Abstract
Background
hip arthroplasties for the treatment of displaced femoral neck fractures in adults can be total replacement or hemiarthroplasty. Despite the large number of studies on the topic, the best choice of arthroplasty to be used remains unclear.
Objectives
overview the results of systematic reviews of randomized controlled trials (RCTs) comparing outcomes between total hip replacement and hemiarthroplasty for displaced femoral neck fractures in adults.
Design and Setting
The study followed the standards of the Prisma checklist and the Cochrane handbook.
Methods
Four electronic databases (Pubmed, Embase, Cochrane Library and Web of Science) were researched until January 2025. The primary outcomes were mortality, function, quality of life and revision rate and the secondary ones: dislocation, periprosthetic fracture, infection, and surgical time. Comparisons of dichotomous data were reported as the OR and 95% CI, and comparisons of functional and health related quality of life outcomes were reported as the mean difference and 95% CI.
Results
twenty systematic reviews with a total of 29,980 patients were analyzed. Patients with total hip arthroplasty had a lower revision rate (RR 0.67, 95% CI 0.48 to 0.93; participants = 4078; studies = 22; I2 = 30%), better early function (SMD 0.59, 95% CI 0.04 to 1.08; participants = 963; studies = 12; I2 = 87%) and better quality of life (DM 0.05, 95% CI 0.03 to 0.08; participants = 1240; studies = 6; I2 = 28%). There was no difference regarding dislocation, infection, periprosthetic fracture and mortality. Surgical time was shorter in hemiarthroplasty (DM 20.46, 95% CI 12.12 to 28, 80; participants = 1493; studies = 16; I2 = 95%).
Conclusion
Total hip arthroplasty had a lower revision rate, better quality of life and function. The surgical time was on average 20 min shorter in hemiarthroplasty. Mortality, dislocation, infection, and periprosthetic fracture rates were similar.
Systematic Review Registration
(CRD42021237885), and published in August 2021 (https://bmjopen.bmj.com/content/11/11/e051840.long).
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-025-06144-w.
Keywords: Femoral neck fracture, Hip arthroplasty, Revision rate, Quality of life, Function
Background
Hip arthroplasties for the treatment of displaced femoral neck fractures in patients aged 50 years and above can be either total or hemiarthroplasty. Despite the high prevalence of these fractures and the numerous published systematic reviews on the topic, the most effective method of arthroplasty remains controversial [1].
Total hip arthroplasty may offer advantages in terms of hip function and improved patient quality of life. However, compared hemiarthroplasty, this technique has a longer surgical time and a higher reported incidence of dislocation in the current literature. Dislocation requires additional procedures such as closed reduction or prosthesis revision, may leading to increased health costs morbidity and mortality. Hemiarthroplasty is more reproducible because its training is widely available in orthopaedic trauma services, making it globally prevalent [2–5].
A large and significant multicentre study called HEALTH [6] compared total hip and hemiarthroplasty for the treatment of displaced femoral neck fractures in patients aged 50 years and above. This robust randomized clinical trial involved 1495 patients from 80 participating hospitals in 10 countries. The primary outcome of this study was the frequency of an unplanned additional procedure within 24 months postoperatively, with the belief that the results would resolve the clinical uncertainty regarding the choice of the optimal procedure. However, in a 2020 editorial comment, Judge et al. raised concerns about the HEALTH study, particularly regarding the chosen primary outcome, which was not related to the patient’s functional aspect but rather the need for an unplanned additional procedure. It is known that the most relevant outcomes in hip fractures are mortality, pain, ability to resume activities of daily living, mobility, and quality of life. Furthermore, despite the robust case series, the study had a relatively short follow-up period for comparing hip arthroplasty outcomes (24 months), and it did not demonstrate statistical differences in the analysed outcomes.
The comparative effectiveness of total hip arthroplasty (THA) versus hemiarthroplasty for the treatment of displaced femoral neck fractures in elderly patients remains a subject of ongoing debate, with conflicting evidence emerging from systematic reviews. While some studies suggest that THA may offer superior functional outcomes and lower cumulative revision rates, others report significantly higher dislocation rates or comparable long-term survivorship between the two procedures. Notably, the lack of consensus persists even in recent high-quality meta-analyses, particularly regarding dislocation risk and cumulative revision rates [7, 8]. This uncertainty can lead to poorer patient outcomes and increased costs for healthcare systems. Therefore, this overview review aims to establish the most effective approach in this relevant and common clinical issue.
Methods
This study is an overview of systematic reviews, strictly adhering to the ethical guidelines. It was approved by the ethics committee of university (document number 6987100920). The study protocol was registered in the PROSPERO platform (International Prospective of Systematic Review - CRD42021237885), linked to the National Institute for Health Research (NHS).
Clinical question
The clinical question was formulated according to the PICOS [9] strategy:
Population: patients aged over 50 years with displaced femoral neck fractures.
Intervention: total hip arthroplasty.
Control: hemiarthroplasty.
Primary Outcomes (critical): revision rate, mortality, function, and quality of life.
Secondary Outcomes (important): complications (dislocations, periprosthetic fractures, infection), cost-effectiveness, and surgical procedure duration.
Study Type: systematic review (overview).
Study design
The study was conducted following the methodology described in the Cochrane Handbook for Systematic Reviews of Overviews [10] and the Preferred Reporting Items for Systematic Reviews (PRISMA) checklist (appendix 2) [11]. The search was performed in four databases: PubMed (1966-January 2025), Embase (1973-January 2025), Cochrane Library (1995-January 2025), and Web of Science (2000-January 2025), with no language restrictions. The search strategy was developed by the research group (appendix 1).
Inclusion criteria
The following systematic reviews of randomized clinical trials with meta-analysis were included:
Comparatively assessed total hip arthroplasty versus hemiarthroplasty in the treatment of displaced femoral neck fractures in adults aged over 50 years, of both sexes, who were able to ambulate before the fracture and did not present severe cognitive impairment (capable of performing activities of daily living independently).
Systematic reviews of randomized clinical trials with meta-analysis on the overall treatment of femoral neck fractures, where at least one study arm compared total hip arthroplasty versus hemiarthroplasty in the treatment of displaced femoral neck fractures in adults (only relevant data for this review were extracted).
Exclusion criteria
The following reviews were excluded:
Non-systematic reviews (narrative reviews, data syntheses from national arthroplasty registries), identified through the reading of the title, abstract, or full text.
Other types of studies on the topic.
Outcomes
Primary outcomes
Revision rate: the percentage of patients who required a reoperation with replacement of at least one prosthetic component.
Mortality: the percentage of deaths in each group of patients during follow-up.
Function: assessed by the validated Harris Hip Score [12] and OXFORD [13] scales, providing data on hip function, with scores ranging from 0 (severe) to 100 (good function).
Quality of life: assessed by the EQ-5D [14] a generic quality of life questionnaire that covers 5 health domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with 3 response levels and a visual analogic scale (VAS), ranging from 0 (severe) to 100 (no impairment in quality of life).
Secondary outcomes
Described complications: the rate of dislocation, infection, and periprosthetic fracture in each group.
Cost-effectiveness of each arthroplasty modality.
Average duration in minutes of the surgical procedure in each group.
Analysis of included studies
The selection and analysis of studies were performed by two evaluators independently, with doubts resolved through consensus. The supervising professor was consulted in cases of final decisions regarding study inclusion.
All outcomes were described according to the recommendation grade and level of evidence defined by the GRADE system [15]. The level of evidence represents the confidence in the information obtained and is classified as high, moderate, low, or very low.
Data extraction
Data extraction and management were carried out independently by two authors (GF and FM) using a form in Microsoft Access/Excel, version 16.34.2020. The extracted data included the study design, author information, patient characteristics (number of patients and inclusion/exclusion criteria), interventions (number of hips in each group and intervention description), outcome measures (types, scale, measurement unit), and relevant study design information. The data were extracted directly from the included systematic reviews and meta-analyses, with particular attention paid to preventing the duplication of primary study data (overlap). Where necessary, we cross-referenced the original studies to verify the accuracy of reported outcomes, especially in cases where data were not explicitly detailed in the systematic review.
Treatment effect measures
For continuous outcomes, means, standard deviations, and the number of participants in each intervention group were extracted. Data were summarized using generic inverse variance or inverse of variance meta-analysis and random-effects models. For outcomes presented in different measurement units, standardized mean difference (SMD) with standard error (SE) for each study was used, and then the data were expressed as SMD with a 95% confidence interval (CI). For dichotomous outcomes, the number of events and the number of participants in each intervention group were extracted, and the risk ratio (RR) was summarized with a 95% CI using random-effects meta-analysis. In case of disagreements, conflicts were resolved through consensus, and the data were analysed using Cochrane Review Manager software (V.5.3) with the assistance of a statistician specialized in systematic reviews.
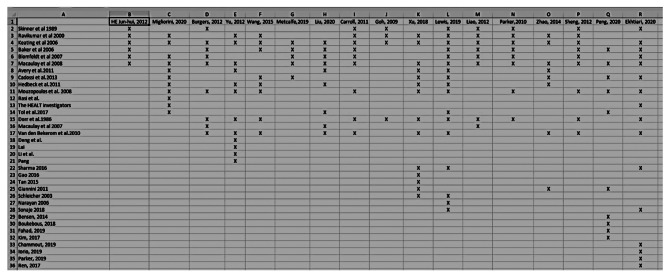
A potential bias in overview systematic reviews is the overlap of data from primary studies, which can result in increased statistical power in meta-analysis. To assess this overlap, we used the table model proposed by PIPER et al. [16]:
Equation: N-r / rc– r.
N: number of publications (including duplicates).
r: number of rows.
c: number of columns.
Values above 10% indicate high overlap. In this study, the overlap was 23%, which guided the individual selection of data from primary studies for each evaluated outcome (Table 1 - Schematic representation of the overlapping table of primary studies: X axis is systematic reviews and Y axis is clinical trials. The final overlapping was: 214–39 / (20 × 39)– 39 = 0,23).
Table 1.
Schematic representation of the overlapping table of primary studies: X axis is systematic reviews and Y axis is clinical trials. The final overlapping was: 214–39 / (20 × 39)– 39 = 0,23
Handling of missing data
When necessary, we contacted the authors of the included studies to obtain missing data or characteristics. Data were extracted based on the intention-to-treat analysis or modified intention-to-treat analysis, following the premises defined by the study authors. If the data were not available or the authors did not respond, only the analysis with the available data was performed. The impact of including these studies in the overall assessment was explored through sensitivity analyses. For continuous data, the standardized mean difference was calculated based on the number of patients analysed in the longest available follow-up.
Assessment heterogeneity
Clinical heterogeneity was assessed considering participants, interventions, outcomes, and characteristics of the included studies. Statistical heterogeneity was assessed visually through forest plots and the Chi [2] test, using a p-value less than 0.1 as an indicator of the presence of heterogeneity. The I [2] statistic was used to describe the proportion of variation in effect estimates due to variability between studies. The interpretation thresholds were according to the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions [10]:
0–40%: heterogeneity may not be important.
30–60%: heterogeneity may represent moderate heterogeneity.
50–74%: heterogeneity may represent substantial heterogeneity.
75–100%: considerable heterogeneity.
Assessment of reporting bias
An investigation of publication bias was planned to use a funnel plot if at least ten studies were included in one or more meta-analyses. Separate statistical analyses were conducted to check for possible influence of publication bias on the results of the systematic review.
Data synthesis
Meta-analyses were conducted when more than one clinical trial was included in each comparison. Studies were grouped in the meta-analysis only if participants, interventions, and outcomes were sufficiently like allow combination. The analyses followed the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions [10]. For continuous outcomes, the effect measures used were the mean difference (MD) or the standardized mean difference (SMD), using generic inverse variance or inverse of variance methods and random-effects models. For dichotomous outcomes, the risk ratio (RR) was used in random-effects meta-analyses (inverse variance or generic inverse variance method - the DerSimonian and Laird random-effects model and Hartung-Knapp adjustment were applied for all meta-analyses, with I² and Cochran’s Q-test used to quantify and test for statistical heterogeneity, respectively).
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were performed, when possible, to investigate possible sources of heterogeneity in the meta-analyses, following the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions [10].
Sensitivity analysis
Sensitivity analyses were conducted to assess the influence of each study on the results. Consistent results in direction, effect size, and statistical significance indicate robustness of the findings. The analyses were conducted following the recommendations of The Cochrane Handbook for Systematic Reviews of Interventions [10].
Results
Systematic literature search result
The literature search was conducted up to January 2025, resulting in the selection of 261 studies from four search platforms: PubMed (166 studies), Embase (53 studies), Cochrane Library (16 studies), and Web of Science (26 studies). All 261 studies were evaluated by two authors (GF and FM), and initially, 205 duplicate studies were excluded, along with 29 studies that did not meet the inclusion criteria based on title and abstract reading. Out of the remaining 27 studies, six studies were further excluded upon full-text reading as they included data from retrospective studies. Therefore, 21 systematic reviews were selected for the final analysis and data extraction. The selected systematic reviews were: GOH et al. (2009); PARKER, GURUSAMY & AZEGAMI (2010); CARROLL et al. (2011); BURGERS et al. (2012); HE et al. (2012); LIAO et al. (2012); SHENG et al. (2012); YU, WANG & CHEN (2012); ZHAO et al. (2014); WANG et al. (2015); XU et al. (2018); LEWIS et al. (2019); METCALFE et al. (2019); LIU et al. (2020); EKHTIARI et al. (2020); MIGLIORINI et al. (2020); PENG et al. (2020); TANG et al. (2020); LEWIS et al. (2022); WEK et al. (2022) and RAMADANOV et al. (2023) The flowchart of article evaluation is described in the Fig. 1 (PRISMA 2020 systematized search strategy flowchart.)
Fig. 1.
PRISMA 2020 systematized search strategy flowchart
Characteristics of included studies
All data were extracted from systematic reviews of randomized clinical trials that compared the outcomes of THA (total hip arthroplasty) with hemiarthroplasty for the treatment of femoral neck fractures in functional independent patients over 50 years old.
Participant casuistry and data management
A total of 34,398 patients were identified in the 21 systematic reviews. However, due to data overlap among the reviews, it was necessary to extract the data individually to avoid statistical bias (“phantom patients”). Information from the included randomized clinical trials was obtained from the systematic reviews and was cross-referenced with the original primary studies. Any doubts were sent to the corresponding author of the original study before including the data in the meta-analysis. After removing the repeat patients, the final sample was 5669 patients (50% from Europe, 11% from North America and 39% from the Asian continent).
Evaluation of bias risk in included studies
The risk of bias for each systematic review was assessed following the ROBIS (Risk of Bias in Systematic Reviews) methodology described by Whiting et al. [17] and was described individually for each study analysed. The final configuration of the systematic reviews stratified by risk of bias is illustrated in Table 2- risk of bias of systematic reviews (ROBIS).
Table 2.
Risk of bias of systematic reviews (ROBIS)
| HIGH | LOW |
|---|---|
| Goh, 2009 | Parker, 2010 |
| He, 2019 | Carroll, 2011 |
| Liao, 2012 | Burguers, 2012 |
| Sheng, 2012 | Yu, 2012 |
| Zhao, 2014 | Lewis, 2019 |
| Wang, 2015 | Ekhtiari, 2020 |
| Xu, 2018 | Liu, 2020 |
| Metcalfe, 2019 | Tang, 2020 |
| Migliorini, 2020 | Lewis, 2022 |
| Peng, 2020 | |
| Wek, 2022 |
Total hip arthroplasty compared to hemiarthroplasty
Revision rate
A total of 22 studies were found in the systematic reviews, totalling 4078 participants for this outcome. Total hip arthroplasty resulted in a reduction in the revision rate compared to hemiarthroplasty (RR 0.67, 95% CI 0.48 to 0.93; participants = 4078; studies = 22; I2 = 30%)– Fig. 2 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: revision rate).
Fig. 2.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: revision rate
Mortality
A total of 25 studies were found in the systematic reviews, totalling 4,618 participants for this outcome. Total hip arthroplasty did not show a difference in the mortality rate compared to hemiarthroplasty (RR 0.94, 95% CI 0.81 to 1.09; participants = 4,618; studies = 25; I2 = 9%)– Fig. 3 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: mortality).
Fig. 3.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: mortality
Function
A total of 12 studies were found in the systematic reviews, totalling 963 participants for this outcome, assessed by the Harris Hip Score (HHS) and Oxford Hip Score (OHS) instruments. Total hip arthroplasty showed better results in terms of function compared to hemiarthroplasty (SMD 0.59, 95% CI 0.11 to 1.08; participants = 963; studies = 12; I2 = 87%)– Fig. 4 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: function). Subgroup analyses reduced heterogeneity in hip function outcomes from 87 to 62% when stratified by assessment tool (HHS: SMD 0.68, 95% CI 0.20–1.16, I² = 78%; OHS: SMD 0.42, 95% CI − 0.05 to 0.89, I² = 45%), suggesting measurement instrument differences partially explain variability. After Hartung-Knapp adjustment CI widened and includes near-zero values (0.04), suggesting the functional benefit of THA (measured by HHS) may not be robust when accounting for high heterogeneity. Further stratification by follow-up time showed sustained THA had no benefits at 1 year (SMD 0.54, I² = 58%, CI -0.17-1.25).
Fig. 4.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: function
Quality of life
Six studies were found among the systematic reviews, including 1240 participants for this outcome (assessed using the EuroQol-5 Dimensions (EQ-5D) instrument, 0–1; higher = better). Total hip arthroplasty resulted in better quality of life compared to hemiarthroplasty (MD 0.05, 95% CI 0.03 to 0.08; participants = 1240; studies = 6; I2 = 28%)– Fig. 5 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: quality of life).
Fig. 5.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: quality of life
Dislocation rate
Twenty-nine studies were found among the systematic reviews, including 5038 participants for this outcome. Total hip arthroplasty had a similar dislocation rate compared to hemiarthroplasty (RR 1.25, 95% CI 0.81 to 1.91; participants = 5038; studies = 29; I2 = 47%)– Fig. 6 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: dislocation rate).
Fig. 6.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: dislocation rate
Surgical time
Sixteen studies were found among the systematic reviews, including 1493 participants for this outcome. Total hip arthroplasty showed an increase in surgical time by an average of 20 min compared to hemiarthroplasty (MD 20.46, 95% CI 12.12 to 28.80; participants = 1493; studies = 16; I2 = 95%).– Fig. 7 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: surgical time). The high heterogeneity (I² = 95%) in surgical time outcomes was explored via sensitivity/subgroup analyses. Exclusion of high-bias studies reduced heterogeneity to 85%, while stratification by surgical approach revealed consistent THA time increases (MD 18–22 min) across subgroups, suggesting clinical variability is a key driver.
Fig. 7.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: surgical time
Periprosthetic fracture rate
Nine studies were found among the systematic reviews, including 2190 participants for this outcome. Total hip arthroplasty did not show a difference in the rate of periprosthetic fracture compared to hemiarthroplasty (RR 1.13, 95% CI 0.74 to 1.72; participants = 2190; studies = 9; I2 = 0%)– Fig. 8 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: periprosthetic fracture rate).
Fig. 8.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: periprosthetic fracture rate
Periprosthetic infection rate
Thirteen studies were found among the systematic reviews, including 1650 participants for this outcome. Total hip arthroplasty did not show a difference in the rate of periprosthetic infection compared to hemiarthroplasty (RR 1.54, 95% CI 0.77 to 3.08; participants = 1650; studies = 13; I2 = 0%)– Fig. 9 (forest plot of the comparison total hip replacement versus hemiarthroplasty, outcome: periprosthetic infection rate).
Fig. 9.
Forest plot of the comparison total hip replacement versus partial replacement, outcome: periprosthetic infection rate
Table of main findings
Key findings are summarized in the table below using the GRADE approach accompanied by evidence certainty assessments - Table 3 (table of main findings with grades of evidence).
Table 3.
Table of main findings with grades of evidence
| Total arthroplasty compared to partial arthroplasty for patients with displaced femoral neck fractures | ||||||
|---|---|---|---|---|---|---|
|
Patient or population: patients > 50 yo with displaced femoral neck fractures Context: Hospital Intervention: total hip arthroplasty Comparison: hemiarthoplasty | ||||||
|
Outcome Number of participants (studies) |
Relative effect (CI 95%) |
Potential XXXemiarth effects (CI 95%) | Certainty of evidence | Results | ||
| Hemiarthoplasty | Total hip arthroplasty | Difference | ||||
|
Revision Rate Nº of participants = 4078 (22 RCTs) |
RR 0.67 (0.48 to 0.93) |
9.3% |
6.2% (4.5 to 8.6) |
3.1% (4.8 to 0.6) |
⨁⨁⨁◯ Moderatea |
Total arthroplasty results in a reduction in the revision rate. |
|
Mortality Nº of participants = 4618 (25 RCTs) |
RR 0.94 (0.81 to 1.09) |
19.5% |
18.4% (15.8 to 21.3) |
1.2% (3.7 to 1.8) |
⨁⨁⨁⨁ High |
Total hip arthroplasty shows no difference in the mortality rate. |
|
Function (HHS and Oxford) Nº of participants = 963 (12 RCTs) |
- | The average function was 71.9 points | - |
MD 7.49 more (1.4 to 13.7) |
⨁◯◯◯ Very lowa, c |
Total hip arthroplasty showed better early function, but the evidence is very uncertain. SMD = 0.59 (95% CI 0.04 to 1.08). |
|
Quality of life (EuroQol-5 Dimensions) № of participants: 1240 (6 RCTs) |
- | The mean quality of life ranged from 0.53 to 0.80 units | - | MD 0.05 units more (0.03 more to 0.08 more) |
⨁⨁⨁⨁ High |
Total hip arthroplasty results in a better quality of life. |
|
Dislocation rate № of participants: 5038 (29 RCTs) |
RR 1.25 (0.81 to 1.91) |
4,4% |
5.5% (3.5 to 8.3) |
1,1% mais (0,8 menos para 4 mais) |
⨁⨁◯◯ Lowd, e |
Total hip arthroplasty shows no difference in the rate of prosthetic dislocation. |
|
Surgical time № of participants: 1493 (16 RCTs) |
- | The mean surgical time ranged from 35 to 125.3 min | - |
MD 20.46 min (12.12 to more) |
⨁⨁◯◯ Lowf |
Total hip arthroplasty may increase surgical time slightly. |
|
Periprosthetic Fracture Rate № of participants: 2190 (9 RCTs) |
RR 1.13 (0.74 to 1.72) |
3.5% |
3.9% (2.6 para 6) |
0.5% (0,9 to 2,5) |
⨁⨁⨁◯ Moderateg |
Total hip arthroplasty does not show a difference in the periprosthetic fracture rate. |
|
Periprosthetic Infection Rate № of participants: 1650 (13 RCTs) |
RR 1.54 (0.77 to 3.08) |
1.5% |
2.3% (1.1 to 4.5) |
0.8% (0.3 to 3.1) |
⨁⨁⨁◯ Moderateg |
Total hip arthroplasty does not show a difference in the periprosthetic infection rate. |
* The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk of the comparator group and the relative effect of the intervention (and its 95% CI)
CI: Confidence interval; MD: Mean difference; RCT: Randomized clinical trial; RR: Relative risk
GRADE Working Group grades of evidence
High certainty: High confidence that the true effect is close to the estimate
Moderate certainty: Moderate confidence in the effect estimate: the actual effect is likely to be close to the effect estimate, but there is a possibility that it will be substantially different
Low certainty: Confidence in the effect estimate is limited: the true effect may be substantially different from the effect estimate
Very low certainty: Very little confidence in the effect estimate: The true effect is likely to be substantially different from the effect estimate
Discussion
The present overview on the treatment of displaced fractures of the femoral neck in adults, comparing total hip arthroplasty with hemiarthroplasty, analysed 21 systematic reviews (SRs) of randomized controlled trials (RCTs) involving initially a total of 34,398 patients. Critical analysis of these studies was conducted, and statistical analysis prevented the overlap of clinical trial data, as they were commonly repeated across various SRs.
This is the first systematic review that demonstrate that total hip arthroplasty (THA) exhibited a lower revision rate compared to hemiarthroplasty, improved early function (< 1 year follow-up) and quality of life as measured by the EQ-5D questionnaire without differences in mortality, dislocation rate, infection, periprosthetic fracture, and ambulatory capacity. These data are significant as they demonstrate that THA was superior in patient-reported outcomes and exhibited reduced future need for revision surgery without an increase in complications. Therefore, active patients, independent in daily activities and with satisfactory life expectancy can likely benefit in the long term from THA treatment. A valuable tool for assessing the expected survival of a patient with a femoral neck fracture involves the application of the Charlson comorbidity index, as introduced by Charlson et al. [18] This index estimates the patient’s 10-year survival based on epidemiological factors and patient comorbidities. Schnell et al. [19] found, through multivariate analysis of mortality-related risk factors in hip fracture patients, that a Charlson score of 4 or higher was a significant predictor of death within 1 year of the surgical procedure. This comorbidity score can be calculated online at https://www.mdcalc.com/charlson-comorbidity-index-cci (MDCalc® 2005–2023).
In 2019, Bhandari et al. [2] published the largest comparative RCT between total and hemiarthroplasty for treating displaced femoral neck fractures in patients over 50 years old. The study involved 80 participating hospitals with over 95% of surgeons meeting minimum surgical training criteria for the proposed technique. The primary outcome was the need for an unplanned additional procedure (closed or open) up to the final follow-up time (24 months). The study included 1495 patients (749 THA and 746 HA), of which 1243 survived beyond the 24-month mark. There was no difference in the primary outcome between the groups; however, contrary to the current overview, a higher dislocation rate was found in the THA group.
In 2020, Ekhtiari et al. [7] conducted a systematic literature review (with low bias risk according to the ROBIS scale) comparing THA and HA in displaced femoral neck fractures. Their search was conducted in 2019, and they found no differences in functional scores and revision rates between the groups. The results of pooled functional data from 6 RCTs (n = 1,022) showed a non-significant trend favouring THA (MD = 3.06, 95% CI: −0.37 to 6.49). The mean difference was below the minimally important difference (MID) of 8 points for HHS. The risk difference (RD) suggested an 8% higher chance of achieving MID with THA, but the CI overlapped no effect (95% CI: −3.6–19.6%). Possible interpretations for these findings include lack of clinical significance (the marginal functional benefit of THA (3.06 points) is unlikely to be perceptible to patients); outcome tool variability (studies used HHS, WOMAC, or Hip Rating Questionnaire); follow-up duration (function was assessed at 1–3 years; longer follow-up might reveal THA’s durability advantages). Regarding the cumulative revision rate, twelve RCTs (n = 2,590) demonstrated no significant difference in revision rates between THA and HA at 1–5 years (OR = 0.89, 95% CI: 0.66–1.20, p = 0.44), with no heterogeneity (I² = 0%). Sensitivity analyses excluding studies with atypical revision definitions (e.g., closed reductions) yielded similar results. Points to be considered about this topic was that earlier meta-analyses suggested THA reduced revisions, but this study’s inclusion of the HEALTH trial (which contributed 58% of the weight) neutralized this effect and the shorter follow-up (most trials had ≤ 5-year data; THA’s theoretical long-term advantages may not yet be evident). Our study, in a wider approach showed lower cumulative revision rate in THA.
In a 2022 Cochrane systematic review (with low bias risk according to the ROBIS scale), Lewis et al. [8] included 3232 patients in a comparative analysis of THA and hemiarthroplasty, finding no differences in revision rates, function, and quality of life between the groups. However, they found a double dislocation rate in the THA group (12 studies, 2719 participants), which contrasts with the findings of the current review. This difference may be attributed to the difficulty in stratifying the surgical approach, femoral head size, and surgeon’s experience level.
In 2023, Tohidi, Mann & Groome [20] conducted a large cross-sectional study with data from 49,597 patients, assessing the preferences of surgeons and healthcare services in treating femoral neck fractures in patients over 60 years old. They found that 9.4% of patients (n = 4638) were treated with THA, and the determining factors for this choice were younger age, male gender, and prior diagnosis of rheumatoid arthritis. However, institutionalized patients with prior diagnosis of dementia or multiple comorbidities preferred hemiarthroplasty. The higher surgical volume in THA in the year preceding the surgery was the main factor associated with choosing THA as the treatment method. This finding supports the present overview’s results, as younger patients with greater life expectancy can benefit from THA, considering the lower future revision rate.
Ramadanov et al. (2023) [21] compared THA and HA in patients with displaced femoral neck fractures. Key findings include: Functional Outcomes (Harris Hip Score, HHS) - THA consistently outperformed HA at all follow-up intervals (≤ 6 months, 12 months, 2 years, and 3–5 years postoperatively), with statistically significant differences favouring THA (e.g., HHS at 12 months: THA 81.7 vs. HA 75.2, MD − 4.33, 95% CI − 7.05 to − 1.61); Quality of Life (EQ-5D) - THA ranked first, with HA second, particularly at 2 years postoperatively (THA 0.7 vs. HA 0.6, MD − 0.09, 95% CI − 0.17 to − 0.02); Reoperation Risk - no significant difference was observed between THA (6.36%) and HA (9.11%) (OR = 1.60, 95% CI 0.89–2.89); Dislocation Risk - HA had a 52% lower risk of dislocation compared to THA (3.11% vs. 6.33%, OR = 0.48, 95% CI 0.28–0.81); Mortality and Complications - no significant differences were noted in mortality, infection, or intraoperative fracture rates. Some findings differ from the present study, particularly the discrepancy in the dislocation rate.
The primary limitation of the current study is the lack of robust data for patients with longer follow-up times (> 5 years). This limitation is understandable due to the high mortality rate of femoral neck fracture patients, as well as the social challenges that family members face in maintaining adherence to ambulatory follow-up for elderly and clinically weakened patients.
In conducting a comparative study on two modalities of hip arthroplasty in patients with femoral neck fractures, several limitations must be acknowledged to ensure a comprehensive understanding of the findings. Firstly, the study did not account for the variations in prosthesis types used. Different hip prostheses can significantly impact patient outcomes, including factors such as longevity, complication rates, and overall functional recovery. The absence of this consideration means that the results may not fully capture the nuances associated with each type of prosthesis. Secondly, the experience level of the surgical team and the specific healthcare service where the procedures were performed were not evaluated. The proficiency and expertise of the surgeons, as well as the operational efficiency of the healthcare facility, can play a critical role in the success of hip arthroplasty. Variations in surgical technique, decision-making during surgery, and perioperative management are all influenced by the experience and skill of the medical professionals involved. Consequently, these variables could introduce significant bias and variability into the study outcomes.
As for future perspectives, evaluating different types of arthroplasties, such as the double mobility acetabular prosthetic system, which offers potential functional advantages and lower revision rates than conventional THA, while also reducing the risk of dislocation, requires larger RCTs and cost-effectiveness analyses to better define their role in femoral neck fracture treatment. Another notable point is the potential development of a clinical-epidemiological score for femoral neck fracture patients, aiming to stratify these patients in advance and determine, with reduced likelihood of error, the best arthroplasty modality case by case.
Conclusion
Total hip arthroplasty (THA) appears to be a more favourable treatment option compared to hemiarthroplasty for displaced femoral neck fractures in functional independent adults over 50 years old. THA demonstrated a lower revision rate, better quality of life and minimal improvement in function during the first postoperative year compared to hemiarthroplasty. Additionally, no significant differences were observed in terms of mortality, dislocation rate, infection, periprosthetic fracture, and ambulatory capacity between the two procedures.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Special thanks to the members of the Research Group of the Evidence-Based Orthopaedics Centre at the Escola Paulista de Medicina.
Author contributions
GGF, FTM and VYM carried out the checking, review and selection of the articles. They wrote the main manuscript text.JSF, FF, MJST and JCB conceptualised the methodology and the writing of the paper.MSG prepared figures.All authors reviewed the manuscript.
Funding
There is no funding source.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was approved by the local ethics committee by number (CEP 6987100920). As this is a secondary study (systematic review), there was no direct manipulation of patient data and therefore there was no requirement to apply a participation consent form.
Competing interests
The authors declare no competing interests.
Clinical trial number
not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–62. [DOI] [PubMed] [Google Scholar]
- 2.Lewis DP, Wæver D, Thorninger R, Donnelly WJ, Schemitsch EH. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: a systematic review and meta-analysis. J Arthroplasty. 2019;34(8):1837–43. [DOI] [PubMed] [Google Scholar]
- 3.Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J. 2016;98–B(3):291–7. [DOI] [PubMed] [Google Scholar]
- 4.Hansson S, Bülow E, Garland A, Kärrholm J, Rogmark C. More hip complications after total hip arthroplasty than after hemi-arthroplasty as hip fracture treatment: analysis of 5,815 matched pairs in the Swedish hip arthroplasty register. Acta Orthop. 2020;91(2):133–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gjertsen JE, Fenstad AM, Leonardsson O, Engesæter LB, Kärrholm J, Furnes O, Garellick G, Rogmark C. Hemiarthroplasties after hip fractures in Norway and sweden: a collaboration between the Norwegian and Swedish National registries. Hip Int. 2014 May-Jun;24(3):223–30. [DOI] [PMC free article] [PubMed]
- 6.Bhandari HEALTHI, Einhorn M. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381(23):2199–208. [DOI] [PubMed] [Google Scholar]
- 7.Ekhtiari S, Gormley J, Axelrod DE, Devji T, Bhandari M, Guyatt GH. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fracture: A systematic review and Meta-Analysis of randomized controlled trials. J Bone Joint Surg Am. 2020;102(18):1638–45. [DOI] [PubMed] [Google Scholar]
- 8.Lewis SR, Macey R, Parker MJ, Cook JA, Griffin XL. Arthroplasties for hip fracture in adults. Cochrane Database Syst Rev. 2022;2(2):CD013410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12–3. [PubMed] [Google Scholar]
- 10.Pollock M, Fernandes RM, Becker LA et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 Cochrane, 2022.
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–55. [PubMed] [Google Scholar]
- 13.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–90. [PubMed] [Google Scholar]
- 14.van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–15. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt GH, Oxman AD, Vist GE, et al. GRADE working group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75. [DOI] [PubMed] [Google Scholar]
- 17.Whiting P, Savović J, Higgins JP, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 19.Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1(1):6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tohidi M, Mann SM, Groome PA. Total hip arthroplasty versus hemiarthroplasty for treatment of femoral neck fractures: a population-based analysis of practice variation in ontario, Canada. Bone Joint J. 2023;105–B(2):180–9. [DOI] [PubMed] [Google Scholar]
- 21.Ramadanov N, Jóźwiak K, Hauptmann M, Lazaru P, Marinova-Kichikova P, Dimitrov D, Becker R. Cannulated screws versus dynamic hip screw versus hemiarthroplasty versus total hip arthroplasty in patients with displaced and non-displaced femoral neck fractures: a systematic review and frequentist network meta-analysis of 5703 patients. J Orthop Surg Res. 2023;18(1):625. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.