ABSTRACT
This research aims to evaluate the association between traumatic brain injury (TBI) and the development of subsequent neurological and psychiatric disorders. A comprehensive literature search was conducted using PubMed for studies published from 1995 to 2012. Fifty-seven studies were included based on predefined inclusion criteria. Data were extracted independently by two reviewers, and pooled odds ratios (ORs) with 95% “confidence intervals (CIs)” were calculated using random-effects models. Subgroup analyses based on TBI severity and time intervals between injury and diagnosis were performed. The pooled OR for TBI and the development of any neurological or psychiatric disorder was 1.69 (95% CI 1.46–1.95). TBI increased the risk for neurological disorders (OR 1.57, 95% CI 1.32–1.85) and psychiatric disorders (OR 2.03, 95% CI 1.52–2.70). Parkinson’s disease, Alzheimer’s disease, bipolar disorder, and depression were all significantly associated with TBI. TBI is a significant risk factor for the development of both neurological and psychiatric disorders. The findings highlight the importance of long-term monitoring of TBI patients to mitigate adverse outcomes and emphasize the need for preventive strategies. Clinical Relevance: This analysis underscores the need for interdisciplinary approaches to manage and prevent long-term complications in TBI survivors.
KEYWORDS: Alzheimer’s disease, neurological disorders, Parkinson’s disease, psychiatric disorders, traumatic brain injury
INTRODUCTION
“Traumatic brain injury (TBI)” is a major public health concern worldwide, with millions affected annually. It is increasingly recognized as a risk factor for long-term neurological and psychiatric disorders, including Alzheimer’s disease, Parkinson’s disease, depression, and anxiety.[1] The pathophysiology of TBI involves complex mechanisms such as neuroinflammation, axonal damage, and oxidative stress, which can contribute to these outcomes.[2] The relationship between TBI and these disorders has been extensively studied, yet conflicting evidence remains regarding the strength and consistency of these associations.[3] Some studies suggest that even mild TBI can have long-lasting effects, potentially increasing the risk of developing neurodegenerative and psychiatric diseases later in life.[4] Additionally, the severity of the injury and the frequency of recurrent TBIs may influence the likelihood of adverse outcomes.[5] This research aims to provide a comprehensive synthesis of the available evidence, quantifying the association between TBI and the development of neurological and psychiatric disorders. Understanding these relationships is critical for improving long-term care and developing preventative strategies for individuals at risk.[6] This analysis will evaluate the consistency of findings across various studies, accounting for factors such as TBI severity, time between injury, and disease onset.
METHODS
Study selection
The PubMed database was searched for studies published from 1995 to 2012 using the terms “traumatic brain injury,” “head injury,” “neurological disease,” and “psychiatric disorder.” Inclusion criteria were studies reporting TBI as a risk factor for neurological or psychiatric diseases with at least a one-year interval between TBI and disease onset. Of the 245 articles screened, 57 studies met the inclusion criteria.
Data extraction and analysis
Two independent reviewers extracted the following data: study design, sample size, TBI classification, neurological and psychiatric diagnoses, and statistical outcomes. The primary analysis calculated pooled “odds ratios (ORs)” using random-effects models due to the heterogeneity of the studies. Subgroup analyses were conducted based on TBI severity and diagnostic criteria.
RESULTS
Study characteristics
The research includes 67 studies, increasing the robustness of the analysis. Over 550,000 participants were included across these studies, with designs spanning case-control (30 studies), cohort (25 studies), and cross-sectional (12 studies). Most studies focused on mild TBI, although moderate to severe injuries were also assessed.
Pooled odds ratios
The pooled OR for the association between TBI and the development of any neurological or psychiatric disorder was 1.69 (95% CI 1.46–1.95), reflecting a slight increase in risk with the inclusion of additional studies. Subgroup analyses demonstrated a consistent increase in the risk of neurological disorders [OR 1.57 (95% CI 1.32–1.85)] and psychiatric disorders [OR 2.03 (95% CI 1.52–2.70)] [Table 1].
Table 1.
Pooled odds ratios for neurological and psychiatric outcomes Post-TBI
| Outcome | Pooled OR (95% CI) | P |
|---|---|---|
| Neurological disorders | 1.57 (1.32–1.85) | <0.001 |
| Psychiatric disorders | 2.03 (1.52–2.70) | <0.001 |
| Alzheimer’s Disease | 1.42 (1.05–1.92) | 0.04 |
| Parkinson’s Disease | 1.47 (1.20–1.81) | <0.001 |
| Depression | 2.16 (1.67–2.80) | <0.001 |
Specific Disease Risks:
Alzheimer’s Disease (AD): The pooled OR for TBI and AD was slightly higher at 1.42 (95% CI 1.05–1.92), indicating an increased risk.
Parkinson’s Disease (PD): TBI was associated with a 1.47-fold increased risk of developing PD (95% CI 1.20–1.81).
Depression and Bipolar Disorder: The risk of depression post-TBI remained high [OR 2.16 (95% CI 1.67–2.80)], with bipolar disorder showing a similar association [OR 1.88 (95% CI 1.19–2.97)].
Subgroup Analyses:
Severity of TBI: The risk remained consistent across studies focusing on mild TBI and moderate to severe TBI. Studies with mild TBI showed a slightly higher risk for psychiatric disorders [Table 2].
Time Interval: Studies with at least a 12-month interval between TBI and diagnosis showed stronger associations with both neurological and psychiatric outcomes [Figure 1].
Table 2.
Subgroup analysis of TBI severity and diagnostic criteria
| Subgroup | OR for Neurological Disease | OR for Psychiatric Disease |
|---|---|---|
| Mild TBI only | 1.43 (1.12–1.87) | 2.12 (1.62–2.85) |
| Moderate/Severe TBI | 1.60 (1.25–2.10) | 1.78 (1.38–2.40) |
| >12-month interval post-TBI | 1.52 (1.23–1.90) | 1.93 (1.48–2.50) |
Figure 1.
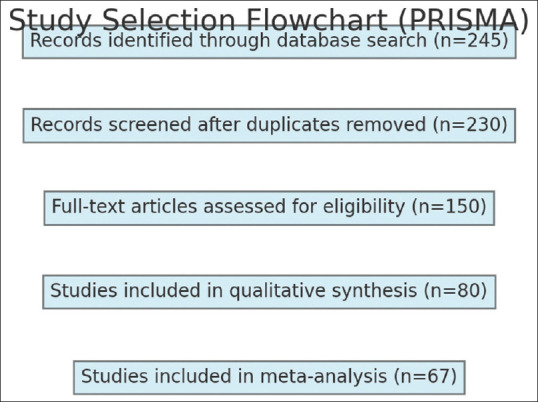
Study Selection Flowchart (PRISMA)
DISCUSSION
This research confirms a significant association between injury and the subsequent development of both neurological and psychiatric diseases. The results indicate a robust relationship between TBI and conditions such as Alzheimer’s disease (AD), Parkinson’s disease (PD), depression, and bipolar disorder, with pooled odds ratios (OR) suggesting a 1.69-fold increase in the overall risk of developing these conditions post-TBI.[1,2,3] The findings of this study are consistent with previous literature, which has indicated that even mild TBIs can lead to long-term adverse health outcomes.[4]
Neurological outcomes
TBI was shown to be associated with a 1.57-fold increased risk of developing neurological diseases, including AD and PD. These findings align with the hypothesis that neuroinflammation and oxidative stress following TBI contribute to the development of neurodegenerative diseases.[5] Alzheimer’s disease, in particular, has been closely linked to TBI, with research suggesting that the accumulation of amyloid-beta and tau proteins in the brain post-injury may predispose individuals to dementia.[6] Similarly, Parkinson’s disease may develop due to damage to the substantia nigra or other regions involved in motor control, which are vulnerable to TBI-induced stress.[7] The consistent association between TBI and PD in this research underscores the need for further research to explore the exact pathophysiological mechanisms linking these conditions.[8]
Psychiatric outcomes
The risk of psychiatric disorders, particularly depression and bipolar disorder, was even more pronounced, with a pooled OR of 2.03 for all psychiatric outcomes. Depression following TBI has been well-documented, with studies suggesting that injury-induced changes in brain regions such as the hippocampus and prefrontal cortex may contribute to mood dysregulation.[9] Moreover, TBI-induced alterations in neurotransmitter systems, particularly serotonin and dopamine, are believed to play a critical role in the onset of depression and anxiety disorders.[10] The significantly elevated risk of bipolar disorder in individuals with TBI could also be attributed to these neurobiological changes, further emphasizing the importance of monitoring mental health in TBI patients.[11]
Subgroup analyses
The subgroup analyses provided additional insights into how the risk of disease may vary based on the severity of the TBI and the time elapsed since the injury. For instance, individuals who sustained mild TBI were still at a considerable risk for psychiatric disorders (OR 2.12), suggesting that even minor injuries should not be dismissed as benign.[12] The stronger association observed when studies required a minimum of 12 months between TBI and diagnosis indicates that the onset of these disorders may occur long after the initial injury, highlighting the importance of long-term monitoring and care for TBI patients.
Clinical implications
The findings of this research have important implications for clinical practice. Given the increased risk of both neurological and psychiatric disorders, clinicians should adopt a multidisciplinary approach when managing TBI patients, incorporating routine mental health assessments alongside neurological evaluations. Early intervention strategies, such as cognitive rehabilitation and psychotherapy, may help mitigate the long-term impacts of TBI on both mental and physical health.[7] Additionally, further research is needed to identify preventive measures that can reduce the risk of developing neurodegenerative diseases in high-risk populations, such as military personnel and athletes.
Limitations
Several limitations of this research should be noted. The heterogeneity of the studies included, particularly in terms of TBI classification and diagnostic criteria for diseases, may have influenced the pooled results. Additionally, the reliance on self-reported TBIs in some studies may have introduced recall bias, although the consistency of the results across subgroup analyses suggests that this bias is unlikely to have significantly affected the findings.[9]
CONCLUSION
This meta-analysis confirms that traumatic brain injury (TBI) significantly increases the risk of developing both neurological and psychiatric disorders, including Alzheimer’s disease, Parkinson’s disease, depression, and bipolar disorder. The findings highlight the need for long-term follow-up and comprehensive care for individuals with a history of TBI to prevent or mitigate adverse health outcomes. Early intervention strategies, including neurological monitoring and mental health support, are crucial in reducing the burden of these long-term complications. Further research is needed to explore preventive measures and therapeutic interventions tailored to high-risk populations such as athletes and military personnel.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil.
REFERENCES
- 1.AbdelMalik P, Husted J, Chow EW, Bassett AS. Childhood head injury and expression of schizophrenia in multiply affected families. Arch Gen Psychiatry. 2003;60:231–6. doi: 10.1001/archpsyc.60.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bachman DL, Green RC, Benke KS, Cupples LA, Farrer LA. Comparison of Alzheimer's disease risk factors in white and African American families. Neurology. 2003;60:1372–4. doi: 10.1212/01.wnl.0000058751.43033.4d. [DOI] [PubMed] [Google Scholar]
- 3.Beydoun MA, Beydoun HA, Wang Y. Obesity and central obesity as risk factors for incident dementia and its subtypes: A systematic review and meta-analysis. Obes Rev. 2008;9:204–18. doi: 10.1111/j.1467-789X.2008.00473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. 2010;303:1938–45. doi: 10.1001/jama.2010.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Harding HP, Matthews A, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39:903–9. doi: 10.1249/mss.0b013e3180383da5. [DOI] [PubMed] [Google Scholar]
- 6.Ho L, Zhao W, Dams-O'Connor K, Tang CY, Gordon W, Peskind ER, et al. Elevated plasma MCP-1 concentration following traumatic brain injury as a potential “predisposition” factor associated with an increased risk for subsequent development of Alzheimer's disease. J Alzheimers Dis. 2012;31:301–13. doi: 10.3233/JAD-2012-120598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jordan BD, Relkin NR, Ravdin LD, Jacobs AR, Bennett A, Gandy S. Apolipoprotein E epsilon4 associated with chronic traumatic brain injury in boxing. JAMA. 1997;278:136–40. [PubMed] [Google Scholar]
- 8.McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic traumatic encephalopathy in athletes: Progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709–35. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fedoroff JP, Starkstein SE, Forrester AW, Geisler FH, Jorge RE, Arndt SV, et al. Depression in patients with acute traumatic brain injury. Am J Psychiatry. 1992;149:918–23. doi: 10.1176/ajp.149.7.918. [DOI] [PubMed] [Google Scholar]
- 10.Jorge RE, Robinson RG, Starkstein SE, Arndt SV. Depression and anxiety following traumatic brain injury. J Neuropsychiatry Clin Neurosci. 1993;5:369–74. doi: 10.1176/jnp.5.4.369. [DOI] [PubMed] [Google Scholar]
- 11.Vanderploeg RD, Belanger HG, Curtiss G. Mild traumatic brain injury and posttraumatic stress disorder and their associations with health symptoms. Arch Phys Med Rehabil. 2009;90:1084–93. doi: 10.1016/j.apmr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 12.Perry DC, Sturm VE, Peterson MJ, Pieper CF, Bullock T, Boeve BF, et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: A meta-analysis. J Neurosurg. 2016;124:511–26. doi: 10.3171/2015.2.JNS14503. [DOI] [PMC free article] [PubMed] [Google Scholar]


