation (MIH) in Salzburg und Tirol und Ein beitrag Zur erforschung der ursachen. Stomatologie 2010 107:3(107:43–50). 10.1007/S00715-010-0118-5
- 94.Mittal N, Sharma BB (2015) Hypomineralised second primary molars: prevalence, defect characteristics and possible association with molar incisor hypomineralisation in Indian children. Eur Archives Pediatr Dentistry 16:441–447. 10.1007/s40368-015-0190-z [DOI] [PubMed] [Google Scholar]
- 95.Quintero Y, Restrepo M, Rojas-Gualdrón DF et al (2022) Association between hypomineralization of deciduous and molar incisor hypomineralization and dental caries. Braz Dent J 33:113–119. 10.1590/0103-6440202204807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Preusser SE, Ferring V, Wleklinski C, Wetzel WE (2007) Prevalence and severity of molar incisor hypomineralization in a region of Germany -- a brief communication. J Public Health Dent 67:148–150. 10.1111/J.1752-7325.2007.00040.X [DOI] [PubMed] [Google Scholar]
- 97.Pitiphat W, Luangchaichaweng S, Pungchanchaikul P et al (2014) Factors associated with molar incisor hypomineralization in Thai children. Eur J Oral Sci 122:265–270. 10.1111/EOS.12136 [DOI] [PubMed] [Google Scholar]
- 98.Petrou MA, Giraki M, Bissar AR et al (2014) Prevalence of Molar-Incisor-Hypomineralisation among school children in four German cities. Int J Paediatr Dent 24:434–440. 10.1111/IPD.12089 [DOI] [PubMed] [Google Scholar]
- 99.Parikh DR, Ganesh M, Bhaskar V (2012) Prevalence and characteristics of molar incisor hypomineralisation (MIH) in the child population residing in Gandhinagar, Gujarat, India. Eur Arch Paediatr Dent 13:21–26. 10.1007/BF03262836 [DOI] [PubMed] [Google Scholar]
- 100.Padavala S, Sukumaran G (2018) Molar incisor hypomineralization and its prevalence. Contemp Clin Dent 9:S246–S250. 10.4103/CCD.CCD_161_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Oyedele TA, Folayan MO, Adekoya-Sofowora CA et al (2015) Prevalence, pattern and severity of molar incisor hypomineralisation in 8- to 10-year-old school children in Ile-Ife, Nigeria. Eur Arch Paediatr Dent 16:277–282. 10.1007/S40368-015-0175-Y [DOI] [PubMed] [Google Scholar]
- 102.Owlia F, Akhavan-Karbassi M-H, Rahimi R (2020) Could Molar-Incisor hypomineralization (MIH) existence be predictor of short stature?? Int J Prev Med 11:101. 10.4103/IJPVM.IJPVM_459_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ortega-Luengo S, Feijóo-Garcia G, Miegimolle-Herrero M et al (2024) Prevalence and clinical presentation of molar incisor hypomineralisation among a population of children in the community of Madrid. BMC Oral Health 24:1–9. 10.1186/S12903-024-04003-4/FIGURES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Oreano MDavila, Santos PS, Borgatto AF et al (2023) Association between dental caries and molar-incisor hypomineralisation in first permanent molars: A hierarchical model. Community Dent Oral Epidemiol 51:436–442. 10.1111/CDOE.12778 [DOI] [PubMed] [Google Scholar]
- 105.Ordonez-Romero I, Jijon-Granja Y, Ubilla-Mazzini W et al (2019) Distribution of molar incisor hypomineralization in Ecuadorian children. Dent Hypotheses 10:65–69. 10.4103/DENTHYP.DENTHYP_26_19 [Google Scholar]
- 106.Opydo-Szymaczek J, Gerreth K (2015) Developmental enamel defects of the permanent first molars and incisors and their association with dental caries in the region of Wielkopolska, Western Poland. Oral Health Prev Dent 13:461–469. 10.3290/J.OHPD.A33088 [DOI] [PubMed] [Google Scholar]
- 107.Olczak-Kowalczyk D, Krämer N, Gozdowski D, Turska-Szybka A (2023) Developmental enamel defects and their relationship with caries in adolescents aged 18 years. Scientific Reports 2023 13:1 13:1–9. 10.1038/s41598-023-31717-2 [DOI] [PMC free article] [PubMed]
- 108.Nisii F, Mazur M, De Nuccio C et al (2022) Prevalence of molar incisor hypomineralization among school children in Rome, Italy. Sci Rep 12. 10.1038/S41598-022-10050-0 [DOI] [PMC free article] [PubMed]
- 109.Ng JJ, Eu OC, Nair R, Hong CHL (2015) Prevalence of molar incisor hypomineralization (MIH) in Singaporean children. Int J Paediatr Dent 25:73–78. 10.1111/IPD.12100 [DOI] [PubMed] [Google Scholar]
- 110.Negre-Barber A, Montiel-Company JM, Catalá-Pizarro M, Almerich-Silla JM (2018) Degree of severity of molar incisor hypomineralization and its relation to dental caries. Sci Rep 2018 8(1):1–7. 10.1038/s41598-018-19821-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Arslanagic-Muratbegovic A, Markovic N, Zukanovic A et al (2020) Molar incisor hypomineralization: prevalence and severity in six to nine-year-old Sarajevo children. Eur J Paediatr Dent 21:243–247. 10.23804/EJPD.2020.21.03.16 [DOI] [PubMed] [Google Scholar]
- 112.Muratbegovic A, Markovic N, Ganibegovic Selimovic M (2007) Molar incisor hypomineralisation in Bosnia and Herzegovina: aetiology and clinical consequences in medium caries activity population. Eur Arch Paediatr Dent 8:189–194. 10.1007/BF03262595 [DOI] [PubMed] [Google Scholar]
- 113.Mulic A, Cehajic E, Tveit AB, Stenhagen KR (2017) How serious is molar incisor hypomineralisation (MIH) among 8- and 9-year-old children in Bosnia-Herzegovina? A clinical study. Eur J Paediatr Dent 18:153–157. 10.23804/EJPD.2017.18.02.12 [DOI] [PubMed] [Google Scholar]
- 114.Mittal R, Chandak S, Chandwani M et al (2016) Assessment of association between molar incisor hypomineralization and hypomineralized second primary molar. J Int Soc Prev Community Dent 6:34. 10.4103/2231-0762.175409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mittal NP, Goyal A, Gauba K, Kapur A (2014) Molar incisor hypomineralisation: prevalence and clinical presentation in school children of the Northern region of India. Eur Arch Paediatr Dent 15:11–18. 10.1007/S40368-013-0045-4 [DOI] [PubMed] [Google Scholar]
- 116.Mittal N (2016) Phenotypes of enamel hypomineralization and molar incisor hypomineralization in permanent dentition: identification, quantification and proposal for classification. J Clin Pediatr Dent 40:367–374. 10.17796/1053-4628-40.5.367 [DOI] [PubMed] [Google Scholar]
- 117.Mejía JD, Restrepo M, González S et al (2019) Molar incisor hypomineralization in Colombia: prevalence, severity and associated risk factors. J Clin Pediatr Dent 43:185–189. 10.17796/1053-4625-43.3.7 [DOI] [PubMed] [Google Scholar]
- 118.Mariam S, Goyal A, Dhareula A et al (2022) A case–controlled investigation of risk factors associated with molar incisor hypomineralization (MIH) in 8–12 year-old children living in Chandigarh, India. Eur Archives Pediatr Dentistry 23:97–107. 10.1007/S40368-021-00665-8/TABLES/3 [DOI] [PubMed] [Google Scholar]
- 119.Mahoney E, Morrison D (2011) Further examination of the prevalence of MIH in the Wellington region. N Z Dent J 107:79–84 [PubMed] [Google Scholar]
- 120.Mahoney EK, Morrison DG (2011) Further examination of the prevalence of MIH in the Wellington region. NZ Dent J 107:79–84 [PubMed] [Google Scholar]
- 121.Shin J-H, An U-J, Kim S, Jeong T-S (2010) THE PREVALENCE OF MOLAR INCISOR HYPOMINERALIZATION AND STATUS OF FIRST MOLARS IN PRIMARY SCHOOL CHILDREN. Journal of the Korean Academy of Pediatric Dentistry
- 122.Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH (2011) Molar incisor hypomineralisation: prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent 12:31–36. 10.1007/BF03262776 [DOI] [PubMed] [Google Scholar]
- 123.Zagdwon A, Toumba KJ, Curzon M (2022) The prevalence of developmental enamel defects in permanent molars in a group of english school children - PubMed. Eur J Paediatr Dent 3:91–96 [PubMed] [Google Scholar]
- 124.Yi X, Chen W, Liu M et al (2021) Prevalence of MIH in children aged 12 to 15 years in Beijing, China. Clin Oral Investig 25:355–361. 10.1007/S00784-020-03546-4 [DOI] [PubMed] [Google Scholar]
- 125.Yannam SD, Amarlal D, Rekha CV (2016) Prevalence of molar incisor hypomineralization in school children aged 8–12 years in Chennai. J Indian Soc Pedod Prev Dent 34:134–138. 10.4103/0970-4388.180438 [DOI] [PubMed] [Google Scholar]
- 126.Wuollet E, Laisi S, Salmela E et al (2016) Molar–incisor hypomineralization and the association with childhood illnesses and antibiotics in a group of Finnish children. Acta Odontol Scand 74:416–422. 10.3109/00016357.2016.1172342 [DOI] [PubMed] [Google Scholar]
- 127.Wuollet E, Laisi S, Salmela E et al (2014) Background factors of molar-incisor hypomineralization in a group of Finnish children. Acta Odontol Scand 72:963–969. 10.3109/00016357.2014.931459 [DOI] [PubMed] [Google Scholar]
- 128.Wogelius P, Viuff JH, Haubek D (2020) Use of asthma drugs and prevalence of molar incisor hypomineralization. Int J Paediatr Dent 30:734–740. 10.1111/IPD.12655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wogelius P, Haubek D, Nechifor A et al (2010) Association between use of asthma drugs and prevalence of demarcated opacities in permanent first molars in 6-to-8-year-old Danish children. Community Dent Oral Epidemiol 38:145–151. 10.1111/J.1600-0528.2009.00510.X [DOI] [PubMed] [Google Scholar]
- 130.Wogelius P, Haubek D, Poulsen S (2008) Prevalence and distribution of demarcated opacities in permanent 1st molars and incisors in 6 to 8-year-old Danish children. Acta Odontol Scand 66:58–64. 10.1080/00016350801926941 [DOI] [PubMed] [Google Scholar]
- 131.Weerheijm KL, Groen HJ, Beentjes VEVM, Poorterman JHG (2001) Prevalence of cheese molars in 11-year-old Dutch children. J Dent Child 68:259–262 [PubMed] [Google Scholar]
- 132.Villanueva-Gutiérrez T, Irigoyen-Camacho ME, Castaño-Seiquier A et al (2019) Prevalence and severity of Molar-Incisor hypomineralization, maternal education, and dental caries: A Cross-Sectional study of Mexican schoolchildren with low socioeconomic status. J Int Soc Prev Community Dent 9:513–521. 10.4103/JISPCD.JISPCD_130_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vicioni-Marques F, Carvalho MR, Raposo F et al (2023) Association of dental hypersensitivity and anxiety in children with molar-incisor hypomineralisation (MIH). Eur Archives Pediatr Dentistry 24:313–319. 10.1007/S40368-023-00803-4/TABLES/3 [DOI] [PubMed] [Google Scholar]
- 134.Verma S, Dhinsa K, Tripathi AM et al (2022) Molar incisor hypomineralization: prevalence, associated risk factors, its relation with dental caries and various enamel surface defects in 8-16-year-old schoolchildren of Lucknow district. Int J Clin Pediatr Dent 15:1–8. 10.5005/JP-JOURNALS-10005-2088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Vanhée T, Poncelet J, Cheikh-Ali S, Bottenberg P (2022) Prevalence, caries, dental anxiety and quality of life in children with MIH in Brussels, Belgium. J Clin Med 2022 11:3065. 10.3390/JCM11113065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Tourino LFPG, Corrêa-Faria P, Ferreira RC et al (2016) Association between molar incisor hypomineralization in schoolchildren and both prenatal and postnatal factors: A Population-Based study. PLoS ONE 11:e0156332. 10.1371/JOURNAL.PONE.0156332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Thakur H, Kaur A, Singh N et al (2020) Prevalence and clinical characteristics of Molar-Incisor hypomineralization in 8-16-year-old children in industrial town of Solan district of Himachal Pradesh. Int J Clin Pediatr Dent 13:230–234. 10.5005/JP-JOURNALS-10005-1767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rehaman T, Ravichandra KS, Muppa R et al (2021) Molar incisor hypomineralization prevalence in the schoolchildren of Gannavaram Mandal, Krishna district, Andhra Pradesh, India: A Cross-sectional study. Int J Clin Pediatr Dent 14:737–740. 10.5005/JP-JOURNALS-10005-2097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Subramaniam P, Gupta T, Sharma A (2016) Prevalence of molar incisor hypomineralization in 7–9-year-old children of Bengaluru City, India. Contemp Clin Dent 7:11. 10.4103/0976-237X.177091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Soviero V, Haubek D, Trindade C et al (2009) Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol Scand 67:170–175. 10.1080/00016350902758607 [DOI] [PubMed] [Google Scholar]
- 141.Souza JF, Jeremias F, Costa-Silva CM et al (2013) Aetiology of molar-incisor hypomineralisation (MIH) in Brazilian children. Eur Arch Paediatr Dent 14:233–238. 10.1007/S40368-013-0054-3 [DOI] [PubMed] [Google Scholar]
- 142.Sosa-Soto J, Padrón-Covarrubias AI, Márquez-Preciado R et al (2022) Molar incisor hypomineralization (MIH): prevalence and degree of severity in a Mexican pediatric population living in an endemic fluorosis area. J Public Health Dent 82:3–10. 10.1111/JPHD.12446 [DOI] [PubMed] [Google Scholar]
- 143.Sönmez H, Yıldırım G, Bezgin T (2013) Putative factors associated with molar incisor hypomineralisation: an epidemiological study. Eur Arch Paediatr Dent 14:375–380. 10.1007/S40368-013-0012-0 [DOI] [PubMed] [Google Scholar]
- 144.Shah VU, Dave BH, Chari DN, Shah KA (2023) Prevalence, severity and associated risk indicators of molar incisor hypomineralization amongst 8–13-year-old children of Vadodara district Gujarat: A Cross-sectional study. Int J Clin Pediatr Dent 16:280. 10.5005/JP-JOURNALS-10005-2570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Schmalfuss A, Stenhagen KR, Tveit AB et al (2016) Canines are affected in 16-year-olds with molar-incisor hypomineralisation (MIH): an epidemiological study based on the Tromsø study: fit futures. Eur Arch Paediatr Dent 17:107–113. 10.1007/S40368-015-0216-6 [DOI] [PubMed] [Google Scholar]
- 146.Salem K, Aziz D, Asadi M (2016) Prevalence and predictors of molar incisor hypomineralization (MIH) among rural children in Northern Iran. Iran J Public Health 45:1528 [PMC free article] [PubMed] [Google Scholar]
- 147.Saldarriaga A, Rojas-Gualdrón D, Restrepo M et al (2021) Dental fluorosis severity in children 8–12 years old and associated factors. Acta Odontol Latinoam 34:156–165. 10.54589/AOL.34/2/156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Saitoh M, Nakamura Y, Hanasaki M et al (2018) Prevalence of molar incisor hypomineralization and regional differences throughout Japan. Environ Health Prev Med 23:1–6. 10.1186/S12199-018-0748-6/FIGURES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rodríguez-Rodríguez M, Carrasco-Colmenares W, Ghanim A et al (2021) Prevalence and distribution of molar incisor hypomineralization in children receiving dental care in Caracas metropolitan area, Venezuela. Acta Odontol Latinoam 34:104–112. 10.54589/AOL.34/2/104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Robles MJ, Ruiz M, Bravo-Perez M et al (2013) Prevalence of enamel defects in primary and permanent teeth in a group of schoolchildren from Granada (Spain). 10.4317/MEDORAL.18580. Med Oral Patol Oral Cir Bucal 18: [DOI] [PMC free article] [PubMed]
- 151.Reyes MRT, Fatturi AL, Menezes JVNB et al (2019) Demarcated opacity in primary teeth increases the prevalence of molar incisor hypomineralization. Braz Oral Res 33(e048). 10.1590/1807-3107BOR-2019.VOL33.0048 [DOI] [PubMed]
- 152.Reis P, Jorge R, Americano G et al (2021) Prevalence and severity of molar incisor hypomineralization in Brazilian children. Pediatr Dent 43:270–275 [PubMed] [Google Scholar]
- 153.Ravindran R, Saji AM (2016) Prevalence of the developmental defects of the enamel in children aged 12–15 years in Kollam district. J Int Soc Prev Community Dent 6:28. 10.4103/2231-0762.175407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Raposo F, De Carvalho Rodrigues AC, Lia ÉN, Leal SC (2019) Prevalence of hypersensitivity in teeth affected by Molar-Incisor hypomineralization (MIH). Caries Res 53:424–430. 10.1159/000495848 [DOI] [PubMed] [Google Scholar]
- 155.Rai PM, Jain J, Raju AS et al (2019) Prevalence of molar incisor hypomineralization among school children aged 9 to 12 years in Virajpet, Karnataka, India. Open Access Maced J Med Sci 7:1042–1046. 10.3889/OAMJMS.2019.224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rai A, Singh A, Menon I et al (2018) Molar incisor hypomineralization: prevalence and risk factors among 7–9 years old school children in Muradnagar, Ghaziabad. Open Dent J 12:714–722. 10.2174/1745017901814010714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shrestha R, Upadhaya S, Bajracharya M (2014) Prevalence of molar incisor hypomineralisation among school children in Kavre. Kathmandu Univ Med J 12:38–42. 10.3126/KUMJ.V12I1.13631 [DOI] [PubMed] [Google Scholar]
- 158.Olczak-Kowalczyk D, Krämer N, Gozdowski D, Turska-Szybka A (2023) Developmental enamel defects and their relationship with caries in adolescents aged 18 years. Sci Rep 13. 10.1038/S41598-023-31717-2 [DOI] [PMC free article] [PubMed]
- 159.Folayan MO, Chukwumah NM, Popoola BO et al (2018) Developmental defects of the enamel and its impact on the oral health quality of life of children resident in Southwest Nigeria. BMC Oral Health 18. 10.1186/S12903-018-0622-3 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset used in this study is available in the supplementary materials.