Abstract
Purpose
Disparities in the behavioral health outcomes for lesbian, gay, bisexual, transgender, and queer+ (LGBTQ+) adults—such as depression, anxiety, and alcohol use—are often attributed to experiences of discrimination, victimization, and lack of supportive environments, including hetero- and cis-normative family settings. Yet, how family environments in childhood influence LGBTQ+ adults’ behavioral health and internalized homonegativity has not been extensively examined.
Methods
This study utilized a U.S. national dataset of LGBTQ+ adults (N = 499). Data were collected in November 2020 using an online survey. A series of multivariate ordinary least squares regression models and Sobel tests were performed.
Results
Results showed that as homophobic messages from family increased, levels of depression (β = .19, p < .001), anxiety (β = .17, p < .001), and internalized homonegativity (β = .13, p < .01) increased. As the conservatism level in families increased, levels of alcohol use (β = .11, p < .05), and internalized homonegativity (β = .15, p < .01) increased. In the mediation analysis, internalized homonegativity was found to partially mediate the relationship between homophobic messages from family and depression (z = 3.35, p < .001), homophobic messages and anxiety (z = 3.09, p < .01), and conservatism in family and alcohol use (z = 2.80, p < 0.01). Internalized homonegativity also fully mediated the relationship between homophobic messages and alcohol use (z = 2.66, p < 0.01), conservatism in family and depression (z = 3.76, p < 0.001), and conservatism in family and anxiety (z = 3.45, p < 0.001).
Conclusion
Study findings underscore the importance of inclusive climates within a family and internalized homonegativity as a mediator for LGBTQ+ individuals’ behavioral health. Implications for intervention and future research are discussed.
Introduction
Lesbian, gay, bisexual, transgender, queer and other sexual and gender diverse (LGBTQ+) adults experience heightened rates of negative behavioral health outcomes (e.g., depression, anxiety, alcohol use) compared to their heterosexual and cisgender peers [1–3]. These disparities are often attributed to the presence of unique and chronic stressors, referred to as “minority stress”—that may include experiences of discrimination, victimization, and lack of supportive environments with pervasive heteronormativity and cisnormativity [4,5]. Heteronormativity is the assumption that heterosexuality is the only “normal” sexual orientation, often leading to the privilege of heterosexual relationships and gender norms within society. Likewise, cisnormativity views cisgender as the only acceptable gender identity and confers privileges and advantages to individuals whose identities fall within its imposed constraints. Even though societies adopt more policies protecting LGBTQ+ rights and discussing LGBTQ+ issues openly more than before, heteronormativity and cisnormativity remain dominant in the countries worldwide and affect social systems and LGBTQ+ people’s health and development [6,7]. For example, social norms and expectations on gender and sexuality create additional challenges for LGBTQ+ populations in healthcare settings in terms of access to information or quality care [8,9]. In addition, laws that criminalize homosexuality or restrict the rights of transgender and gender-diverse individuals can place LGBTQ+ people at increased risk of physical violence, job loss, social exclusion, and suicidality [10,11]. Among social systems, the family environment has a particularly direct and profound influence in shaping and reinforcing cis- and heteronormativity on LGBTQ+ individuals [12]. In the United States, only 38% of LGBTQ+ young people reported home as a LGBTQ + -affirming space [13]. Childhood family environments, which may involve experiences of power imbalances and lack of autonomy, can have lasting effects on behavioral health, extending into adulthood [12,14–16].
An issue closely related to behavioral health is internalized homonegativity (IH), a process in which LGBTQ+ individuals receive negative social messages about their sexual identity and incorporate those views into their self-concept [17,18]. IH is also considered a consequence of heteronormative societal beliefs and affects one’s behavioral health [4,19,20]. Yet, how the family environment in childhood influences LGBTQ+ adults’ behavioral health and whether IH plays a mediation role have not been extensively examined. This study aims to add to this literature using a national survey of LGBTQ+ adults.
Behavioral health disparities facing LGBTQ+ adults
Compared to heterosexual and cisgender people, LGBTQ+ populations are disproportionately struggling with mental health problems and suicidality [1,21]. From U.S. Census Bureau data, 18.8%–60.8% of LGBTQ+ adults (depending on subgroup) reported symptoms of anxiety, compared to 14.3%–42.5% of non-LGBTQ+ peers [2]. Additional data showed that compared to their non-LGBTQ+ counterparts, LGBTQ+ adults report higher symptoms of depression (11.4%–28.9% vs 15.5%–50.0%, respectively) and major depressive episodes (7.0% vs 26.7%, respectively [2,3]. Additionally, LGBTQ+ adults were more likely to engage in binge drinking alcohol during the past 30 days compared to their non-LGBTQ+ counterparts (32.0% vs 22.0%) [3]. Given the behavioral health disparities facing LGBTQ+ populations, it is essential to understand the mechanisms behind and factors that could potentially mitigate the disparities.
Social and family environments for LGBTQ+ people
Affirming and inclusive social environments for LGBTQ+ people have multiple characteristics, including acknowledging LGBTQ+ identities, providing safe spaces, using inclusive language, and confronting stigma and discrimination [22,23]. An LGBTQ+ -affirming or inclusive environment is a safe space for individuals expressing themselves and seek help or support [24,25]. Researchers have investigated the influences of state, school, and community climates among LGBTQ+ populations and found that more affirming environments are associated with lower odds of binge drinking, depression, and suicidal ideation among LGBTQ+ youth [24,26–31]. Alternatively, spaces where behaviors such as making negative comments about LGBTQ+ issues, using derogatory slurs for LGBTQ+ people, enforcing gender-binary norms, not welcoming LGBTQ+ people to family activities, or espousing hostile political or religious views characterize non-affirming or rejecting environments for LGBTQ+ people [32–34]. These non-affirming or hostile environments could fall under the category of sexual orientation microaggressions and can negatively affect LGBTQ+ people’s behavioral health [35,36].
Research on family environments has explored relationships between parenting practices, acceptance or rejection responses to children’s coming out, and parental cultural expectations of children [37–41]. Despite important findings about influences of family and caregiver interactions with LGBTQ+ children’s behavioral health outcomes, existing studies largely focus on individual-level factors. For example, parental responses to coming out, family member’s acceptance-rejection responses, family connectedness, and parents’ awareness of children’s identities are often discussed in literature, and they predict LGBTQ+ people’s behavioral health outcomes [15,42]. Broader influences of family views, interactions, and beliefs in the childhood environment and their relationships with LGBTQ+ behavioral health outcomes in adulthood have been under-researched but may play important roles in understanding and improving LGBTQ+ behavioral health disparities. Next, we discuss various domains of the family environment for LGBTQ+ people and their influences on LGBTQ+ behavioral health.
Homophobic language used in family.
Not only do overt acts of homophobia cause harm, but also subtle forms of homophobia, such as hearing homophobic language in social environments, can threaten the psychological safety and well-being of LGBTQ+ youth [12,43,44]. Prejudice-based words can impact stigmatized groups even if they are not the direct target of the comments [45]. Silverschanz and others found that college students in the northwestern U.S. who experienced ambient heterosexist harassment, such as hearing offensive remarks about LGBTQ+ people, reported higher substance use [46]. Those exposed to both personal and ambient harassment had worse well-being than those unexposed. The study highlighted the harmful impact of homophobic language. Other studies also examined the associations between exposure to homophobic language and various outcomes including psychological distress, and found a negative impact from indirect discrimination [44,45]. Current literature predominantly represents rejecting responses from families to LGBTQ+ children through explicit verbal harassment [33,34,47]. However, environmental factors also play a crucial role in shaping these responses. The mechanisms of ambient homophobic messages within a family and its subsequent impacts on LGBTQ+ youth behavioral health are not yet fully understood.
Political conservatism in family.
Political discourse is another way heteronormativity can manifest in social settings. Historically, LGBTQ+ rights have been supported by liberal political groups and opposed by conservative political groups [48,49]. Studies suggest that people with conservative political ideology generally have more negative attitudes toward LGBTQ+ policies, less willingness to engage in LGBTQ+ activities, and greater endorsement of binary gender beliefs [50–54]. Research suggests that conservative family members oftentimes view youth sexual and/or gender expressions and identities that deviate from cis-heteronormative norms as temporary and expect individuals to settle into heterosexual relationships over time [55–57]. In fact, some caregivers self-identify as progressive but still grapple with accepting LGBTQ+ identities within their family unit [58]. Familial perspectives and pressures aligned with heteronormative societal views and practices generally inhibit LGBTQ+ youth development and may exacerbate minority stressors, such as identity management and concealment, subsequently adversely impacting mental well-being [59,60]. Negative LGBTQ+ political attitudes can contribute to psychosocial harm to LGBTQ+ individuals, as evidenced by numerous studies elucidating the deleterious impacts of recent increasing anti-LGBTQ+ policies on LGBTQ+ youth families and mental well-being [10,61–63].
Openly LGBTQ+ people in family.
The composition and outness of family members also contribute to the family context for LGBTQ+ youth. Research suggests that growing up with LGBTQ+ parents can offer benefits for LGBTQ+ children, such as a more positive coming-out process and reduced concerns about family rejection [64]. In addition, extended relatives who identify as LGBTQ+ , such as aunts or cousins, were regarded as important supports for LGBTQ+ young adults navigating family environments centering heteronormativity [65]. During adolescence, LGBTQ+ youth often look to family members as role models [66], and adolescents seek psychological support, shared experience, self-acceptance, and assistance in overcoming challenging experiences from role models [67]. Therefore, open LGBTQ+ adults in the family could serve as both role models and sources of social supports to help foster positive development and well-being of LGBTQ+ individuals However, the impacts of having openly LGBTQ+ people within a family unit while growing up and the subsequent influences on LGBTQ+ individuals’ behavioral health in adulthood has not been adequately investigated.
Internalized homonegativity as a mediator
Underlying psychological processes can be important mechanisms in behavioral health disparities with marginalized populations. In Hatzenbuehler’s Psychological Mediation Framework (PMF) [68], cognitive processes are one of the mechanisms mediating the relationship between stigma-related stress and psychopathology. That is, negative views of the self may result from stigma-based stressful environments and contribute to behavioral health outcomes. IH is a psychological process of absorbing negative social views into the self-concept, often resulting in the development of an internal conflict with one’s own identity [18]. IH stems from stigma-based stress exposure in hostile environments [69,70] and is a predictor of poor behavioral health outcomes [18,71–73]. Studies have shown that IH plays a mediation role between cultural expectations and past parental rejection and current psychological distress among LGBTQ+ population [38,74]. However, again, the pathways from the family environmental factors through IH to behavioral health were not fully examined yet.
Current study
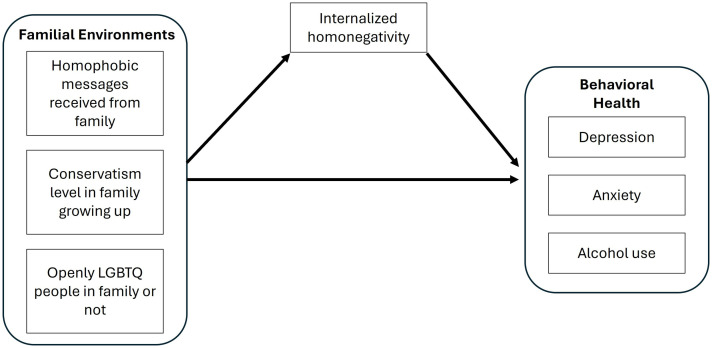
With few studies focusing on the influences of family environment factors on LGBTQ+ adult’s behavioral health, the purpose of this study was to understand whether family environment factors growing up are risk or protective factors for LGBTQ+ adult behavioral health problems, including depression, anxiety, and alcohol use. In addition, the potential mediating role of IH in the path between family factors and outcomes will be examined. This study aims to answer the following research questions: (1) How are family environment factors growing up (i.e., homophobic messages received from family; conservatism level in family growing up; having openly LGBTQ+ people in family or not) associated with LGBTQ+ adult children’s behavioral health issues and IH? (2) How does IH mediate the relationships between family environment and the behavioral health outcomes of depression, anxiety, and alcohol use? Our analyses were guided by this conceptual model (Fig 1), which is based on prior theory and research as described above.
Fig 1. Conceptual model.
Methods
This study used cross-sectional data from a national U.S. study of LGBTQ+ adults. Data were collected in an online survey from November 2, 2020 to February 2, 2021 through CloudResearch, a participant-sourcing platform for online research [75]. Informed consent was attained online by the adult participants anonymously agreeing to participate, and then participants completed survey questions about demographics, IH, behavioral health, including depression, anxiety, and alcohol use, and family environments growing up. Participants were paid $10 for their participation. Validity check items were embedded in the survey, and mischievous respondents were removed. The study was approved by the authors’ Institutional Review Board (Reference: R21MD012687).
Measures
Internalized homonegativity.
The Internalized Homonegativity Inventory (IHNI) is a 23-item scale with three subscales that include IH, morality of homosexuality, and identity affirmation [76]. IHNI responses were measured with a 7-point Likert-type scale from 1 (Strongly Disagree) to 7 (Strongly Agree) to understand the emotions and thoughts related to being a sexual minority. Example IHNI items included the following: “I feel ashamed of my homosexuality.” “In my opinion, homosexuality is harmful to the order of society.” “I am thankful for my sexual orientation.” The subscale of identity affirmation was reverse scored. Average scores ranging from 1 to 7 were used for analysis. Higher scores indicate higher levels of IH. In this study, the internal consistency reliability of IHNI was very good (α = .94).
Depression symptoms.
The Clinically Useful Depression Outcome Scale (CUDOS) is a 16-item scale of depressive symptoms [77]. Participants’ indicated the frequency that they had experienced depressive symptoms in the past 2 weeks using response options that ranged from 1 (Never) to 5 (Almost Every Day). Average scores ranging from 1 to 5 were used for analysis. Higher scores indicate higher levels of depressive symptom severity. In this study, the internal consistency reliability of the CUDOS was very good (α = .93).
Anxiety symptoms.
Anxiety symptoms in this study were measured with Beck Anxiety Inventory (BAI) [78]. The BAI consists of 21 anxiety symptom items. Participants rated how much they had been bothered by each symptom in the past 30 days using response options that ranged from 1 (Not At All) to 4 (Extremely). Average scores ranging from 1 to 4 were used for analysis. Higher scores indicate higher levels of general anxiety symptom severity. In this study, the internal consistency reliability of the BAI was very good (α = .95).
Alcohol use.
PROMIS Item Bank v1.0 - Alcohol: Alcohol Use – Short Form 7a was a 7-item, 5-point Likert-type scale [79]. Participants’ responses ranging from 1 (Never) to 5 (Almost Always) to answer alcohol use statements in the past 30 days. Example items include “I spent too much time drinking alcohol” or “It was difficult for me to stop drinking after one or two drinks.” Average scores ranging from 1 to 5 were used for analysis. Higher scores indicate higher levels of alcohol use. In this study, the internal consistency reliability of the Alcohol Use – Short Form 7a was very good (α = .97).
Homophobic messages received from family.
Homophobic messages received from family is a 5-item measure with a 5-point Likert scale response set, which was modified from the Attitudes Toward Lesbians and Gay Men Scale (ATLG-R-S5) [80]. Participants chose 1 (Never) to 5 (Almost Always) to answer the frequency they heard homophobic messages from their family growing up. Example items include: “Sexual activity between people of the same sex is just plain wrong” or “LGBTQ+ people are disgusting.” Average scores ranging from 1 to 5 were used for analysis. Higher scores indicate the higher frequency of receiving homophobic messages from family growing up. In this study, the internal consistency reliability of ATLG-R-S5 was good (α = .87).
Conservatism level in family growing up.
Conservatism level in one’s family growing up was measured with a 1-item, 9-point Likert scale question with options from 1 (Very Liberal) to 9 (Very Conservative). Higher scores indicate higher level of conservatism in family.
Openly LGBTQ+ people in family or not.
Participants answered a question developed by the research team about LGBTQ+ in their families: “When you were growing up, how many openly LGBTQ+ people were there in your family?” Response options were 0, 1 or 2, 3 or 4, or 5 or more. Given the response distribution, this variable was recoded 0 (No openly LGBTQ+ people in family) and 1 (Having openly LGBTQ+ people in family).
Demographic.
Demographic variables for participants included the following: Age (in years); gender identity (0 = cisgender; 1 = transgender and gender diverse); sexual orientation identity (0 = gay/lesbian; 1 = bisexual and/or pansexual; 2 = queer; 3 other identities [e.g., asexual, questioning]); racial/ethnic identity (0 = White; 1 = Asian or Pacific Islander; 2 = Black; 3 = Latinx; 4 = Multiracial; 5 = Native American); immigrant status (0 = US-born and not from an immigrant family; 1 = immigrant family background); and geographic area grow up in (0 = small town/rural), 1 (suburban), and 2 (large city/urban).
Data analysis
Analyses were conducted in Stata/BE 18.0. Descriptive statistics, including central tendency, variability, and frequency distributions, were run. Main assumptions of linear regression, including linearity, homoscedasticity, normality of the error term, and no multicollinearity were tested using visual tests, Breusch-Pagan test, and variance inflation factors, and no issues that would preclude regression were found.
Next, guided by Fig 1, a series of multiple linear regression models were run to examine how family environment factors growing up (e.g., homophobic messages received from family; conservatism level in family growing up; openly LGBTQ+ people in family or not) were associated with LGBTQ+ adult’s depression, anxiety, alcohol use, and IH. Openly LGBTQ+ people in family was a dichotomous variable, and other independent variables (IVs) and dependent variables (DVs) were continuous variables. After multilinear regression tests, the IH variable was further assessed to determine if there was a mediating relationship on family environment factors and behavioral health outcomes of depression, anxiety, and alcohol use. The first step to test a mediation effect was to examine whether the mediator (i.e.,IH) was associated with the IVs (i.e., homophobic messages received from family, conservatism level in family growing up, and openly LGBTQ+ people in family or not). The IVs showing significant associations with the mediator were then regressed on each DV (i.e., depression, anxiety, and alcohol use) to see if there were significant associations between the mediator and DVs and between IVs and DVs. Six regression models were generated using Sobel tests. All the models controlled for age, racial/ethnic identity, gender identity, sexual orientation, immigrant background, and geographic area. Age was a continuous variable. The other demographic variables were categorical and were dummy coded for analyses. The Sobel tests calculations were conducted using an interactive calculation tool developed by Preacher and Leonardelli [81].
Results
Demographic characteristics
The sample included 499 LGBTQ+ adults, and the demographic characteristics are shown in Table 1. Ages ranged from 18 to 70 years, with an average age of 33.7 (SD = 10.0). Most participants identified as cisgender (86.0%) while 14.0% of them identified as transgender or gender diverse. Regarding sexual orientation, 60.9% identified as bisexual and/or pansexual, 29.9% identified as gay or lesbian, 8.4% identified as queer, and 4 (0.8%) participants had other sexual identities including demisexual or questioning. In terms of racial/ethnic identity, over 60% were White (64.8%), with additional participants identifying as Asian (6.2%), Black (14.6%), Latinx (11.8%), multiracial (0.4%), and Native American (2.2%). Most participants (85.4%) were U.S.-born and not from an immigrant family, and the sample was diverse on geographic background with 47.3% growing up in suburban area, 29.4% in small town or rural area, and 23.3% in large city or urban area.
Table 1. Participant demographics (n = 499).
| Variable | Mean (SD) or n (%) |
|---|---|
| Internalized homonegativity (range = 1–7) | 2.1 (0.9) |
| Depression (range = 1–5) | 2.2 (0.9) |
| Anxiety (range = 1–4) | 1.8 (0.6) |
| Alcohol abuse (range = 1–5) | 1.5 (0.8) |
| Homophobic messages from family (range = 1–5) | 2.4 (0.8) |
| Conservatism level in family growing up (range = 1–9) | 1.2 (0.8) |
| Having openly LGBTQ+ people in family growing up | |
| Yes | 147 (29.5) |
| No | 352 (70.5) |
| Age | 33.7 (10.0) |
| Gender identity | |
| Cisgender | 429 (86.0) |
| Transgender and gender diverse | 70 (14.0) |
| Sexual orientation | |
| Gay or Lesbian | 149 (29.9) |
| Bisexual, Pansexual, or Bi/Pan+ | 304 (60.9) |
| Queer | 42 (8.4) |
| Other | 4 (0.8) |
| Racial/ethnic identity | |
| White | 323 (64.7) |
| Asian or Pacific Islander | 31 (6.2) |
| Black or African American | 73 (14.6) |
| Latinx | 59 (11.8) |
| Multiracial | 2 (0.4) |
| Native American | 11 (2.2) |
| Immigrant status | |
| U.S.-born and not from an immigrant family | 426 (85.4) |
| Immigrant family background | 73 (14.6) |
| Geographic area grew up in | |
| Small town or rural area | 147 (29.4) |
| Suburban area | 236 (47.3) |
| Large city or urban area | 116 (23.3) |
Notes: SD = Standard Deviation.
Demographics predicting behavioral health outcomes and IH
Compared to cisgender individuals, transgender people reported higher levels of depression (β = .32, SE = 0.11. p < .01). Bisexual/pansexual individuals had significantly higher levels of depression (β = .31, SE = 0.08, p < .001) and anxiety (β = .14, SE = .06, p < .05), and queer sexual orientation identity individuals had significantly higher depression (β = .30, SE = .15, p < .05) compared to gay/lesbian peers. Lastly, Asians or Pacific Islanders (β = .59, SE = .19, p < .01) and Black Americans (β = .67, SE = .13, p < .001) reported higher levels of IH compared to White peers. Latinx people reported significantly lower level of depression (β = −.34, SE = .13, p < .01) compared to White people. Native Americans reported significantly higher level of depression (β = .52, SE = .25, p < .05) and anxiety (β = .51, SE = .18, p < .01) compared to White peers. Results were shown in Table 2.
Table 2. Results of multivariate linear regression models predicting behavioral health outcomes (n = 499).
| Model 1: Depression β (SE) |
Model 2: Anxiety β (SE) |
Model 3: Alcohol abuse β (SE) |
Model 4: IH β (SE) |
|
|---|---|---|---|---|
| Homophobic messages received from family | 0.21 (0.05)*** | 0.14 (0.04)*** | 0.06 (0.05) | 0.05 (0.06) |
| Conservatism level in family growing up | 0.01 (0.02) | 0.01 (0.01) | 0.04 (0.02)* | 0.07 (0.02)*** |
| Openly LGBTQ+ people in family (Ref: No) | ||||
| Yes | 0.06 (0.08) | 0.10 (0.06) | 0.13 (0.08) | 0.09 (0.09) |
| Age | −0.01 (0.004)** | −0.01 (0.003)*** | −0.001 (0.004) | 0.01 (0.004) |
| Gender identity (Ref: Cisgender) | ||||
| Transgender | 0.32 (0.11)** | 0.11 (0.08) | −0.06 (0.11) | −0.14 (0.12) |
| Sexual orientation (Ref: Gay or Lesbian) | ||||
| Bisexual, Pansexual, or Bi/Pan+ | 0.31 (0.08)*** | 0.14 (0.06)* | 0.11 (0.09) | −0.09 (0.09) |
| Queer | 0.30 (0.15)* | 0.21 (0.11) | 0.12 (0.15) | −0.19 (0.16) |
| Other | 0.66 (0.41) | 0.33 (0.30) | 0.11 (0.43) | 0.36 (0.47) |
| Racial/ethnic identity (Ref: White) | ||||
| Asian or Pacific Islander | −0.16 (0.17) | −0.12 (0.13) | −0.28 (0.18) | 0.59 (0.19)** |
| Black or African American | −0.19 (0.11) | −0.06 (0.08) | 0.17 (0.12) | 0.67 (0.13)*** |
| Latinx | −0.34 (0.13)** | −0.06 (0.09) | −0.001 (0.13) | 0.24 (0.14) |
| Multiracial | 0.63 (0.58) | 0.17 (0.43) | −0.64 (0.60) | −0.06 (0.64) |
| Native American | 0.52 (0.25)* | 0.51 (0.18)** | 0.23 (0.26) | −0.23 (0.28) |
| Immigrant status (Ref: U.S.-born and not from an immigrant family) | ||||
| Immigrant family background | 0.17 (0.12) | 0.06 (0.09) | −0.02 (0.12) | −0.16 (0.13) |
| Geographic area grew up in (Ref: small town or rural area) | ||||
| Suburban area | −0.10 (0.09) | −0.09 (0.06) | −0.08 (0.09) | −0.06 (0.09) |
| Large city or urban area | −0.06 (0.11) | −0.10 (0.08) | 0.07 (0.11) | 0.06 (0.12) |
| Model fit | ||||
| F | 5.75*** | 4.91*** | 1.75* | 4.25*** |
| Adjusted R2 | 0.132 | 0.112 | 0.024 | 0.094 |
* p < .05, **p < .01, *** p < .001.
Family environment factors predicting behavioral health outcomes and IH
Family environment factors in this study include homophobic messages received from family, conservatism level in family, and whether having openly LGBTQ+ people in family or not. Results showed that homophobic messages received from family significantly predict depression and anxiety, and conservatism level in family significantly predicted alcohol abuse and IH. As homophobic messages from family increased, levels of depression (β = .21, SE = .05, p < .001) and anxiety (β = .14, SE = .04, p < .001) increased significantly, but alcohol use (β = .06, SE = .05, p = .280) and IH (β = .05, SE = .06, p = .347) just increased slightly. As the conservatism level in family increased, levels of alcohol abuse (β = .04, SE = .02, p < .05) and IH (β = .04, SE = .02, p < .05) increased significantly, but depression (β = .01, SE = .02, p = .575) and anxiety level (β = .01, SE = .01, p = .257) did not. No significant difference in the DVs were found between people with and without openly LGBTQ+ people in the family growing up. Results were shown in Table 2.
Mediation of IH
Among the three family environment factors, openly LGBTQ+ people in one’s family did not have significant associations with any dependent variables; thus, it was not further examined for the indirect effect analysis. As results shown in Table 3, IH partially mediated the relationship between homophobic messages from family and depression (z = 2.00, p < .05). IH also fully mediated the relationships between family conservatism and depression (z = 3.35, p < .001), family conservatism and anxiety (z = 2.38, p < .05), and family conservatism and alcohol abuse (z = 2.65, p < .01).
Table 3. Mediation effect results of IH using Aroian Sobel Tests (n = 499).
| Testing steps | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|---|
| IV | Homophobic messages | Homophobic messages | Homophobic messages | Conservatism level | Conservatism level | Conservatism level | |
| DV | Depression | Anxiety | Alcohol abuse | Depression | Anxiety | Alcohol abuse | |
| 1 |
BetaA
(SE) between IV and Mediator |
0.12 (0.05)* | 0.12 (0.05)* | 0.12 (0.05)* | 0.07 (0.02)*** | 0.07 (0.02)*** | 0.07 (0.02)*** |
| 2 |
BetaB
(SE) between Mediator and DV |
0.20 (0.04)*** | 0.08 (0.03)** | 0.15 (0.04)*** | 0.21 (0.04)*** | 0.09 (0.03)** | 0.14 (0.04)** |
|
BetaC
(SE) between IV and DV |
0.20 (0.05)*** | 0.15 (0.04)*** | 0.08 (0.05) | 0.01 (0.02) | 0.02 (0.01) | 0.03 (0.02) | |
| 3 | Aroian Sobel test statistic Beta (SE) | 2.00 (0.01)* | 1.72 (0.01) | 1.86 (0.01) | 3.35 (0.01)*** | 2.38 (0.003)* | 2.65 (0.004)** |
| Mediation effect | Partial mediation | None | None | Fully mediation | Fully mediation | Fully mediation | |
* p < .05, **p < .01, *** p < .001.
Discussion
Family environments factors and behavioral health outcomes
The results showed homophobic messages at family growing up predicts LGBTQ+ people’s depression and anxiety level in adulthood, which aligns with literature that LGBTQ+ individuals who live in less accepting/affirming environments are at a heightened risk of experiencing negative behavioral health conditions, including depression, PTSD, and suicidal ideation [82,83]. Wang and others found that young adults exposed to homophobic messaging, both verbally and online, developed higher rates of severe depression, anxiety, and physical pain in emerging adulthood [84]. It should be noted that homophobic comments do not have to be directly communicated to LGBTQ+ youth for them to be harmful—just exposure to homophobic messages in the family environment can have subsequent negative effects.
The results showed that family conservatism significantly predicted alcohol abuse and IH. These results align with findings from Pacilli and Colleagues’ study [85], which found a significant association between right-wing conservative political orientation and IH in a LGBTQ+ sample. Also, scholars have found that parents’ political conservatism contributed to negative parental reactions to their LGBTQ+ children’s coming out [86]. No existing literature was found on the influence of family conservatism and LGBTQ+ alcohol abuse, which warrants further research.
Extant research suggests that growing up with LGBTQ+ parents or relatives can offer benefits, such as a smoother coming-out processes, reduced concern about family rejection, reduced isolation, and better connection to LGBTQ+ communities and cultures [64,65], which are associated with better behavioral health outcomes [15,87] and lower IH [74]. However, our study found no association between having openly LGBTQ+ family members and behavioral health outcomes or IH. One possible explanation is that the presence of openly LGBTQ+ individuals in the family is not an essential component of a supportive family environment. Supportive and affirming family dynamics can manifest through acceptance, open communication, inclusive language, and consistent and explicit support [88,89], regardless of whether there are open LGBTQ+ family members. These family elements have been shown to play critical roles in shaping LGBTQ+ youth’s behavioral health and internalized attitudes [15,87]. For example, Stone and Colleagues identified supportive behaviors for LGBTQ+ youth [65], including LGBTQ+ family members helping youth navigate family communication norms, introducing LGBTQ+ cultures, and helping mediate conflict between LGBTQ+ youth and parents. Future research should more deeply examine how openly LGBTQ+ family members interact in various ways in family contexts that can affect LGBTQ+ youth.
IH as a mediator
While initial regression analysis found that family conservatism was associated with alcohol abuse, mediation results suggest that IH fully mediated the relationship between family conservatism and all three behavioral health outcomes. In other words, family conservatism may have adverse effects on LGBTQ+ individuals’ depression, anxiety, and alcohol abuse only when channeled through IH. No prior studies were located that examined IH as a mediator between family conservatism growing up and the outcomes of depression, anxiety, and alcohol abuse. Nonetheless, politics has played a significant role in the lives of LGBTQ+ people for decades, with LGBTQ+ rights and discrimination being the focus of political movements and the enactment of legislation via political parties [90,91]. Multiple studies (with the general population and LGBTQ+ participants) have found that political conservatism is associated with negative attitudes about LGBTQ+ communities [50–54]. Therefore, growing up in a family with politically conservative ideologies likely contributes to IH, and there is substantial research connecting IH and behavioral health problems [71–73,92,93]. Given that political conservatism in the family context is a complex construct that could encompass multiple elements, more research is needed in this area.
Our findings that IH partially mediates the relationship between family homophobic messaging and depression fill a gap in the literature as there is a lack of evidence about the mediation role of IH between family homophobic messages and behavioral health outcomes for LGBTQ+ youth. Our findings do align studies showing IH as a mediator between lesbians and gay men’s experiences of general experiences with discrimination and symptoms of depression [94]. Moreover, IH has been positively associated with family sexual stigma and mental health problems among LGBTQ+ people [95,96]. These results from our findings along with previous literature raise important concerns on the influence of family environment given that IH can develop over long periods of time despite avoiding interactions with homophobic family members during adulthood [96].
Implications for practice
This study underscores the critical role of childhood family environments in shaping the behavioral health and internalized self-concepts of LGBTQ+ adults. Interventions aimed at reducing behavioral health disparities among LGBTQ+ populations should focus on addressing the adverse effects of unsupportive family environments, such as homophobic language and conservative political views. Incorporating family dynamics and inclusive practices into therapy, support programs, and educational initiatives would help mitigate the negative impacts of childhood environmental homophobia. While existing efforts, such as school-based Gender-Sexuality Alliances and the Family Acceptance Project, and have demonstrated positive impacts on the well-being of LGBTQ+ individuals [97,98], these programs primarily serve those who are already aware of their own or their children’s LGBTQ+ identities. Expanding such initiatives to include the general population could foster greater awareness and inclusivity, thereby reducing the prevalence of environmental homophobia more broadly. Moreover, programs supporting families with LGBTQ+ members, such as support groups offered by Parents, Families, and Friends of Lesbians and Gays (PFLAG), could be further developed more to encourage more families to engage in creating inclusive environments for LGBTQ+ children. In addition to developing inclusive programs, when working with LGBTQ+ individuals, clinicians should explore with them how their beliefs and perception about LGBTQ+ identities. One’s thoughts and feelings about being an LGBTQ+ individual in hetero- and cis-normative societies impacts their stress and health outcomes [4,99,100]. Interventions on reducing IH should be emphasized in research and practice to provide supportive service for LGBTQ+ populations.
Data for this study were collected during the COVID-19 pandemic, a period that may strengthen stigmatization existing pre-pandemic and worsen LGBTQ+ individual’s behavioral health due to undesired family interactions, social isolation, or political polarization [101]. These unique circumstances demonstrated the needs for accessible and crisis-responsive support or service systems that can address LGBTQ + -related stressors, especially within the family context.
Limitations
The present study has some limitations, which should be addressed in future research. First, regarding generalizability, the participants were primarily cisgender individuals (86.0%), which may not fully reflect the range of life experiences of gender-diverse people. Some items in the homophobic message scale were modified to include gender-diverse populations, but the survey still lacks questions specifically related to gender diversity or transphobic situations. In addition, data for this study were collected during the COVID-19 pandemic. This unique circumstance may have influenced participants’ experiences of family interactions, minority stress, and mental health. For example, LGBTQ+ people may have lost access to LGBTQ+ communities and moved back into non-affirming homes, increasing the likelihood of tense family situations. As such, the findings may not fully generalize to non-pandemic conditions.
Second, the participants were adults with ages ranging from 18 to 70 years but were asked to recall the family environment growing up, which may involve potential recall bias. Furthermore, the researchers who designed the survey did not provide a fixed definition of “family” in the survey. Therefore, the question relies on participants’ understanding of family. While the use of “when you were growing up” in the item implies that the question refers to the family of origin, it still could be interpreted differently by participants (e.g., immediate family vs. extended family).
Third, regarding the analysis, our data were cross-sectional, so no causal inferences can be made about whether family environments and IH lead to behavioral health outcomes. Moreover, we conducted multiple regression models without applying formal corrections for multiple testing. Although the models were guided by theoretical framework and prior empirical findings to reduce the concern of inflated Type I error, we acknowledge this as a limitation in the data analysis. Last, due to data availability, information of gender identity disaggregated into cisgender-men and cisgender-women, as well as more specific breakdown (e.g., bi/pansexual), was not included in the analysis.
Future research
Future research should use longitudinal study designs to better understand how childhood family environments influence LGBTQ+ individuals’ behavioral health and IH over time and help establish causal relationships. Studies should include more gender-diverse participants and more detailed demographic breakdowns, such as sexual orientation subgroups. Exploring the interplay of diverse family structures, such as stepfamilies or same-sex parent families, and intersecting identities, such as racial/ethnic identity, gender identity, and socioeconomic background, could provide valuable insights into these complex dynamics. Additionally, developing and applying clear definitions of family will be important to ensure that findings are interpretable within specific contexts. Further investigations are also needed to examine the potential intersectional influences of age, race/ethnicity, gender identity, sexual orientation, and immigrant background on the mediating role of internalized homonegativity and behavioral health outcomes. These social identities may interact to shape both the experience of stigma and the coping mechanisms to LGBTQ+ individuals. Furthermore, based on the results of this study, more research is needed to explore how openly LGBTQ+ family members affect LGBTQ+ youth and what aspects of political views within the family context impact the behavioral health of LGBTQ+ individuals. Lastly, investigating the protective effects of affirming family environments may inform strategies to promote equitable behavioral health outcomes for LGBTQ+ communities. Finally, researchers should consider implementing corrections for multiple testing when conducting numerous statistical models, particularly in exploratory analyses, to enhance the robustness of findings.
Supporting information
(XLSX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Research reported in this article was supported by the National Institute of Minority Health and Health Disparities of the National Institutes of Health (https://www.nimhd.nih.gov/) under award number R21MD012687. W.H. is the author who received this award. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Adelson SL, Reid G, Miller AM, Sandfort TGM. Health Justice for LGBT Youths: Combining Public Health and Human Rights. J Am Acad Child Adolesc Psychiatry. 2021;60(7):804–7. doi: 10.1016/j.jaac.2021.02.021 [DOI] [PubMed] [Google Scholar]
- 2.Marley M, File T, Scherer Z. LGBT adults report anxiety, depression at all ages [Internet]. Franklin County Free Press; 2022. Dec 14 [cited 2025 May 16]. Available from: https://fcfreepresspa.com/lgbt-adults-report-anxiety-depression-at-all-ages/ [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Substance Abuse and Mental Health Services Administration (SAMHSA)’s public online data analysis system [Internet]. [cited 2024 Jun 11]. Available from: https://datatools.samhsa.gov/das/nsduh/2021/nsduh-2021-ds0001/variable-list [Google Scholar]
- 4.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orellana L, Alarcón T, Schnettler B. Behavior without beliefs: Profiles of heteronormativity and well-being among heterosexual and non-heterosexual university students in Chile. Front Psychol. 2022;13:988054. doi: 10.3389/fpsyg.2022.988054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mills-Koonce WR, Rehder PD, McCurdy AL. The Significance of Parenting and Parent-Child Relationships for Sexual and Gender Minority Adolescents. J Res Adolesc. 2018;28(3):637–49. doi: 10.1111/jora.12404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Bergen DD, Wilson BDM, Russell ST, Gordon AG, Rothblum ED. Parental Responses to Coming out by Lesbian, Gay, Bisexual, Queer, Pansexual, or Two-Spirited People across Three Age Cohorts. J Marriage Fam. 2021;83(4):1116–33. doi: 10.1111/jomf.12731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franco-Rocha OY, Wheldon CW, Osier N, Lett E, Kesler SR, Henneghan AM, et al. Cisheteronormativity and its influence on the psychosocial experience of LGBTQ+ people with cancer: A qualitative systematic review. Psychooncology. 2023;32(6):834–45. doi: 10.1002/pon.6133 [DOI] [PubMed] [Google Scholar]
- 9.Marshall K, Martin W, Walker RL, Vandenberg H. Exploring the Impacts of Heteronormative and Cisnormative Ideologies on Fertility Intentions and Family Planning Experiences Within the 2SLGBTQ Community: A Qualitative Case Study. J Holist Nurs. 2024;42(2):156–67. doi: 10.1177/08980101231189653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee WY, Hobbs JN, Hobaica S, DeChants JP, Price MN, Nath R. State-level anti-transgender laws increase past-year suicide attempts among transgender and non-binary young people in the USA. Nat Hum Behav. 2024;8(11):2096–106. doi: 10.1038/s41562-024-01979-5 [DOI] [PubMed] [Google Scholar]
- 11.Makofane K, Beck J, Lubensky M, Ayala G. Homophobic legislation and its impact on human security. Afr Secur Rev. 2014;23(2):186–95. doi: 10.1080/10246029.2014.913832 [DOI] [Google Scholar]
- 12.McDermott E, Gabb J, Eastham R, Hanbury A. Family trouble: Heteronormativity, emotion work and queer youth mental health. Health (London). 2021;25(2):177–95. doi: 10.1177/1363459319860572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Trevor Project. 2023 U.S. national survey on the mental health of LGBTQ+ young people [Internet]. The Trevor Project; 2023. [cited 2025 May 20]. Available from: https://www.thetrevorproject.org/ [Google Scholar]
- 14.Abraham E, Letkiewicz AM, Wickramaratne PJ, Bunyan M, van Dijk MT, Gameroff MJ, et al. Major depression, temperament, and social support as psychosocial mechanisms of the intergenerational transmission of parenting styles. Dev Psychopathol. 2022;34(5):1997–2011. doi: 10.1017/S0954579421000420 [DOI] [PubMed] [Google Scholar]
- 15.Bouris A, Guilamo-Ramos V, Pickard A, Shiu C, Loosier PS, Dittus P, et al. A systematic review of parental influences on the health and well-being of lesbian, gay, and bisexual youth: time for a new public health research and practice agenda. J Prim Prev. 2010;31(5–6):273–309. doi: 10.1007/s10935-010-0229-1 [DOI] [PubMed] [Google Scholar]
- 16.Rohner RP, Lansford JE. Deep Structure of the Human Affectional System: Introduction to Interpersonal Acceptance–Rejection Theory. J Fam Theory Rev. 2017;9(4):426–40. doi: 10.1111/jftr.12219 [DOI] [Google Scholar]
- 17.Berg RC, Munthe-Kaas HM, Ross MW. Internalized Homonegativity: A Systematic Mapping Review of Empirical Research. J Homosex. 2016;63(4):541–58. doi: 10.1080/00918369.2015.1083788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yolaç E, Meriç M. Internalized homophobia and depression levels in LGBT individuals. Perspect Psychiatr Care. 2021;57(1):304–10. doi: 10.1111/ppc.12564 [DOI] [PubMed] [Google Scholar]
- 19.Hall WJ, Dawes HC, Hannay JW, Williams DY, Frey JJ, Srivastava A, et al. Development and initial validation of the implicit internalized sexual orientation stigma affect misattribution procedure. Front Psychol. 2024;15:1385410. doi: 10.3389/fpsyg.2024.1385410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ventriglio A, Castaldelli-Maia JM, Torales J, De Berardis D, Bhugra D. Homophobia and mental health: a scourge of modern era. Epidemiol Psychiatr Sci. 2021;30:e52. doi: 10.1017/S2045796021000391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M. Estimating the Risk of Attempted Suicide Among Sexual Minority Youths: A Systematic Review and Meta-analysis. JAMA Pediatr. 2018;172(12):1145–52. doi: 10.1001/jamapediatrics.2018.2731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Human Rights Campaign. All children - all families: LGBTQ+ resources for youth-serving professionals [Internet]. HRC Foundation; [cited 2025 May 20]. Available from: https://www.thehrcfoundation.org/professional-resources/all-children-all-families-lgbtq-resources-for-youth-serving-professionals [Google Scholar]
- 23.National LGBT Health Education Center. Providing inclusive services and care for LGBT people - a guide for health care staff [Internet]. National LGBT Health Education Center; 2016. [cited 2025 May 21]. Available from: https://www.lgbtqiahealtheducation.org/publication/learning-guide/ [Google Scholar]
- 24.Chien Y-S, Schwartz G, Huang L, Kawachi I. State LGBTQ policies and binge drinking among sexual minority youth in the US: a multilevel analysis. Soc Psychiatry Psychiatr Epidemiol. 2022;57(1):183–94. doi: 10.1007/s00127-021-02119-4 [DOI] [PubMed] [Google Scholar]
- 25.Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and Cultural Contexts of Alcohol Use: Influences in a Social-Ecological Framework. Alcohol Res. 2016;38(1):35–45. [PMC free article] [PubMed] [Google Scholar]
- 26.Coulter RWS, Birkett M, Corliss HL, Hatzenbuehler ML, Mustanski B, Stall RD. Associations between LGBTQ-affirmative school climate and adolescent drinking behaviors. Drug Alcohol Depend. 2016;161:340–7. doi: 10.1016/j.drugalcdep.2016.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paceley MS, Goffnett J, Gandy‐Guedes M. Impact of victimization, community climate, and community size on the mental health of sexual and gender minority youth. J Community Psychol. 2017;45(5):658–71. doi: 10.1002/jcop.21885 [DOI] [Google Scholar]
- 28.Price MN, Lee WY, Hobbs JN, DeChants JP, Davis CK. Middle and High School LGBTQ Students Report What Makes School LGBTQ-Affirming Across Race/Ethnicity and Gender Identity, a Topic Modeling Method. J Sch Health. 2024;94(7):601–9. doi: 10.1111/josh.13460 [DOI] [PubMed] [Google Scholar]
- 29.Saewyc EM, Li G, Gower AL, Watson RJ, Erickson D, Corliss HL, et al. The link between LGBTQ-supportive communities, progressive political climate, and suicidality among sexual minority adolescents in Canada. Prev Med. 2020;139:106191. doi: 10.1016/j.ypmed.2020.106191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watson RJ, Park M, Taylor AB, Fish JN, Corliss HL, Eisenberg ME, et al. Associations Between Community-Level LGBTQ-Supportive Factors and Substance Use Among Sexual Minority Adolescents. LGBT Health. 2020;7(2):82–9. doi: 10.1089/lgbt.2019.0205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woodford MR, Kulick A, Atteberry B. Protective factors, campus climate, and health outcomes among sexual minority college students. J Divers High Educ. 2015;8(2):73–87. doi: 10.1037/a0038552 [DOI] [Google Scholar]
- 32.Bosse JD, Katz-Wise SL, Chiodo LM. Sexual and Gender Diverse Young Adults’ Perception of Behaviors that are Supportive and Unsupportive of Sexual Orientation and Gender Identities. J Adolesc Res. 2022;39(1):165–95. doi: 10.1177/07435584221124957 [DOI] [Google Scholar]
- 33.Kibrik EL, Cohen N, Stolowicz-Melman D, Levy A, Boruchovitz-Zamir R, Diamond GM. Measuring Adult Children’s Perceptions of Their Parents’ Acceptance and Rejection of Their Sexual Orientation: Initial Development of the Parental Acceptance and Rejection of Sexual Orientation Scale (PARSOS). J Homosex. 2019;66(11):1513–34. doi: 10.1080/00918369.2018.1503460 [DOI] [PubMed] [Google Scholar]
- 34.Ryan C, Rees RA. Supportive families, healthy children: helping latter-day saint families with lesbian, gay, bisexual & transgender children. San Francisco (CA): Marian Wright Edelman Institute, San Francisco State University; 2012. [Google Scholar]
- 35.Marchi M, Travascio A, Uberti D, De Micheli E, Quartaroli F, Laquatra G, et al. Microaggression toward LGBTIQ people and implications for mental health: A systematic review. Int J Soc Psychiatry. 2024;70(1):23–35. doi: 10.1177/00207640231194478 [DOI] [PubMed] [Google Scholar]
- 36.Nadal KL, Whitman CN, Davis LS, Erazo T, Davidoff KC. Microaggressions Toward Lesbian, Gay, Bisexual, Transgender, Queer, and Genderqueer People: A Review of the Literature. J Sex Res. 2016;53(4–5):488–508. doi: 10.1080/00224499.2016.1142495 [DOI] [PubMed] [Google Scholar]
- 37.Felner JK, Wisdom JP, Williams T, Katuska L, Haley SJ, Jun H-J, et al. Stress, Coping, and Context: Examining Substance Use Among LGBTQ Young Adults With Probable Substance Use Disorders. Psychiatr Serv. 2020;71(2):112–20. doi: 10.1176/appi.ps.201900029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang Y-T, Chan RCH, Cui L. Filial piety, internalized homonegativity, and depressive symptoms among Taiwanese gay and bisexual men: A mediation analysis. Am J Orthopsychiatry. 2020;90(3):340–9. doi: 10.1037/ort0000439 [DOI] [PubMed] [Google Scholar]
- 39.Lawrenz P, Habigzang LF. Minority Stress, Parenting Styles, and Mental Health in Brazilian Homosexual Men. J Homosex. 2020;67(5):658–73. doi: 10.1080/00918369.2018.1551665 [DOI] [PubMed] [Google Scholar]
- 40.Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346–52. doi: 10.1542/peds.2007-3524 [DOI] [PubMed] [Google Scholar]
- 41.Ryan C, Toomey RB, Diaz RM, Russell ST. Parent-Initiated Sexual Orientation Change Efforts With LGBT Adolescents: Implications for Young Adult Mental Health and Adjustment. J Homosex. 2020;67(2):159–73. doi: 10.1080/00918369.2018.1538407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bosse JD, Clark KD, Dion KA, Chiodo LM. Transgender and nonbinary young adults’ depression and suicidality is associated with sibling and parental acceptance-rejection. J Nurs Scholarsh. 2024;56(1):87–102. doi: 10.1111/jnu.12917 [DOI] [PubMed] [Google Scholar]
- 43.Athanases SZ, Comar TA. The Performance of Homophobia in Early Adolescents’ Everyday Speech. J LGBT Youth. 2008;5(2):9–32. doi: 10.1080/19361650802092366 [DOI] [Google Scholar]
- 44.Collier KL, Bos HMW, Sandfort TGM. Homophobic name-calling among secondary school students and its implications for mental health. J Youth Adolesc. 2013;42(3):363–75. doi: 10.1007/s10964-012-9823-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norris AL, McGuire JK, Stolz C. Direct and indirect experiences with heterosexism: how slurs impact all students. Appl Dev Sci. 2018;22(2):154–67. [Google Scholar]
- 46.Silverschanz P, Cortina LM, Konik J, Magley VJ. Slurs, Snubs, and Queer Jokes: Incidence and Impact of Heterosexist Harassment in Academia. Sex Roles. 2007;58(3–4):179–91. doi: 10.1007/s11199-007-9329-7 [DOI] [Google Scholar]
- 47.Matsuno E, Huynh KD, Abreu RL. Development and validation of the Trans- and Nonbinary-Affirming Parental Practices (TAPP) measure. J Fam Psychol. 2024;:10.1037/fam0001205. doi: 10.1037/fam0001205 [DOI] [PubMed] [Google Scholar]
- 48.Lin L, Horowitz JM, Hurst K, Braga D. Race and LGBTQ issues in K-12 schools [Internet]. Pew Research Center; 2024. [cited 2025 May 16]. Available from: https://www.pewresearch.org/social-trends/2024/02/22/race-and-lgbtq-issues-in-k-12-schools/ [Google Scholar]
- 49.Sherkat DE, Powell-Williams M, Maddox G, de Vries KM. Religion, politics, and support for same-sex marriage in the United States, 1988–2008. Soc Sci Res. 2011;40(1):167–80. [Google Scholar]
- 50.Dessel AB, Rodenborg N. Social Workers and LGBT Policies: Attitude Predictors and Cultural Competence Course Outcomes. Sex Res Soc Policy. 2016;14(1):17–31. doi: 10.1007/s13178-016-0231-3 [DOI] [Google Scholar]
- 51.Feinstein BA, Dyar C, Bhatia V, Latack JA, Davila J. Conservative Beliefs, Attitudes Toward Bisexuality, and Willingness to Engage in Romantic and Sexual Activities With a Bisexual Partner. Arch Sex Behav. 2016;45(6):1535–50. doi: 10.1007/s10508-015-0642-x [DOI] [PubMed] [Google Scholar]
- 52.Hall WJ, Rodgers GK. Teachers’ attitudes toward homosexuality and the lesbian, gay, bisexual, and queer community in the United States. Soc Psychol Educ. 2018;22(1):23–41. doi: 10.1007/s11218-018-9463-9 [DOI] [Google Scholar]
- 53.Jaffee KD, Dessel AB, Woodford MR. The nature of incoming graduate social work students’ attitudes toward sexual minorities. J Gay Lesbian Soc Serv. 2016;28(4):255–76. doi: 10.1080/10538720.2016.1224210 [DOI] [Google Scholar]
- 54.Prusaczyk E, Hodson G. The Roles of Political Conservatism and Binary Gender Beliefs in Predicting Prejudices Toward Gay Men and People Who Are Transgender. Sex Roles. 2019;82(7–8):438–46. doi: 10.1007/s11199-019-01069-1 [DOI] [Google Scholar]
- 55.Gray ML. From websites to Wal-Mart: youth, identity work, and the queering of boundary publics in small town, USA. Am Stud. 2007;48(2):49–59. [Google Scholar]
- 56.Gray ML. Negotiating Identities/Queering Desires: Coming Out Online and the Remediation of the Coming-Out Story. J Computer-Mediat Commun. 2009;14(4):1162–89. doi: 10.1111/j.1083-6101.2009.01485.x [DOI] [Google Scholar]
- 57.Hulko W, Hovanes J. Intersectionality in the Lives of LGBTQ Youth: Identifying as LGBTQ and Finding Community in Small Cities and Rural Towns. J Homosex. 2018;65(4):427–55. doi: 10.1080/00918369.2017.1320169 [DOI] [PubMed] [Google Scholar]
- 58.Ghosh A. After coming out: Parental acceptance of young lesbian and gay people. Sociol Compass. 2020;14(1):e12740. doi: 10.1111/soc4.12740 [DOI] [Google Scholar]
- 59.Elliott KJ, Stacciarini J-MR, Jimenez IA, Rangel AP, Fanfan D. A Review of Psychosocial Protective and Risk Factors for the Mental Well-Being of Rural LGBTQ+ Adolescents. Youth Soc. 2021;54(2):312–41. doi: 10.1177/0044118x211035944 [DOI] [Google Scholar]
- 60.Katz-Wise SL, Rosario M, Tsappis M. Lesbian, Gay, Bisexual, and Transgender Youth and Family Acceptance. Pediatr Clin North Am. 2016;63(6):1011–25. doi: 10.1016/j.pcl.2016.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goldberg AE, Abreu R. LGBTQ parent concerns and parent–child communication about the Parental Rights in Education Bill (“Don’t Say Gay”) in Florida. Fam Relat. 2023;73(1):318–39. doi: 10.1111/fare.12894 [DOI] [Google Scholar]
- 62.Kuper LE, Cooper MB, Mooney MA. Supporting and Advocating for Transgender and Gender Diverse Youth and Their Families Within the Sociopolitical Context of Widespread Discriminatory Legislation and Policies. Clin Pract Pediatr Psychol. 2022;10(3):336–45. doi: 10.1037/cpp0000456 [DOI] [Google Scholar]
- 63.Wallace ER, O’Neill S, Lagdon S. Risk and protective factors for suicidality among lesbian, gay, bisexual, transgender, and queer (LGBTQ+) young people, from countries with a high global acceptance index (GAI), within the context of the socio-ecological model: A scoping review. J Adolesc. 2024;96(5):897–924. doi: 10.1002/jad.12308 [DOI] [PubMed] [Google Scholar]
- 64.Kuvalanka KA, Munroe C. The “second generation:” LGBTQ youth with LGBTQ parents. In: Goldberg AE, Allen KR, editors. LGBTQ-parent families: innovations in research and implications for practice. Cham: Springer International Publishing; 2020. p. 241–56. [Google Scholar]
- 65.Stone AL, Pride C, Adams B, Salcido R Jr. Bisexual Aunts, Gay Cousins: How LGBTQ Family Members Help LGBTQ Youth Navigate Family Heteronormativity. Socius. 2022;8:1–11. doi: 10.1177/23780231221117145 [DOI] [Google Scholar]
- 66.Bird JDP, Kuhns L, Garofalo R. The impact of role models on health outcomes for lesbian, gay, bisexual, and transgender youth. J Adolesc Health. 2012;50(4):353–7. doi: 10.1016/j.jadohealth.2011.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Strasser-Burke N, Symonds J. Who Do You Want to Be Like? Factors Influencing Early Adolescents’ Selection of Accessible and Inaccessible Role Models. J Early Adolesc. 2019;40(7):914–35. doi: 10.1177/0272431619880619 [DOI] [Google Scholar]
- 68.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–30. doi: 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barnes DM, Meyer IH. Religious affiliation, internalized homophobia, and mental health in lesbians, gay men, and bisexuals. Am J Orthopsychiatry. 2012;82(4):505–15. doi: 10.1111/j.1939-0025.2012.01185.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Berg RC, Ross MW, Weatherburn P, Schmidt AJ. Structural and environmental factors are associated with internalised homonegativity in men who have sex with men: findings from the European MSM Internet Survey (EMIS) in 38 countries. Soc Sci Med. 2013;78:61–9. doi: 10.1016/j.socscimed.2012.11.033 [DOI] [PubMed] [Google Scholar]
- 71.Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clin Psychol Rev. 2010;30(8):1019–29. doi: 10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- 72.Williams DY, Hall WJ, Dawes HC, Srivastava A, Radtke SR, Ramon M, et al. Relationships between internalized stigma and depression and suicide risk among queer youth in the United States: a systematic review and meta-analysis. Front Psychiatry. 2023;14:1205581. doi: 10.3389/fpsyt.2023.1205581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Szymanski DM, Kashubeck-West S, Meyer J. Internalized heterosexism: measurement, psychosocial correlates, and research directions. Couns Psychol. 2008;36(4):525–74. doi: 10.1177/0011000007309489 [DOI] [Google Scholar]
- 74.Puckett JA, Woodward EN, Mereish EH, Pantalone DW. Parental Rejection Following Sexual Orientation Disclosure: Impact on Internalized Homophobia, Social Support, and Mental Health. LGBT Health. 2015;2(3):265–9. doi: 10.1089/lgbt.2013.0024 [DOI] [PubMed] [Google Scholar]
- 75.Douglas BD, Ewell PJ, Brauer M. Data quality in online human-subjects research: Comparisons between MTurk, Prolific, CloudResearch, Qualtrics, and SONA. PLoS One. 2023;18(3):e0279720. doi: 10.1371/journal.pone.0279720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mayfield W. The development of an Internalized Homonegativity Inventory for gay men. J Homosex. 2001;41(2):53–76. doi: 10.1300/J082v41n02_04 [DOI] [PubMed] [Google Scholar]
- 77.Zimmerman M, Chelminski I, McGlinchey JB, Posternak MA. A clinically useful depression outcome scale. Compr Psychiatry. 2008;49(2):131–40. doi: 10.1016/j.comppsych.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 78.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. doi: 10.1037//0022-006x.56.6.893 [DOI] [PubMed] [Google Scholar]
- 79.PROMIS Health Organization and PROMIS Cooperative Group. PROMIS item bank v1.0 – alcohol: alcohol use – short form 7a. PROMIS Health Organization and PROMIS Cooperative Group; 2016. [Google Scholar]
- 80.Herek GM. Assessing heterosexuals’ attitudes toward lesbians and gay men: a review of empirical research with the ATLG scale. In: Greene B, Herek GM, editors. Lesbian and gay psychology: theory, research, and clinical applications. Thousand Oaks (CA): SAGE Publications, Inc.; 1994. p. 206–28. [Google Scholar]
- 81.Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: an interactive calculation tool for mediation tests [Internet]. 2001. [cited 2024 Jun 11]. Available from: https://quantpsy.org/sobel/sobel.htm [Google Scholar]
- 82.Ayhan CHB, Bilgin H, Uluman OT, Sukut O, Yilmaz S, Buzlu S. A Systematic Review of the Discrimination Against Sexual and Gender Minority in Health Care Settings. Int J Health Serv. 2020;50(1):44–61. doi: 10.1177/0020731419885093 [DOI] [PubMed] [Google Scholar]
- 83.Mustanski B, Andrews R, Puckett JA. The Effects of Cumulative Victimization on Mental Health Among Lesbian, Gay, Bisexual, and Transgender Adolescents and Young Adults. Am J Public Health. 2016;106(3):527–33. doi: 10.2105/AJPH.2015.302976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang C-C, Lin H-C, Chen M-H, Ko N-Y, Chang Y-P, Lin I-M, et al. Effects of traditional and cyber homophobic bullying in childhood on depression, anxiety, and physical pain in emerging adulthood and the moderating effects of social support among gay and bisexual men in Taiwan. Neuropsychiatr Dis Treat. 2018;14:1309–17. doi: 10.2147/NDT.S164579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pacilli MG, Taurino A, Jost JT, van der Toorn J. System Justification, Right-Wing Conservatism, and Internalized Homophobia: Gay and Lesbian Attitudes toward Same-Sex Parenting in Italy. Sex Roles. 2011;65(7–8):580–95. doi: 10.1007/s11199-011-9969-5 [DOI] [Google Scholar]
- 86.Baiocco R, Fontanesi L, Santamaria F, Ioverno S, Marasco B, Baumgartner E, et al. Negative Parental Responses to Coming Out and Family Functioning in a Sample of Lesbian and Gay Young Adults. J Child Fam Stud. 2014;24(5):1490–500. doi: 10.1007/s10826-014-9954-z [DOI] [Google Scholar]
- 87.Newcomb ME, LaSala MC, Bouris A, Mustanski B, Prado G, Schrager SM, et al. The Influence of Families on LGBTQ Youth Health: A Call to Action for Innovation in Research and Intervention Development. LGBT Health. 2019;6(4):139–45. doi: 10.1089/lgbt.2018.0157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Diamond LM, Alley J. Rethinking minority stress: A social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations. Neurosci Biobehav Rev. 2022;138:104720. doi: 10.1016/j.neubiorev.2022.104720 [DOI] [PubMed] [Google Scholar]
- 89.Roe S. “Family support would have been like amazing”: LGBTQ youth experiences with parental and family support. Fam J. 2016;25(1):55–62. doi: 10.1177/1066480716679651 [DOI] [Google Scholar]
- 90.Lau H. Sexual orientation and gender identity discrimination. In: Kjaran JI, Sauntson H, editors. Schools as queer transformative spaces: Global perspectives. Leiden: Brill; 2018. Available from: https://brill.com/display/title/34847 [Google Scholar]
- 91.Pierceson J. Same-sex marriage in the United States: the road to the Supreme Court and beyond. Lanham (MD): Rowman & Littlefield; 2014. [Google Scholar]
- 92.Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Educ Prev. 2004;16(4):328–40. doi: 10.1521/aeap.16.4.328.40397 [DOI] [PubMed] [Google Scholar]
- 93.Weber GN. Using to Numb the Pain: Substance Use and Abuse Among Lesbian, Gay, and Bisexual Individuals. J Ment Health Couns. 2008;30(1):31–48. doi: 10.17744/mehc.30.1.2585916185422570 [DOI] [Google Scholar]
- 94.Feinstein BA, Goldfried MR, Davila J. The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. J Consult Clin Psychol. 2012;80(5):917–27. doi: 10.1037/a0029425 [DOI] [PubMed] [Google Scholar]
- 95.Cain DN, Mirzayi C, Rendina HJ, Ventuneac A, Grov C, Parsons JT. Mediating Effects of Social Support and Internalized Homonegativity on the Association Between Population Density and Mental Health Among Gay and Bisexual Men. LGBT Health. 2017;4(5):352–9. doi: 10.1089/lgbt.2017.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lin C-Y, Griffiths MD, Pakpour AH, Tsai C-S, Yen C-F. Relationships of familial sexual stigma and family support with internalized homonegativity among lesbian, gay and bisexual individuals: The mediating effect of self-identity disturbance and moderating effect of gender. BMC Public Health. 2022;22(1):1465. doi: 10.1186/s12889-022-13815-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Andrzejewski J, Salgin L, Poteat VP, Yoshikawa H, Calzo JP. Gender-Sexuality Alliance Advisors’ Self-Efficacy to Address Transgender Issues: An Interpersonal Protective Factor for Transgender Student Depression. LGBT Health. 2023;10(4):296–305. doi: 10.1089/lgbt.2022.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–13. doi: 10.1111/j.1744-6171.2010.00246.x [DOI] [PubMed] [Google Scholar]
- 99.Knauer-Turner E. Sexual minorities’ internalized homophobia, experience of heterosexism, and use of humor. Thesis, University of La Verne. 2015. Available from: https://www.proquest.com/openview/249c3838771766f5bca66abfc70f6cb2/1?cbl=18750&pq-origsite=gscholar [Google Scholar]
- 100.Rosenberg A, Gates A, Richmond K, Sinno S. It’s not a joke: masculinity ideology and homophobic language. Psychol Men Masculinity. 2017;18(4):293–300. [Google Scholar]
- 101.Ruprecht MM, Floresca Y, Narla S, Felt D, Phillips G 2nd, Macapagal K, et al. “Being Queer, It Was Really Isolating”: Stigma and Mental Health Among Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ+) Young People During COVID-19. Health Educ Behav. 2024;51(4):521–32. doi: 10.1177/10901981241249973 [DOI] [PMC free article] [PubMed] [Google Scholar]