Abstract
Background
One factor that contributes to balance impairment after ACL reconstruction is balance. Balance impairment leads to decreased performance in athletes, limitations in daily activities, and increases the risk of re-injury. Despite the importance of addressing this issue, previous studies do not appear to have directly compared virtual reality (VR) training with proprioception training. This systematic review compares the effects of proprioception exercise and VR on postural balance in individuals with anterior cruciate ligament reconstruction (ACL-R).
Methods
A search was conducted in four databases: PubMed, Science Direct, Web of Science (WOS), and Scopus to find available sources from the beginning to the end of February 2025. Studies that assessed postural balance were selected. Quality assessment, risk of bias, and Quality assessment of the body of evidence of the studies were performed using the PEDro scale, A revised tool to assess risk of bias (RoB 2), and GRADE, respectively, by two authors, and any discrepancies were reported by a third person and consensus was reached by three people. Meta-analysis was performed using the Comprehensive Meta-Analysis V.3.0 software.
Results
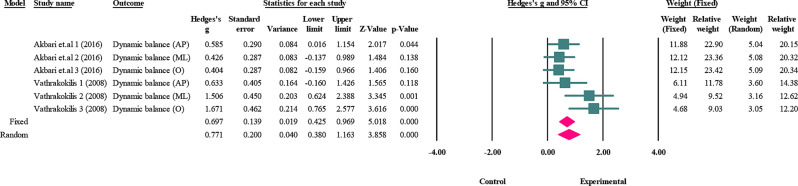
Nine studies, with a total of 333 participants, Including 279 men and 54 women, were included in the present study. The meta-analysis conducted on the proprioception exercises section, which were evaluated dynamic balance in group 1 (Biodex Balance System), has Hedges` g an effect size (95% confidence intervals) of 0.697 (0.429 to 0.969), and in group 2 (Kinesthetic Ability Trainer) has 2.465 (-1.534 to 6.463) and static balance has 0.302 (0.037 to 0.568). VR exercise in dynamic balance has 0.390 (0.077 to 0.704). The quality of evidence for studies on VR exercises was high, proprioception exercises were low in static balance, and dynamic balance was moderate in Group 1 and very low in Group 2.
Conclusion
Research shows that both proprioception and VR exercises can help improve postural balance. Interestingly, when comparing the two under similar conditions, VR exercises may be more effective. The engaging nature of VR exercises can be a real advantage in helping people stick with the exercise and achieve better results. While these findings are promising, more high-quality research is needed. Future studies using rigorous methods will help us confirm these benefits and better understand how VR can be used to improve postural balance.
Clinical trial number
Not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-025-08823-5.
Keywords: Anterior cruciate ligament reconstruction, Balance, Stability, Virtual reality, Proprioception
Background
The anterior cruciate ligament (ACL) is essential for maintaining knee joint stability. Unfortunately, injuries to this ligament are quite common among athletes and can lead to issues like instability, swelling, and severe pain, which significantly affect a person’s quality of life [1]. When these injuries occur, timely surgical intervention can help reconstruct the knee [2]. Anterior cruciate ligament reconstruction (ACL-R) typically provides greater mechanical stability, but Its effect on function depends on various factors, including individual characteristics, adherence to rehabilitation programs, and the extent of injury [3]. However, the high rates of re-injury raise concerns about the effectiveness of postoperative rehabilitation. Many patients find that their recovery programs do not sufficiently restore the mobility and neuromuscular control necessary to avoid future injuries. As a result, those who have undergone ACL-R often experience ongoing muscle weakness, balance issues, and uneven movement patterns [4, 5]. This decline in their ability to manage posture and movement can be quite significant [6]. Given these challenges, it’s vital to prioritize comprehensive rehabilitation programs after surgery. These programs should focus not only on physical healing but also on enhancing neuromuscular coordination. This approach will play a key role in ensuring that patients can safely and effectively return to their activities [6, 7].
One of the significant challenges following an ACL injury is the impairment of neuromuscular control in the lower extremity. Enhancing this control is crucial for facilitating a successful return to functional activities and for lowering the risk of re-injury. Implementing neuromuscular training protocols alongside proprioceptive exercises can aid in the development of compensatory movement patterns and significantly enhance postural stability [8, 9]. These training methods have been found to be both safe and effective, particularly for those who have undergone ACL-R [10]. By focusing on these areas, we can better support recovery and promote long-term health and mobility for individuals dealing with such injuries [10].
Hewitt et al. (2002) emphasize that ligament injuries can impair knee proprioception and neuromuscular control, highlighting the importance of tailored rehabilitation programs for athletes seeking to resume high-level sports activities [11]. Balance training using a balance board can commence early in the postoperative phase. Proprioception training effectively starts as soon as the patient begins weight-bearing during this initial recovery period [11]. Early initiation of movement at a level that the patient tolerates ensures early recovery of proprioception and progression in sports facilitates proprioception [11]. Since the rehabilitation process is just as important as the surgery itself, research has shown that ACL-R should be used in conjunction with a detailed postoperative rehabilitation program to help patients return to their pre-injury levels of physical activity [12]. Evidence suggests that proprioception and balance exercises can significantly improve outcomes for people with ACL deficiencies, enhancing joint position sense (JPS), muscle strength, and perceived knee function [10].
Proprioception exercises play an important role in the rehabilitation process and improving the function of the knee joint [13]. The goal of these exercises is to improve proprioception and balance, and ultimately prevent re-injury [14]. These exercises activate proprioceptors, which are located in the knee and other joints. These receptors send mechanical information about the position and movement of the joints to the nervous system. This allows the person to better regulate their movements, resulting in increased knee stability. This is especially crucial after surgery, such as ACL-R [15].
Furthermore, proprioception training following ACL-R is also found to be beneficial [10, 16].
Proprioception protocols used after ACL-R have primary goals of improving JPS and secondary goals of improving stability and postural control. The exercises in these protocols challenge individuals to improve joint receptors and, on the other hand, can coordinate nerve and muscle activity [15].
In recent years, one of the exercise interventions that has attracted the attention of researchers is rehabilitation using virtual reality (VR) exercises [17, 18]. These exercises use digital technologies to simulate real-world environments and create interactive experiences. In fact, these types of exercises can include motor games, sports simulations, and challenging activities specifically designed to enhance balance and postural control. VR can provide patients with greater motivation and significantly improve their learning experience [19].
VR protocols include balance and strength exercises. These exercises are presented in real scenarios using different devices [20]. The use of VR exercises in sports rehabilitation allows patients to train in a simulated environment, and strength and balance exercises mainly focus on the lower extremities to improve postural control. The virtual environment shifts the patient’s focus from knee pain to interaction with the virtual environment and increases their mental readiness and motivation to participate in the rehabilitation process. This factor is in the secondary goals of this group and can help enhance motor learning of the central nervous system [21].
The use of VR and game-based exercises can be considered an effective tool in the delivery of rehabilitation interventions after lower limb surgeries [22]. In the context of rehabilitation exercises after ACL-R and balance exercises, this technology may help improve knee joint function, strengthen lower limb muscles, increase proprioception, and manage pain [1].
In a systematic review by Cortés-Pérez et al., virtual reality training improved knee function, balance, and muscle strength after ACL injury. Knee function was assessed using the Lysholm Knee Joint Score, balance with the star test, and muscle strength with an isokinetic dynamometer. Strengthening of the quadriceps and hamstrings occurred as a result of virtual reality training, which resulted in better function, balance, and strength [20].
However, conflicting results were observed in the study by Baltaci et al. (2013) that compared two traditional and VR training programs; this study showed that both control and experimental groups achieved similar results in the area of muscle strength, dynamic balance, and motor performance measures. In general, ACL injury, like any other sports injury, cannot be limited to a musculoskeletal dimension, and cognitive and neurological factors also need to be considered in the assessment and prevention of injuries [18].
Emerging insights suggest that incorporating VR can enhance adherence to rehabilitation protocols, as patients often find these exercises more engaging. This improved adherence is crucial, as consistent practice is paramount for effective recovery. Additionally, VR can provide real-time feedback, allowing patients to monitor their progress and make necessary adjustments to their technique. Multidimensional reintegration approaches and virtual reality technologies are two new methods that can assist bridge this gap between science and practice [23].
Based on the conducted studies, it appears that no systematic review has yet compared the effects of VR and proprioception exercises on the postural balance of individuals with ACL reconstruction (ACL-R). Confirming the effectiveness of each of these protocols exclusively and comparing them with each other could provide practitioners in this field with a clear understanding of the most effective method to choose based on the current situation and allow them to achieve the desired outcomes. This would also be facilitated by clarifying the quality of the evidence and clinical outcomes. Therefore, this study aims to compare the effects of two exercise methods—proprioception exercises and VR on the postural balance of people with ACL-R.
Method
We carried out this review in accordance with the PRISMA guidelines [24]. This study registered in PROSPERO with the number: CRD420251000153.
Literature search strategy
Articles were searched in four databases: Scopus, Web of Science, PubMed, and ScienceDirect. The review included articles published in English from the beginning to February 2025, focusing on VR and Proprioception interventions that assessed postural control in Athletes with ACL-R. The analysis utilized the PICOS framework:
P: Population: individual with unilateral ACL_R: This includes both male and female individual who have undergone surgery for ACL injuries.
I: Intervention: Intervention involves the use of Proprioception and VR.
C: Comparison: Conventional rehabilitation and No intervention.
O: Outcome: Postural balance (Static and dynamic balance, and Postural control).
S: Study type: Randomized control trials (RCTs) and quasi-experimental studies.
To implement the search strategy, Relevant terms were selected using the MeSH (Medical Subject Headings) terms. Taking the words chosen from the MeSH into account, these terms were combined with additional keywords. These keywords usually included more general terms or synonyms in the scientific literature. Alongside our database searches, we conducted a manual search to maximize the identification of pertinent research. A complete list of the keywords utilized can be found in Table in appendix 1.
Eligibility criteria
Inclusion criteria
Written in English, Mean age of subjects was 16 to 40 years old, Control group was required to fulfill at least 1 of the following conditions: athlete with ACL-R, exercise protocol.
Exclusion criteria
No full text access, Systematic reviews, meta-analysis, Ph.D thesis, case studies, comments, Control criteria not met Post intervention results not reported.
Study selection
Records gathered from our database searches were entered into EndNote version 20. After eliminating duplicates, two independent authors reviewed the titles and abstracts to identify studies that might find our inclusion criteria. We then thoroughly assessed the full texts of the studies that remained to determine their eligibility. In cases where the two authors disagreed, a third author was brought in to provide an additional perspective. Ultimately, our final report reflects the consensus reached by all three authors.
Data extraction
The necessary information was gathered from the selected studies using a standardized form. This data encompassed the first author’s name, publication year, country of the study, and specific sample details, including the number of male and female participants. We also recorded the mean age and standard deviation for each group and gender, as well as information related to the interventions such as exercise duration, frequency per week, type of intervention, graft type, outcome measures, measurement tools used, and key results. Two authors independently conducted the data extraction, while a third author helped ensure consistency and accuracy across the data collected.
Risk of bias assessment
The RoB 2.0 tool was utilized to assess bias in detail. This tool consists of questions that can be answered with “yes,” “probably yes,” “probably no,” “no,” or “no information”. Finally, these scores are summed into an overall assessment, which includes a classification of “low”, “some concern” or “high” [25]. Two researchers independently reviewed the studies, and in the event of disagreement between the two investigators, a consensus was reached and the assessment was assessed by discussion with a third investigator.
Quality assessment
We using the PEDro scale, which consists of 11 questions. Each question can earn a maximum of one point, resulting in a total score ranging from 0 to 11. A score of 7 or higher reflects a high quality study, while scores between 5 and 6 indicate average quality. Studies scoring below 4 are considered to be of low quality [26]. Each study was reviewed by two independent authors and in case of disagreement between the two authors, a third person reviewed the study separately and a consensus was reached between the three authors.
Quality assessment of the body of evidence
The quality of evidence in each part was evaluated with the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology [27]. The assessment for each primary outcome measure considered five criteria: risk of bias, inconsistency, indirectness, imprecision, and publication bias [27].
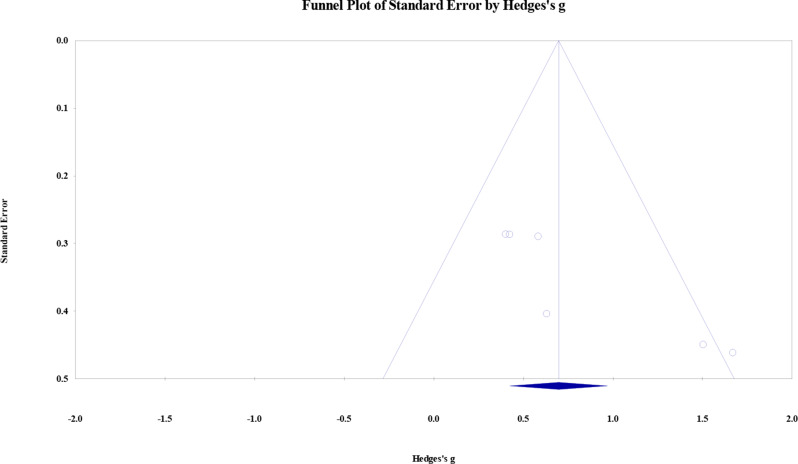
Publication bias
To evaluate publication bias, a funnel plot was created, and for instances where the number of studies per outcome measure exceeded three, the Begg test for asymmetry was conducted. The significance level for this test is 0.05, with numbers lower than this value indicating the possibility of bias and higher numbers indicating the likelihood of no publication bias [28].
Statistical analyses
This study conducted a meta-analysis utilizing Comprehensive Meta Analysis V3 (CMA) software, focusing on two indices of balance: static and dynamic. We included the mean, standard deviation of the post-test balance variable, and the sample sizes from the two study groups to calculate the effect size of the interventions. A 95% confidence interval (CI) was applied across all indices to ensure robust statistical analysis. To assess heterogeneity among the studies, we used the I2 index. 0-40%, might not be important; 30-60%, moderate heterogeneity; 50-90%, substantial heterogeneity; and 75-100%, considerable heterogeneity [29]. alpha level of 0.05 was considered for the measured tests. For determine the impact of the training, Hedges’ g was used to calculate effect sizes (ESs). Effect sizes were evaluated based on these threshold values: less than 0.2, trivial; 0.2–0.6, small; 0.6–1.2, moderate; 1.2-2.0, large; 2.0–4.0, very large; and greater than 4.0, nearly perfect [30, 31]. When heterogeneity ≥ 50% we applied a random-effects model; conversely, if it was below 50% we utilized a fixed-effects model [32].
Result
Selection criteria
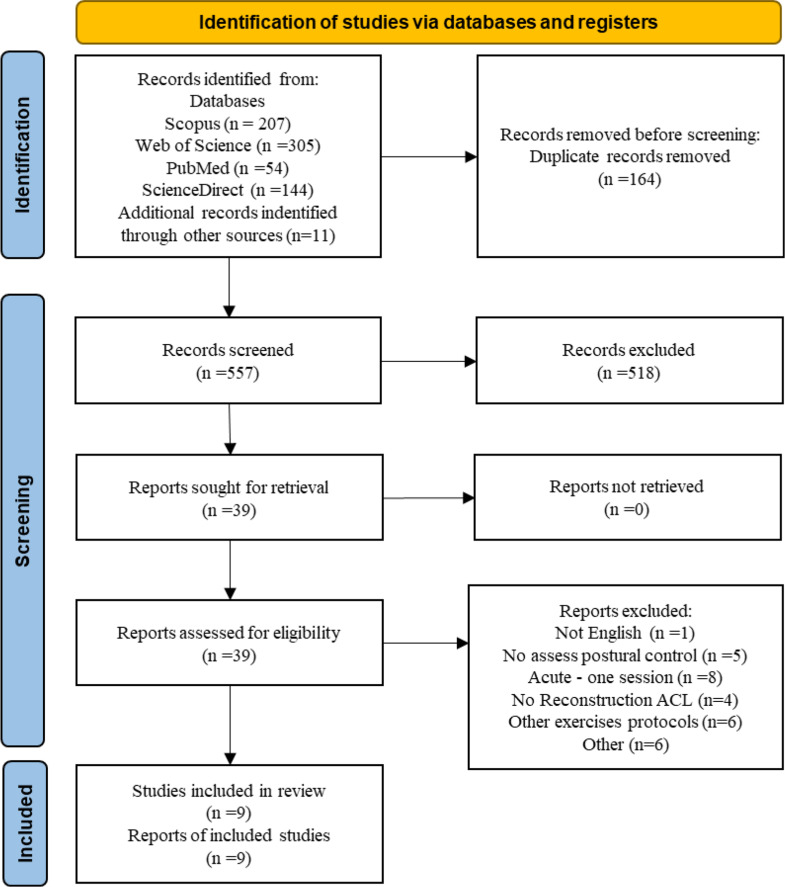
A comprehensive search of the databases yielded a total of 721 studies. After eliminating duplicates (n = 164), we were left with 557 unique studies. Two authors then independently assessed the titles and abstracts of these studies, resulting in the exclusion of 518. Ultimately, 39 studies advanced to the full-text review stage. Following a collaborative evaluation by the two authors, 9 studies were deemed suitable based on our established criteria. The research process is illustrated in Fig. 1. A summary of the details extracted from the studies is reported in Tables 1 and 2.
Fig. 1.
Flow diagram
Table 1.
Summary of studies conducted on the effect of proprioception exercise interventions on postural balance athlete with ACL-R
| Article | Sample | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|
|
Author(s) (Year/Country) |
Number (M/F) |
Age(y) Mean ± SD |
Duration (Weeks/ Sesseion Per week) | Type of Intervention | Graft Type | Outcome Measure | Instrument | Result |
|
Grueva–Pancheva et al. (14) (2023/Bulgaria) |
Experimental group, n = 19 (16/3) |
29.1 ± 8.1 | NR /3 | Cryotherapy, PM, PKEDL, Co-activation of quadriceps and ishiocrural group in CKC, AAM, AHM, Locomotion, Active knee extension in CKC (later with theraband resistance), PES | NR | COP, mean amplitude, mean velocity, sway path | KAT1 | Reduced volatility in the experimental group |
|
Control group, n = 21 (20/1) |
31.1 ± 7.6 | NR /3 | Cryotherapy, PM, PKEDL, AAM, CPM (Knee), AHM, Locomotion | NR | ||||
|
Akbari et al. (33) (2015/Iran) |
Experimental group, n = 24 (M) |
22.33 ± 11.03 | 2/6 | SLS, Step-up exercises | NR | Static, and Dynamic balance | BBS | Lack of significance of balance training on static and dynamic stability |
|
control group, n = 24 (M) |
20.33 ± 10.9 | No intervention | ADL | - | ||||
|
Risberg et al. (9) (2007/Norway) |
Balance and stability exercise group (NT) n = 39 (26/13) |
M (16.7–39.6) F(20.6 − 37.9) |
24/3 | BSE, Plyo, agility drills, SPP | bone-patellar tendon-bone graft | Muscle Strength, Balance, Proprioception, functional Performance, Health-Related Quality of Life, Cincinnati Knee score, VAS | BBS, TTDPM, KAT20001, Cybex 6000 | Significant difference in Cincinnati knee and VAS scores in the NT group compared to the ST group |
|
Strength Training group (ST) n = 35 (21/14) |
M(19.4–40.3) F(19.8–38.0) |
24/3 | ST | bone-patellar tendon-bone graft | ||||
|
Vathrakokilis et al. (34) (2008/Greece) |
Experimental group, n = 12 (8/4) |
28.6 ± 6.1 | 8/3 | Static and dynamic SLS on a hemi-cylindrical board (A/P), Static and dynamic SLS on a hemi-cylindrical board(M-L), SLS on a hemispherical board (all directions) | semitendinosus and gracilis tendon graft | Overall stability index (OSI), stability index A-P, and M-L, stability in sagittal plane (A/PSEO), dynamic stability in sagittal plane (A/PMEO), stability in frontal plane (M/LSEO), dynamic stability in frontal plane (M/LMEO), stability in all directions (RBSEO) | Balance Boards, BSS | Significance in balance stability indices in the experimental group compared to the control group |
|
control group, n = 12 (9/3) |
28.6 ± 6.1 | No intervention | ADL | semitendinosus and gracilis tendon graft | ||||
|
Unver Kocak et al. (13) (2010/Turkey) |
Experimental group, n = 27 (22/5) |
26.51 ± 8.24 | 12/3 | Proprioception exercises |
bone-patellar tendon-bone graft(n = 17) hamstring graft (n = 10) |
Static and dynamic balance, Lysholm knee scoring | KAT20001 |
Static balance: significance between operated and non-operated limbs, significant over time Dynamic balance: no significance |
|
control group, n = 18 (14/4) |
20.88 ± 3.59 | No intervention | ADL | - | ||||
1.Posturographic system, AAM: Ankle active movements, ADL: Activities of Daily Living, AHM: Active hip movements, A/PSEO: stability in sagittal plane, A/PMEO: dynamic stability in sagittal plane, BBS: Biodex Balance System, BPTB: bone-patellar tendon-bone, BSE: Balance and stability exercises, COP: Center of pressure, CPM (Knee): Continuous passive movement through artromot machine for the knee, F: Female, M: Male, M/LMEO: dynamic stability in frontal plane, M/LSEO: stability in frontal plane, NR: Not reported, OSI: Overall stability index, PES: Proprioception exercises in standing, PKEDL: Passive knee extension in face down lying position, PM: Patella mobilization, RBSEO: stability in all directions, SD: Standard deviation, SLS: Single leg stance, SPP: sport-specific exercises, ST: Strength Training, STG: semitendinosus and gracilis tendon, TTDPM: threshold to detection of passive motion, VAS: Visual Analogue Scale
Table 2.
Summary of studies conducted on the effect of VR exercise interventions on postural balance athlete with ACL-R
| Article | Sample | Intervention | ||||||
|---|---|---|---|---|---|---|---|---|
|
Author(s) (Year/Country) |
Number (M/F) |
Age(y) Mean ± SD |
Duration (Weeks/ Sesseion Per week) | Type of Intervention | Graft Type | Outcome Measure | Instrument | Result |
|
Gsangaya et al. (21) (2023/Malaysia) |
Experimental group, n = 15 (13/2) |
28.6 ± NR | 12 | Headmaster 3.0, Dream Match Tennis, Beat Saber for PSVR, Knockout League, Hoops, Richie’s Plank Experience, Pong It VR, Egg Time VR, Sparc VR | hamstring autograft | Limb loading, balance, range of motion of the knee, hop tests, pain score, IKDC score | Nintendo Wii, Lower Limb Weighing Device, goniometer, IKDC 2000, Y-balance |
Significant improvement in pain scores and IKDC scores in the experimental group compared to the control group No significance in other variables |
|
Control group, n = 15 (10/5) |
25.1 ± NR | 12 | AAROM (Knee), CKC flexion, prone hanging, isometric quadriceps, SLR, PKE, PRKFE, SLB exercises, cycling, additional jogging activities | hamstring autograft | ||||
|
Betul Karakoc et al. (35) (2019/Turkey) |
Experimental group n = 14 (M) |
31 ± 8.41 | 6/3 | Soccerheading, Skiing, Tabletilt, Penguinslide | NR | Pain, LEFS, balance, COG | Nintendo Wii balance board | No significant difference was observed between the two groups in the rate of change in any of these parameters. |
|
Control group, n = 8 (M) |
24 ± 5.94 | 6/3 | WBSE, FBE, ROM | NR | ||||
|
Kazemnejad et al. (36) (2023/Iran) |
Experimental group n = 10 (M) |
24.7 ± 4.24 | 12/3 | Ski Slalom, Ski Jump, Table Tilt, Table Tilt Plus, Tightrope Walk, Balance Bubble, Balance Bubble Plus, Penguin Slide, Snowboard Slalom, Skateboard Arena | bone-patellar tendon-bone graft | VAS, Knee flexion Range, Tigh Girth, knee effusion, BESS, MSEBT, SLHD, SLHT | Expert System | The Wii Fit group showed significant improvements in pain, knee swelling, thigh circumference, knee range of motion, static and dynamic balance, and single-leg jump symmetry indices compared with the control group (p < 0.05) |
|
Control group, n = 10 (M) |
24.4 ± 3.16 | 12/3 | Static exercises for quadriceps, hamstring, gluteal muscles, and SLR, CKC exercises (wall sit, mini squat, and leg press), HMSE, Proprioception exercises, Treadmill (Walk/Jog) | bone-patellar tendon-bone graft | ||||
|
Baltaci et al. (18) (2013/Turkey) |
Experimental group n = 15 (M) |
28.6 ± 6.8 | 12/3 | The bowling and skiing games in Wii Sports, Boxing, Football, Balance Board in Sports Pro Series | hamstring tendon graft | Coordination, proprioception, response time, Dynamic balance, Muscle strength | functional squat system, Isomed 2000 isokinetic dynamometer | No significant differences were observed in knee strength, dynamic balance, and squat performance between the two groups over 12 weeks |
|
Control group, n = 15 (M) |
29.3 ± 5.7 | 12/3 | CKC flexion exercises, Prone hanging exercise, SLR and isometric quadriceps, cycling, balance exercises, | hamstring tendon graft | ||||
AAROM: Active-assisted ROM exercises, BESS: Balance Error Scoring System, BPTB: bone-patellar tendon-bone, CKC: Closed kinetic chain, COG: center of gravity, FBE: Functional and balance exercises, HMSE: Hip muscles strengthening exercises, LEFS: Lower Extremity Functional Score, MSEBT: Modified STAR Excursion Balance Test, NR: Not reported, PKE: Passive knee extension, PRKFE: Progressive resistive knee flexion and extension, RKEFE: Resistive knee extension and flexion exercises, ROM: range of motion, SLB: Single leg balance, SLHD: Single-Leg Hop Distance, SLHT: Single-Leg Hop time, SLR: Straight leg rise, VAS: Visual Analog Scale, VR: Virtual reality, WBSE: Weight-bearing and strengthening exercises
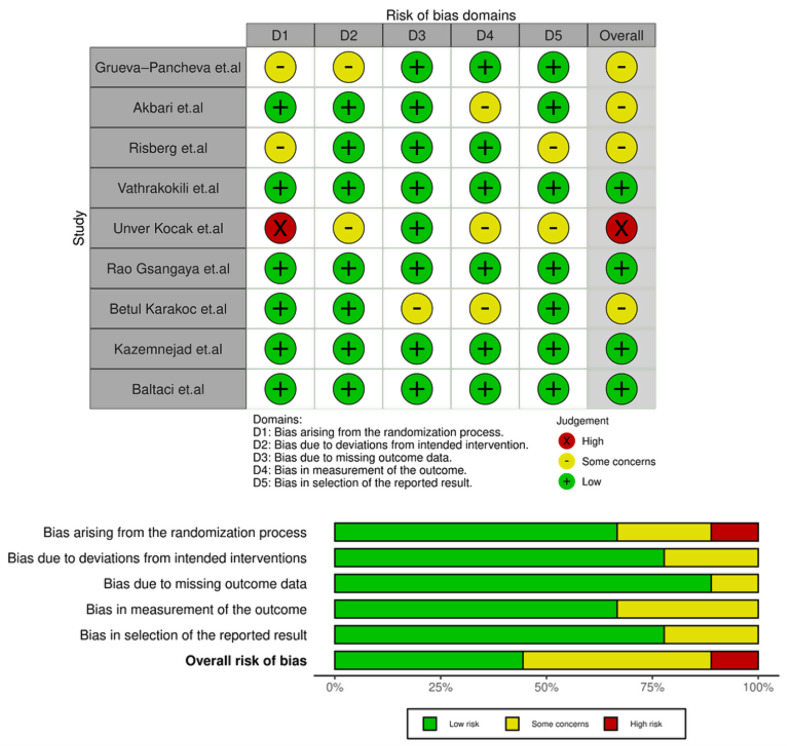
Risk of bias
The risk of bias across the studies is illustrated in Fig. 2. Of these, four study was identified with a low level of bias [18, 21, 33, 34], while four were assessed as having some concerns bias [9, 14, 35, 36]. Additionally, one studies were found to have high bias [13]. On the overall scale, 44% of studies had low risk bias, 44% had some concerns bias, 11% had high bias.
Fig. 2.
Analysis of risk of bias
Quality assessment
The average score of the studies reviewed was 7.1, with a range from 0 to 11, which suggests that they overall maintained good quality. However, a notable weakness across most studies was in their blinding methods. Specifically, only two studies implemented assessor blinding [9, 34], while two others employed therapist blinding [9, 18], and four utilized participants blinding [9, 18, 34, 36]. Among the studies analyzed, those conducted by Kazemnejad et al. and Arna Risberg et al. achieved the highest scores [9, 34]. Supplementary information is reported in Table 3.
Table 3.
PEDro scale
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grueva–Pancheva et al. (14) (2023) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Akbari et al. (33) (2026) | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Risberg et al. (9) (2007) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 |
| Vathrakokili et al. (34) (2008) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 5 |
| Unver Kocak et al. (13) (2010) | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Rao Gsangaya et al. (21) (2023) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Betul Karakoc et al. (35) (2018) | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 8 |
| Kazemnejad et al. (36) (2023) | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 10 |
| Baltaci et al. (18) (2012) | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 9 |
(1) Eligibility Criteria, (2) Random Allocation, (3) Concealed Allocation, (4) Groups Similar at Baseline, (5) Participant Blinding, (6) Therapist Blinding, (7) Assessor Blinding, (8) <15% Dropouts, (9) Intention-to-Treat Analysis, (10) Between-Group Difference Reported, 11. Point Estimate and Variability Reported. 1 = Yes, 0 = No
Quality assessment of the body of evidence
In section evaluated dynamic balance The studies in the first group of proprioception exercises had moderate certainty, the second group had very low certainty, the studies in the VR section had high certainty, and the studies that applied proprioception exercises and assessed static balance had low certainty using the GRADE criteria. Details are reported in Table 4.
Table 4.
Certainty of the evidence and summary of findings
| Meta-analysis | Risk of bias | Inconsistency | Indirectness | Imprecisionb | Publication bias | Quality of evidence |
|---|---|---|---|---|---|---|
| Dynamic balance score in proprioception exercise (Group 11) | Not Serious | Not Serious | Not Serious | Not Serious | Serious |
⊕⊕⊕○ Moderate |
| Dynamic balance score in proprioception exercise (Group 22) | Serious | Seriousa | Not Serious | Serious | N/A |
⊕○○○ Very low |
| Dynamic balance score in VR exercise | Not Serious | Not Serious | Not Serious | Not Serious | Not Serious |
⊕⊕⊕⊕ High |
| Static balance score in proprioception exercise | Serious | Not Serious | Not Serious | Not Serious | Serious |
⊕⊕○○ Low |
1: Biodex Balance System, 2: Kinesthetic Ability Trainer (KAT), a: The test for heterogeneity is significant, and the I2 is high, 97.72%. b: Criterion (95%CI), VR: Virtual Reality, N/A: Not applicable
Data synthesis
Dynamic balance (Proprioception)
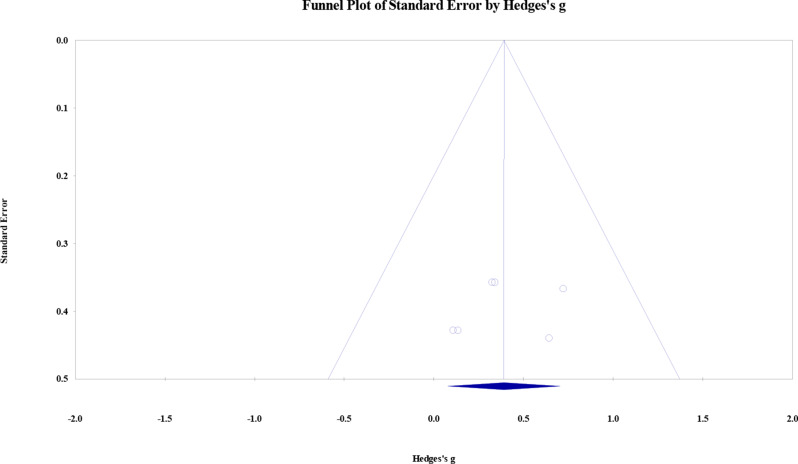
The meta-analysis findings indicated that proprioception exercise (Biodex - Group1) significantly enhanced dynamic balance among individuals with ACL-R. A fixed model was applied due to a low level I2 index (48.88%). Hedges` g effect size = 0.697; 95% of confidence interval = 0.429 to 0.969; Z = 5.018; p = 0.0001. Publication bias may be present based on lack of symmetry in the funnel plot concerning the studies at both ends of the Hedge’s g average index. In Fig. 4, it can be seen that the distribution of points is scattered and there is no symmetry. Two points are far from the center line of the funnel plot, which has a significant impact on the results and there is also a point outside the funnel plot. Furthermore, Begg test produced a p-value of 0.008, highlighting a notable indication of publication bias and implying an overall tendency of publication bias. Figure 3, and 4 show more information.
Fig. 4.
Funnel plot of the effects of proprioception exercise on dynamic balance
Fig. 3.
Dynamic balance score in proprioception exercise (Biodex– Group1)
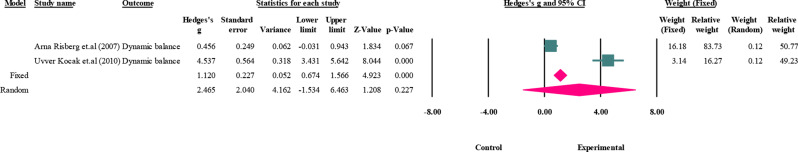
In this section the meta-analysis findings showed that proprioception exercise (KAT– Group2) failed to make a significant difference in dynamic balance among individual with ACL-R. A random model was applied due to a high level I2 index (97.72%) for dynamic balance Hedges` g effect size = 2.465; 95% of confidence interval=-1.534 to 6.463; Z = 1.208; p = 0.227. Furthermore, the comparison of results across studies in this area was no significant meaningful. Figure 5 show more information.
Fig. 5.
Dynamic balance score in proprioception exercise (KAT– Group2)
Dynamic balance (VR)
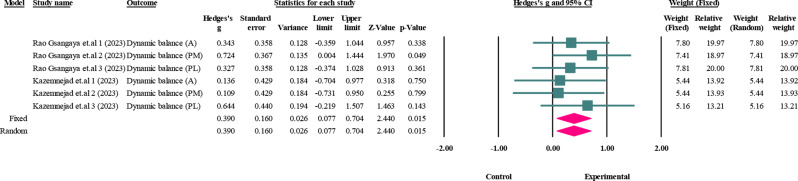
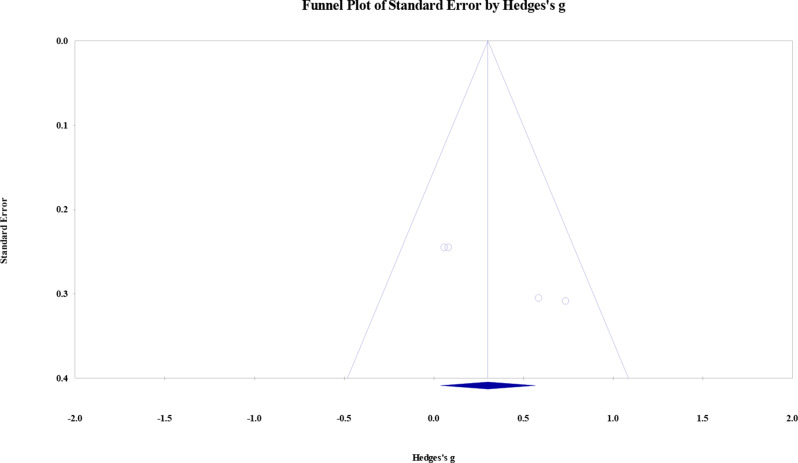
The meta-analysis findings showed that VR exercise significantly enhanced dynamic balance among individuals with ACL-R. A fixed model was applied due to a low level I2 index (0%). Hedges` g effect size = 0.390; 95% of confidence interval = 0.077 to 0.704; Z = 2.440; p = 0.015. The symmetry in the funnel plot concerning the studies at both ends of the Hedge’s g average index suggests that publication bias may not be present. In Fig. 7, it can be seen that the distribution of points is not scattered and there is symmetry. All six points are located under the funnel plot and are close to the center line. Furthermore, Begg test produced a p-value of 1.0, there is no significant indication of publication, suggesting an overall lack of publication bias. Figure 6, and 7 show more information.
Fig. 7.
Funnel plot of the effects of VR exercise on dynamic balance
Fig. 6.
Dynamic balance score in VR exercise
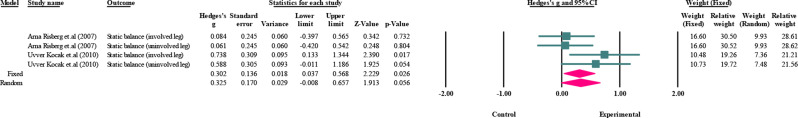
Static balance (Proprioception)
The meta-analysis findings showed that proprioception exercise significantly enhanced static balance among individuals with ACL-R. A fixed model was applied due to a low level I2 index (35.11%). Hedges` g effect size = 0.302; 95% of confidence interval = 0.037 to 0.568; Z = 2.229; p = 0.026. The lack of symmetry in the funnel plot concerning the studies at both ends of the Hedge’s g average index suggests that publication bias may be present. In Fig. 9, it can be seen that the distribution of points is not very scattered and there is relative symmetry. All 4 points are located under the funnel plot and are almost close to the center line. Furthermore, Begg test produced a p-value of 0.08, highlighting a notable indication of publication bias and implying an overall tendency of publication bias. Figure 8, and 9 show more information.
Fig. 9.
Funnel plot of the effects of proprioception exercise on static balance
Fig. 8.
Static balance score in proprioception exercise
Discussion
The purpose of this systematic review and meta-analysis was to compare the impacts of proprioceptive and VR exercise on postural balance in individuals with ACL-R.
Effect of the proprioception exercise on postural balance
The meta-analysis conducted in the dynamic balance (Proprioception) section showed that the exercises were effective in group 1 (p = 0.0001), but in group 2, there was no significant effect of the exercises (p = 0.227). On the other hand, the effect size in group 1 was moderate and in group 2, it was high. In group 1, the largest effect size among the studies was the study by Vathrakokili et al. (1.671) [33], and in group 2, by Unver Kocak et al. (4.534) [13]. The funnel plot also showed that the study results are influenced by several factors. In addition, the bias scale scores indicate that the results of these studies are somewhat reliable and generalizable to the target population. In the static balance section, the effect of exercise was significant (p = 0.026), and the final effect size was small as well. The reported funnel plot demonstrates that there is no observable bias in the results of the studies.
The heterogeneity between studies in Group 2 may be due to differences in exercise duration, with the exercises in the Arna Risberg et al. study lasting 24 weeks and the exercises in the Unver kocak et al. study lasting 12 weeks, showing a twofold difference between the two studies. On the other hand, the number of subjects and the difference between the number of male and female subjects in group 2 of studies may account for the heterogeneity.
In the study by Akbari, and Arna Risberg no significant effect on dynamic balance was observed [8, 35]. The effect size of these studies was also small. The reasons for such a result could be the difference in the duration of the exercise week, which in the study by Akbari et al., was only 2 weeks and consisted of 12 sessions [35]. On the other hand, the intensity of the training and the lack of appropriate intervals between exercise days may have caused such a result.
Beyond the duration, the type and intensity of proprioceptive exercises also exhibited substantial heterogeneity. Some studies utilized basic exercises like single-leg standing and step-ups (Akbari et al.), while others implemented more comprehensive protocols incorporating plyometric exercises, agility drills (Risberg et al.), or the use of specialized equipment such as hemispherical or cylindrical balance boards (Vetrano et al.). It seems that the greater complexity and intensity of exercises in studies like Risberg’s or Vetrano’s were associated with more positive results, although exercise intensity was not quantitatively reported in all studies. This diversity in the type and duration of training makes direct comparisons of intervention effectiveness challenging and contributes to the heterogeneity in the overall findings.
These findings are partially consistent with the results of a systematic review by Cooper et al. (2005), which found limited evidence for improved outcomes with balance and proprioceptive exercises in individuals with ACL injury, particularly those with ACL deficiency [10]. However, they noted a scarcity of research regarding the effectiveness of such exercises following ACL reconstruction. Similarly, a systematic review by Costa et al. (2020) did not find sufficient scientific evidence to definitively establish the positive impact of proprioceptive exercises after ACL reconstruction, citing a lack of studies, inconsistent findings, and heterogeneity in protocols and assessments [16].
Proprioception refers to integrating sensory information to maintain awareness of the joints of position and different parts of the body. Afferent neural input from this sense is essential for daily activities as well as athletic performance [33, 37]. Injury to the ACL not only Causalities mechanical instability but also Results in functional impairment in the form of decreased proprioception of the knee joint. Decreased function and changes in proprioception of the knee joint are associated with ACL tears [38]. Individuals after ACL-R show slower reactions during postural activities [18, 39]. The impact of this reconstruction is not limited to mechanical or positional aspects of the joint, but its effects are increased in challenging postural movements and affect the ability of the individual to react quickly after surgery. This decrease in postural reactions does have a significant impact on other biomechanical and neuromuscular aspects. The slowing of step responses in individuals who have undergone ACL-R surgery suggests a more complex neural response in which the individual prefers stability over mobility [40]. ACL injury commonly occurs during athletic activities and can result in pain, instability, and decreased range of motion (ROM) of the knee [21]. This in turn causes changes in balance, decreased strength, and increased stress on the injured knee. Returning a patient to a competitive level of play is highly dependent on the rehabilitation process. Rehabilitation after ACL surgery presents unique challenges due to the long recovery period and repetitive and tiring exercises, which can also lead to problems with adaptation and psychological aspects of the patients [18, 21, 36]. Therefore, to reduce the risk of reinjury in individuals who have undergone reconstruction, it is essential to evaluate new and clinically relevant rehabilitation exercise interventions to improve lower limb movement patterns and restore physical function before returning to full athletic activity [5]. Proprioception exercise is one of the rehabilitation methods for this group of individuals [13, 14]. These exercises, with their characteristics of enhancing the JPS and body position within the range of support, help reduce body sway and ultimately improve postural balance [9, 13, 14, 33, 35]. The presence of Raffini and Pacinian cells, Golgi tendon organs, and free nerve endings in the ACL indicate the importance of proprioceptive mechanoreceptors in the knee [41]. Athletes who have undergone ACL-R surgery often have impaired knee proprioception in the injured limb, even after the end of the rehabilitation period [9]. These sensory deficits can lead to changes in postural stability and lower limb movement control. Several factors, including quadriceps muscle activity, decreased strength, decreased electromagnetic activity of the vastus medialis and vastus lateralis muscles, and increased tendinous muscle stiffness, affect knee function after ACL-R relative to the injured limb [42]. Input from the sensorimotor system, which is altered due to the ACL tear and the reduction in the number of deep mechanoreceptors, may cause changes in movement patterns and weakness in the quadriceps and hamstrings [43]. Proprioception alone can help increase isokinetic strength. Also, recovery and strengthening of the quadriceps muscles are essential to maximize the function of the operated knee joint. Rehabilitation is of great importance to strengthen muscle responses, especially in the field of proprioception exercises [9].
Using proprioception exercises by stimulating deep receptors, over time, creates a suitable adaptation for improving stability and balance in the joint [13]. The stability created in critical and different situations helps the person a lot and prevents injury [14].
On the other hand, proprioception exercises affect the somatosensory system [14, 35]. The changes that occur in this system at the level of the central nervous system (CNS) cause a difference compared to the state before exercise [35]. Exercise can cause the individual to react more appropriately at the involuntary level and to achieve improvement at the subcortical level [9, 14].
Among patients with ACL injury, proprioception in the normal knee of the opposite side is less than in healthy people [9]. Proprioception exercises of the ACL-injured limb can help improve stability, even if the reflex arc and mechanical stability are reduced, and this is probably due to the effect on the subcortical processing of feedback signals [9, 13, 33]. Similarly, proprioception exercise in the contralateral limb may also help improve stability in the injured limb [38]. Athletes have high expectations for return to athletic activities after ACL-R surgery. For this reason, the use of neuromodulatory interventions; as well as the creation of a rehabilitation environment that includes sensory and cognitive stimulation for movement tasks; and consideration of psychological, and contextual factors are critical and key factors for achieving successful recovery after ACL-R [44]. To avert severe consequences of ACL injury, conventional rehabilitation programs that focus on muscle strengthening, increasing ROM, and correcting biomechanical aspects may not be sufficient alone to reduce the risk of re-injury and return to athletic or physical activities. These programs usually do not address the sensory-motor changes and impairments that occur after ACL injury and repair and have not been very successful in addressing neuroplastic changes in the central nervous system and psychological factors such as anxiety regarding re-injury [45]. After injury, the remnants of the ACL contain proprioceptive fibers that can help improve function if they attach or grow into the repaired ligament [46]. Sensory and motor deficits may remain in the knee [46]. This condition, which is likely caused by a lack of proprioceptive feedback, can lead to a decrease in the patient’s activity level and performance. Therefore, the use of proprioceptive exercises can be a good option to adequately address the deficits and ultimately help improve the individual’s performance [9, 13, 14, 35, 44].
The ACL not only plays a mechanical role by restricting passive knee movement but also plays a sensory function through mechanoreceptors deep within its tissue, that interact with the neuromuscular system to provide proprioceptive feedback [9]. After ACL-R, a person’s proprioceptive abilities are impaired [14]. A decrease in static and dynamic postural balance is observed between the operated and non-operated legs [9, 33]. Participants with ACL injuries have poorer proprioception than individuals without such injuries [47]. The effectiveness of proprioception exercises in ACL injury rehabilitation, including exercises such as calf/foot raises, squats, steps, lunges, figure-8, wobble board exercises, and single-leg standing, has been demonstrated [48]. Proprioceptive exercises should be part of the rehabilitation program after ACL-R surgery and can help improve postural balance indices in the early stages of the process. In addition, proprioception exercises play a very important role in preventing knee injuries [13, 14].
Proprioception exercise may be more acceptable and performed in situations where the injury is more severe because the patient needs to focus on a specific movement or when the exercises need to be performed without additional stimulation. If people experience headaches or other such problems when exposed to VR, proprioception exercise is welcomed between the two methods.
Effect of the VR exercise on postural balance
The results of the meta-analysis show that exercises have a significant effect on the desired variable (p = 0.015), but the effect size of these exercises is small. The largest effect size was related to the study by Rao Gsangaya et al., which showed a moderate effect [21]. This finding, indicating the enhancement of balance through VR training, aligns with the results of a systematic review and meta-analysis conducted by Cortés-Pérez et al. (2025). Their work demonstrated the effectiveness of VR-based balance training (VRBT) in improving dynamic balance, specifically posterior-medial and posterior-lateral displacement of the center of pressure, following ACL injury [20]. In addition, the funnel plot showed that bias was not observed in the research results. In the study by Kazemnejad et al., no significant effect was observed [34]. This could be because, in this study, the number of exercise sessions was few and the exercises were performed in 12 sessions. On the other hand, the average BMI of the subjects in this study was in the overweight range.
Specific rehabilitation protocols after an ACL injury can vary greatly. Therefore, whether the injury is managed surgically or nonsurgically, strengthening the quadriceps and returning to full ROM is among the main goals of rehabilitation [18, 21, 36]. These not only help improve function but also prevent future injuries. One training method that has received attention in recent years in various studies is rehabilitation using VR exercises [18]. These exercises refer to the use of digital technologies to simulate real-world environments and create interactive experiences, and these types of exercises can include movement games, sports simulations, and challenging activities that are specifically designed to improve balance and postural control [18, 34]. Therefore, there is great interest in using new rehabilitation methods, especially VR, for these individuals [34]. However, it should be noted that the negative effects of this process should also be examined, and both conditions should be weighed to determine whether the benefits outweigh the risks.
VR and game-based training can be used as effective tools in the delivery of rehabilitation interventions after lower limb surgeries [22]. The application of VR technology in the context of clinical rehabilitation can have a significant impact on knee biomechanics and motor learning ability [21]. This technology may help change movement patterns after ACL-R and potentially reduce the risk of ACL re-injury [49]. The findings reported by Cortés-Pérez et al. (2025) further corroborate that VR-based balance training (VRBT) facilitates the improvement of movement patterns following ACL injury [20]. This technology can increase patient motivation and improve the learning experience. It may also create better psychological readiness for exercise training [22, 49].
VR exercise can help improve the central nervous system’s ability to learn motor skills. This is because VR comprehensively simulates real-world scenarios through applications and shifts the patient’s attention from the knees to interacting with the VR environment [21]. VR exercise-based rehabilitation is recognized as an effective adjunct to physiotherapy, being incorporated into rehabilitation programs due to its ability to reduce pain and help improve strength, and dynamic balance after injury [20].
In the rehabilitation process after ACL-R surgery and balance exercises for the lower extremities, the use of VR can help improve knee joint function, strengthen lower limb muscles, increase proprioception, and manage pain, and Also, the level of participation may affect rehabilitation outcomes [18, 34].
While the review by Du et al. (2025) suggests the potential benefits of virtual reality for knee function, muscle strength, proprioception, and pain (albeit with a low level of evidence) [1], the meta-analysis conducted by Cortés-Pérez et al. (2024) found no significant difference in proprioceptive improvement with VR-based balance training (VRBT) [20].
When people undergo ACL reconstruction, they often experience an imbalance in leg muscle strength. This imbalance, where one leg is significantly weaker than the other, can make it more difficult for them to maintain good balance while moving [50]. Gsangaya et al. have seen that even after regular physical therapy, people often have a noticeable difference in how strong their legs are– about 6%. But when we used virtual reality to help with their exercises, that difference improved, going down to roughly 5% [21]. Basically, VR rehab exercises could lower the chance of cartilage damage by helping your joints move more evenly and reducing stress on them [51]. With traditional rehab, the exercises mostly target the leg that had surgery. This might actually make the difference in strength between your legs bigger while you’re recovering [52]. But with virtual reality exercises, people get completely drawn into the game or activity, so they naturally use both legs [21]. One more thing that made VR training better than regular rehab was how quickly people could react. This means people were able to respond more quickly to unexpected situations they encountered while healing [18]. When you can react faster, it helps your knee stay steady. This is really crucial after ACL reconstruction, since the knee joint can be less stable [53]. Pain is a frequent issue following ACL reconstruction surgery, and unfortunately, it can linger for months. This persistent pain can trigger a chain reaction, leading to your muscles not activating properly, muscle loss, and a decrease in your knee’s ability to move [54]. Several factors play into how much pain someone experiences after surgery. These include psychological factors and the duration of their post-operative recovery [55]. A small study found that using virtual reality, guided by a smart computer system, helped people feel less pain compared to regular rehab [34].
Research has shown that patients may become tired of repetitive exercises in rehabilitation programs and therefore enjoy VR balance games, which are being developed with the advancement of technology. Patients reported that they actively participated in the games and found them enjoyable, without feeling tired. Accordingly, the use of VR games is easy. It can be suitable for improving balance and symmetrical weight bearing in the rehabilitation of people with different injuries [36]. Baltchi et al. stated that Wii Fit activities as a rehabilitation method can help improve physiotherapy goals including visual-perceptual processing, coordination, proprioception, and functional mobility [18]. Therefore, they consider its use effective for people with a history of ACL-R.
VR exercise, due to the greater interaction of the person with the environment and the additional stimulation it provides for the person, causes greater motivation to adhere to it. This leads to deeper experiences. On the other hand, access to these technologies is not possible for everyone and the conditions for performing it are not available in some positions.
Limitation
No trials were reported on adherence to unsupervised exercises. Without quantifying the actual amount of exercise performed, it is challenging to ascertain whether the positive outcomes observed stemmed from the exercises themselves or the volume of exercise undertaken. This uncertainty may lead to over- or underestimation of the true effectiveness of exercises, thereby reducing the reliability of conclusions about the effectiveness of interventions. To clarify the significance of adherence, future trials should investigate the relationship between adherence to home exercises and patient outcomes. Utilizing a digital exercise diary could facilitate the accurate assessment of adherence levels. The timing of rehabilitation initiation varied across studies, potentially influencing improvements in knee function and proprioception. Studies that commenced rehabilitation later may have missed capturing rapid initial improvements, possibly resulting in an underestimation of exercise effectiveness in the early phases compared to studies that initiated rehabilitation earlier. Therefore, more research is necessary to provide conclusive evidence on this matter. The studies included in this review employed different instruments and measures to evaluate outcomes. This variability complicates direct comparisons between study results and may hinder the ability to pool data in meta-analyses. Such heterogeneity can introduce measurement error and increase uncertainty in the overall interpretation of findings. Another limitation is the absence of cost estimates for VR rehabilitation in the studies. Given the expenses associated with VR equipment and the need to consider the target population, accurate cost assessments and comparisons with traditional rehabilitation methods are crucial for determining the cost-effectiveness of this treatment.
Conclusion
The results showed that the use of proprioception and VR exercises is effective in improving balance in athletes who have undergone ACL-R. According to the available evidence, the use of VR exercises seems to be more effective due to the simulation of real environments in exercise conditions and the simultaneous use of games and sports. In proprioception exercises, the results should be interpreted and evaluated with caution due to the observed bias. Therefore, to determine the results more accurately, higher-quality studies and systematic reviews are required in the future. The use of VR exercises can be recommended to sports coaches and physicians. It is recommended that future research focus on several key areas: combined interventions that integrate both proprioception and VR exercise, the utilization of digital tools to monitor adherence to training protocols, and comparative studies examining the effects of different VR devices on training outcomes. Also, the quality of future studies should be improved so that the evidence is more reliable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Author contributions
All authors contributed equally to the preparation of this manuscript.
Funding
The author(s) received no specific funding for this work.
Data availability
The datasets available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Du C, Gu N-M, Guo T-C, Liu A-F. Efficacy of virtual reality balance training on rehabilitation outcomes following anterior cruciate ligament reconstruction: A systematic review and meta-analysis. PLoS ONE. 2025;20(1):e0316400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. 2019;33(1):33–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang Z, Cui J, Zhong M, Deng Z, Chen K, Zhu W. Risk factors of cartilage lesion after anterior cruciate ligament reconstruction. Front Cell Dev Biology. 2022;10:935795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kotsifaki R, Korakakis V, King E, Barbosa O, Maree D, Pantouveris M, et al. Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. Br J Sports Med. 2023;57(9):500–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Queen RM, Peebles AT, Miller TK, Savla J, Ollendick T, Messier SP, et al. Reduction of risk factors for ACL re-injuries using an innovative biofeedback approach: rationale and design. Contemp Clin Trials Commun. 2021;22:100769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Negahban H, Mazaheri M, Kingma I, van Dieën JH. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22:1491–504. [DOI] [PubMed] [Google Scholar]
- 7.Howells BE, Clark RA, Ardern CL, Bryant AL, Feller JA, Whitehead TS, et al. The assessment of postural control and the influence of a secondary task in people with anterior cruciate ligament reconstructed knees using a nintendo wii balance board. Br J Sports Med. 2013;47(14):914–9. [DOI] [PubMed] [Google Scholar]
- 8.Risberg MA, Lewek M, Snyder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Phys Ther Sport. 2004;5(3):125–45. [Google Scholar]
- 9.Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87(6):737–50. [DOI] [PubMed] [Google Scholar]
- 10.Cooper R, Taylor N, Feller J. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res Sports Med. 2005;13(2):163–78. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clinical orthopaedics and related research (1976–2007). 2002;402:76–94. [DOI] [PubMed]
- 12.Saka T. Principles of postoperative anterior cruciate ligament rehabilitation. World J Orthop. 2014;5(4):450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocak FU, Ulkar B, Özkan F. Effect of proprioceptive rehabilitation on postural control following anterior cruciate ligament reconstruction. J Phys Therapy Sci. 2010;22(2):195–202. [Google Scholar]
- 14.Grueva–Pancheva T, Stambolieva K. Effectiveness of early onset of rehabilitation on the postural stability after anterior cruciate ligament reconstruction. J Bodyw Mov Ther. 2023;35:43–8. [DOI] [PubMed] [Google Scholar]
- 15.Jiang L, Zhang L, Huang W, Zeng Q, Huang G. The effect of proprioception training on knee kinematics after anterior cruciate ligament reconstruction: A randomized control trial. J Back Musculoskelet Rehabil. 2022;35(5):1085–95. [DOI] [PubMed] [Google Scholar]
- 16.Costa WDS, Guilherme VR, Rinaldi W, Alexandrino EG, Santos SRd, Guilherme FR. Effects of inclusion of proprioception training in the recovery of adults submitted to anterior cruciate ligament reconstruction surgery: a systematic review. J Phys Educ. 2020;31:e3134. [Google Scholar]
- 17.Peng L, Zeng Y, Wu Y, Si H, Shen B. Virtual reality-based rehabilitation in patients following total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Chin Med J. 2022;135(02):153–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baltaci G, Harput G, Haksever B, Ulusoy B, Ozer H. Comparison between nintendo wii fit and conventional rehabilitation on functional performance outcomes after hamstring anterior cruciate ligament reconstruction: prospective, randomized, controlled, double-blind clinical trial. Knee Surg Sports Traumatol Arthrosc. 2013;21:880–7. [DOI] [PubMed] [Google Scholar]
- 19.Gumaa M, Rehan Youssef A. Is virtual reality effective in orthopedic rehabilitation? A systematic review and meta-analysis. Phys Ther. 2019;99(10):1304–25. [DOI] [PubMed] [Google Scholar]
- 20.Cortés-Pérez I, Desdentado‐Guillem JM, Camacho‐Delgado MS, del Rocío Ibancos‐Losada M, Obrero‐Gaitán E, Lomas‐Vega R. Virtual reality‐based therapy after anterior cruciate ligament injury effectively reduces pain and improves knee function, movement patterns, and dynamic balance: A systematic review and meta‐analysis. Arthroscopy: Knee Surgery, Sports Traumatology; 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gsangaya MR, Htwe O, Naicker AS, Yusoff BAHM, Mohammad N, Soh EZF, et al. Comparison between the effect of immersive virtual reality training versus conventional rehabilitation on limb loading and functional outcomes in patients after anterior cruciate ligament reconstruction: A prospective randomized controlled trial. Asia-Pacific J Sports Med Arthrosc Rehabilitation Technol. 2023;34:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thakur A, Rishi P, Sivach P. The effectiveness of virtual Reality-Based rehabilitation versus conventional methods in enhancing functional outcomes for Post‐Operative lower limb patients: A systematic review. Musculoskelet Care. 2025;23(1):e70061. [DOI] [PubMed] [Google Scholar]
- 23.Soltanabadi S, Minoonejad H, Bayattork M, Seyedahmadi M. Effect of virtual reality and augmented reality training for injury prevention and accelerating rehabilitation of anterior cruciate ligament injury in athletes: A scoping review. Asian J Sports Med. 2023;14(4).
- 24.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. [DOI] [PMC free article] [PubMed]
- 25.Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366. [DOI] [PubMed]
- 26.Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the physiotherapy evidence database (PEDro). Australian J Physiotherapy. 2002;48(1):43–9. [DOI] [PubMed] [Google Scholar]
- 27.Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. [DOI] [PubMed] [Google Scholar]
- 28.Michael H. The power functions of begg’s and egger’s tests for publication bias. Stat Neerl. 2025;79(1):e12364. [Google Scholar]
- 29.Jpt H. Cochrane handbook for systematic reviews of interventions.http://www.training.cochrane.org/handbook.
- 30.Becker LA. Effect size (ES). 2000.
- 31.Montgomery PG, Pyne DB, Minahan CL. The physical and physiological demands of basketball training and competition. Int J Sports Physiol Perform. 2010;5(1):75–86. [DOI] [PubMed] [Google Scholar]
- 32.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis: Wiley; 2021.
- 33.Vathrakokilis K, Malliou P, Gioftsidou A, Beneka A, Godolias G. Effects of a balance training protocol on knee joint proprioception after anterior cruciate ligament reconstruction. J Back Musculoskelet Rehabil. 2008;21(4):233–7. [Google Scholar]
- 34.Kazemnejad A, Asosheh A, Moezy A, Abasi A. Therapy-based expert system on function and postural stability after anterior cruciate ligament reconstruction: a pilot study. BMC Musculoskelet Disord. 2023;24(1):617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Akbari A, Ghiasi F, Mir M, Hosseinifar M. The effects of balance training on static and dynamic postural stability indices after acute ACL reconstruction. Global J Health Sci. 2015;8(4):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karakoc ZB, Colak TK, Sari Z, Polat MG. The effect of virtual rehabilitation added to an accelerated rehabilitation program after anterior cruciate ligament reconstruction: a randomized controlled trial. Clin Experimental Health Sci. 2019;9(2):124–9. [Google Scholar]
- 37.Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: a critical review of methods. J Sport Health Sci. 2016;5(1):80–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim H-J, Lee J-H, Lee D-H. Proprioception in patients with anterior cruciate ligament tears: a meta-analysis comparing injured and uninjured limbs. Am J Sports Med. 2017;45(12):2916–22. [DOI] [PubMed] [Google Scholar]
- 39.Gokeler A, Benjaminse A, Van Eck C, Webster K, Schot L, Otten E. Return of normal gait as an outcome measurement in acl reconstructed patients. A systematic review. Int J Sports Phys Therapy. 2013;8(4):441. [PMC free article] [PubMed] [Google Scholar]
- 40.Armitano-Lago CN, Morrison S, Hoch JM, Bennett HJ, Russell DM. Anterior cruciate ligament reconstructed individuals demonstrate slower reactions during a dynamic postural task. Scand J Med Sci Sports. 2020;30(8):1518–28. [DOI] [PubMed] [Google Scholar]
- 41.Gao F, Zhou J, He C, Ding J, Lou Z, Xie Q, et al. A morphologic and quantitative study of mechanoreceptors in the remnant stump of the human anterior cruciate ligament. Arthroscopy: J Arthroscopic Relat Surg. 2016;32(2):273–80. [DOI] [PubMed] [Google Scholar]
- 42.Busch A, Blasimann A, Henle P, Baur H. Neuromuscular activity during stair descent in ACL reconstructed patients: a pilot study. Knee. 2019;26(2):310–6. [DOI] [PubMed] [Google Scholar]
- 43.Trulsson A, Miller M, Hansson G-Å, Gummesson C, Garwicz M. Altered movement patterns and muscular activity during single and double leg squats in individuals with anterior cruciate ligament injury. BMC Musculoskelet Disord. 2015;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vutescu ES, Orman S, Garcia-Lopez E, Lau J, Gage A, Cruz AI Jr. Psychological and social components of recovery following anterior cruciate ligament reconstruction in young athletes: a narrative review. Int J Environ Res Public Health. 2021;18(17):9267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.LaCombe YK. Exploring the therapeutic effects of tDCS and proprioceptive training on knee proprioception in anterior cruciate ligament reconstructed population. New Mexico State University; 2023.
- 46.Kosy JD, Mandalia VI. Anterior cruciate ligament mechanoreceptors and their potential importance in remnant-preserving reconstruction: a review of basic science and clinical findings. J Knee Surg. 2018;31(08):736–46. [DOI] [PubMed] [Google Scholar]
- 47.Bąkowski P, Ciemniewska-Gorzela K, Bąkowska-Żywicka K, Stołowski Ł, Piontek T. Similar outcomes and satisfaction of the proprioceptive versus standard training on the knee function and proprioception, following the anterior cruciate ligament reconstruction. Appl Sci. 2021;11(8):3494. [Google Scholar]
- 48.Saha S, Adhya B, Dhillon M, Saini A. A study on the role of proprioceptive training in non operative ACL injury rehabilitation. Quadriceps Femoris Strength Train Eff Neuromuscul Electr Stimul Isometric Exerc Osteoarthr Knee. 2015;9:3232. [Google Scholar]
- 49.Gokeler A, Bisschop M, Myer GD, Benjaminse A, Dijkstra PU, Van Keeken HG, et al. Immersive virtual reality improves movement patterns in patients after ACL reconstruction: implications for enhanced criteria-based return-to-sport rehabilitation. Volume 24. Arthroscopy: Knee Surgery, Sports Traumatology; 2016. pp. 2280–6. [DOI] [PubMed] [Google Scholar]
- 50.Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry following ACL reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015;43(7):1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. JOSPT, Inc. JOSPT, 1033 North Fairfax Street, Suite 304, Alexandria,VA… pp. 374-6. [DOI] [PubMed]
- 52.Labanca L, Laudani L, Menotti F, Rocchi J, Mariani PP, Giombini A, et al. Asymmetrical lower extremity loading early after anterior cruciate ligament reconstruction is a significant predictor of asymmetrical loading at the time of return to sport. Am J Phys Med Rehabil. 2016;95(4):248–55. [DOI] [PubMed] [Google Scholar]
- 53.SM L. Proprioception and neuromuscular control in joint stability. Hum Kinetics. 2000:405–13.
- 54.Baranoff J, Hanrahan SJ, Connor JP. The roles of acceptance and catastrophizing in rehabilitation following anterior cruciate ligament reconstruction. J Sci Med Sport. 2015;18(3):250–4. [DOI] [PubMed] [Google Scholar]
- 55.Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. JAAOS-Journal Am Acad Orthop Surg. 2015;23(8):501–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets available from the corresponding author on reasonable request.