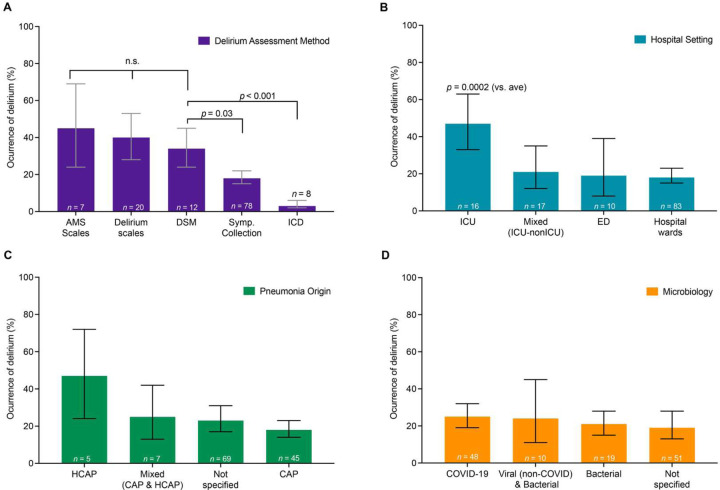
Figure 3.
Delirium rates differ based on assessment methods and are higher in studies performed in intensive care units, but do not differ based on pneumonia origin or microbiological etiology.
A. Delirium rates varied significantly according to the assessment method used, which explained 37% of variance in delirium rates across studies (R2 = 36.8%, p<0 .0001). Given that the Diagnostic and Statistical Manual (DSM) assessment is considered the gold standard for delirium assessment, we compared delirium rates to those of the DSM. Delirium rates were similar to the DSM assessment for standardized assessments of mental status (AMS Scales, such as Glasgow Coma Scale or Richmond Agitation Sedation Scale, p=0.73) or validated Delirium scales (such as CAM, CAM-ICU, ICSDC, 4AT, see abbreviations in Supplementary eMethods, p=0.73). In contrast, rates of delirium were lower when assessed using nonstructured symptom assessments (i.e., symptom collection, p=0.03) or ICD codes (p<0.001). Symp. Collection = symptom collection: identification of relevant symptoms, e.g. chart report of altered mental status. Each bar represents a meta-analytic estimate of delirium rates, with the calculated 95% confidence interval. Post-hoc p-values in all panels are adjusted for multiple comparisons (Holm). Forest plots of all studies with n’s, meta-analytic proportion, CI, and heterogeneity measures for each subgroup analysis are provided in supplementary material (Supplementary Figure S4).
B. Delirium rates varied significantly according to study setting, which explained 12% of variance in delirium rates across studies (R2 12.1%, p=0.002). Compared to the average of all studies, delirium rates were significantly higher for studies performed in the ICU (p=0.0002). (ICU = Intensive Care Unit, ED = Emergency Department). Conventions as in A, with forest plots in Supplementary Figure S5).
C. Delirium rates did not vary significantly according to pneumonia origin, which explained only 2.4% of variance in delirium rates across studies (R2 = 2.4%, p=0.15). (HCAP=Healthcare Acquired Pneumonia, CAP=Community Acquired Pneumonia). Conventions as in A, with forest plots in Supplementary Figure S6).
D. Delirium rates did not vary significantly according to microbiological etiologies, which explained 0.0% of variance in delirium rates across studies (R2 = 0.0%, p=0.63). Conventions as in A, with forest plots in Supplementary Figure S7).