Abstract
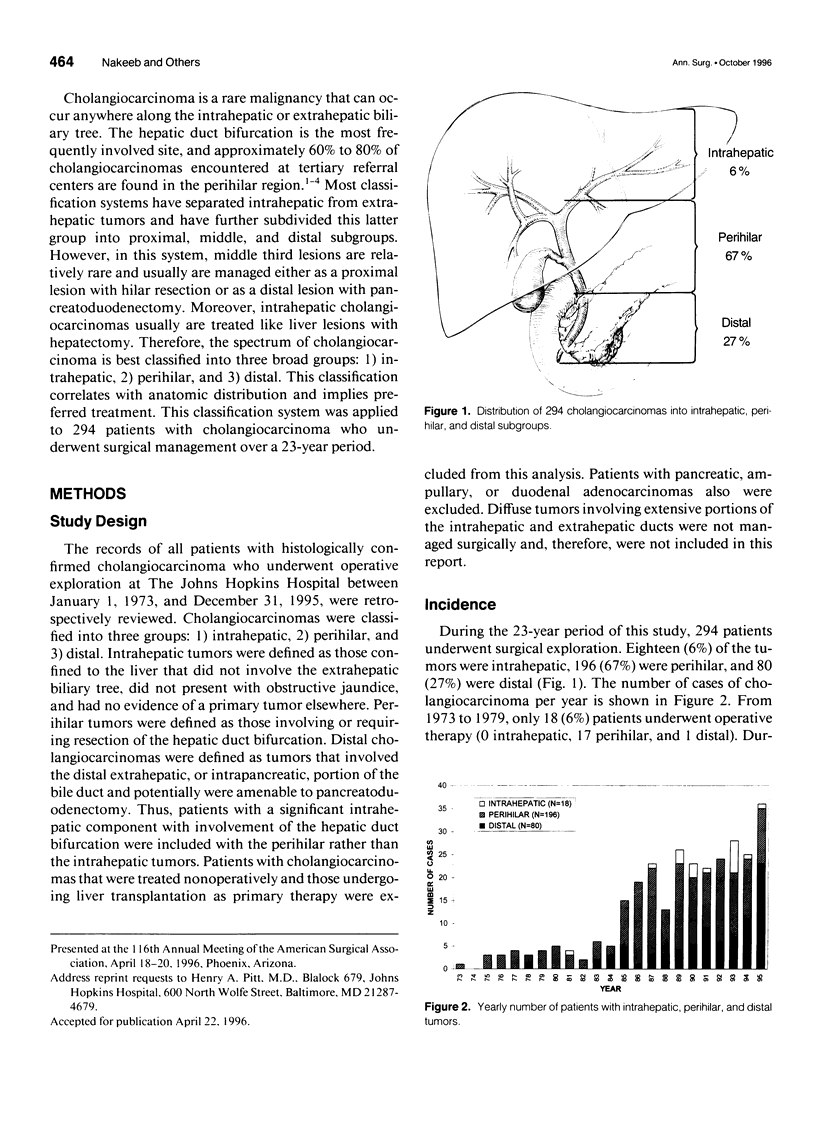
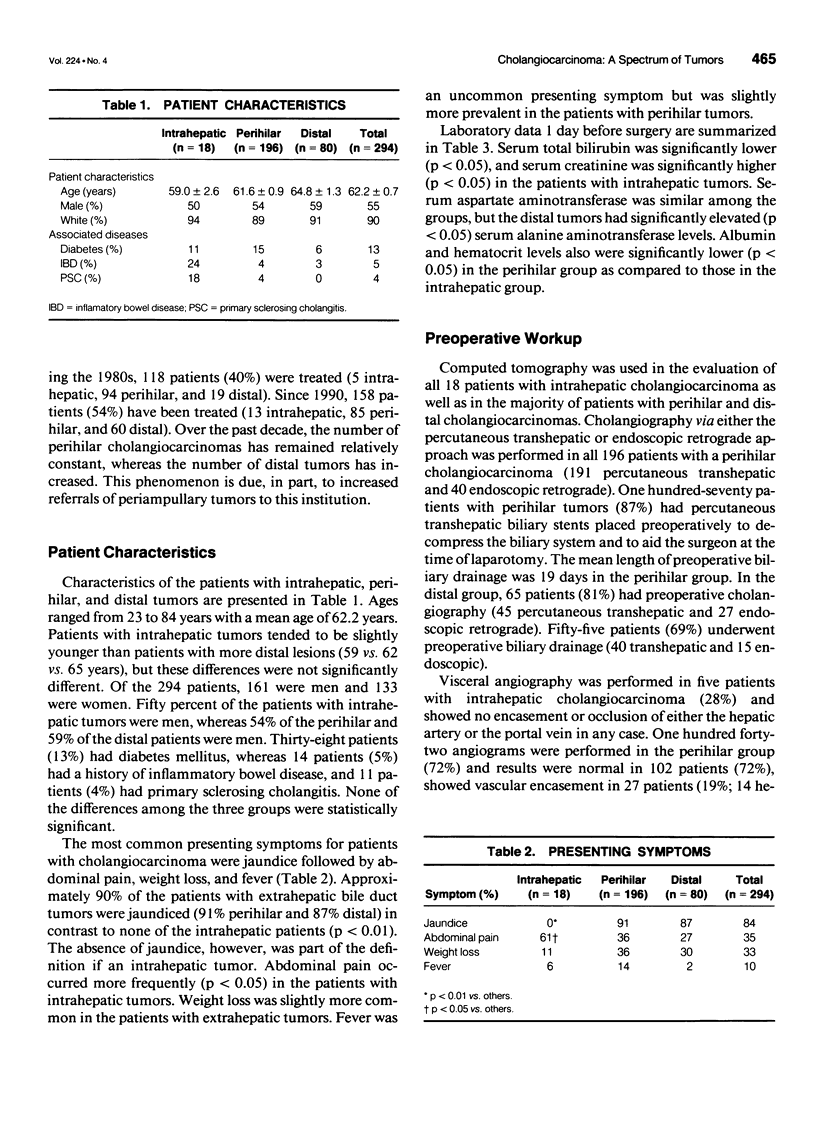
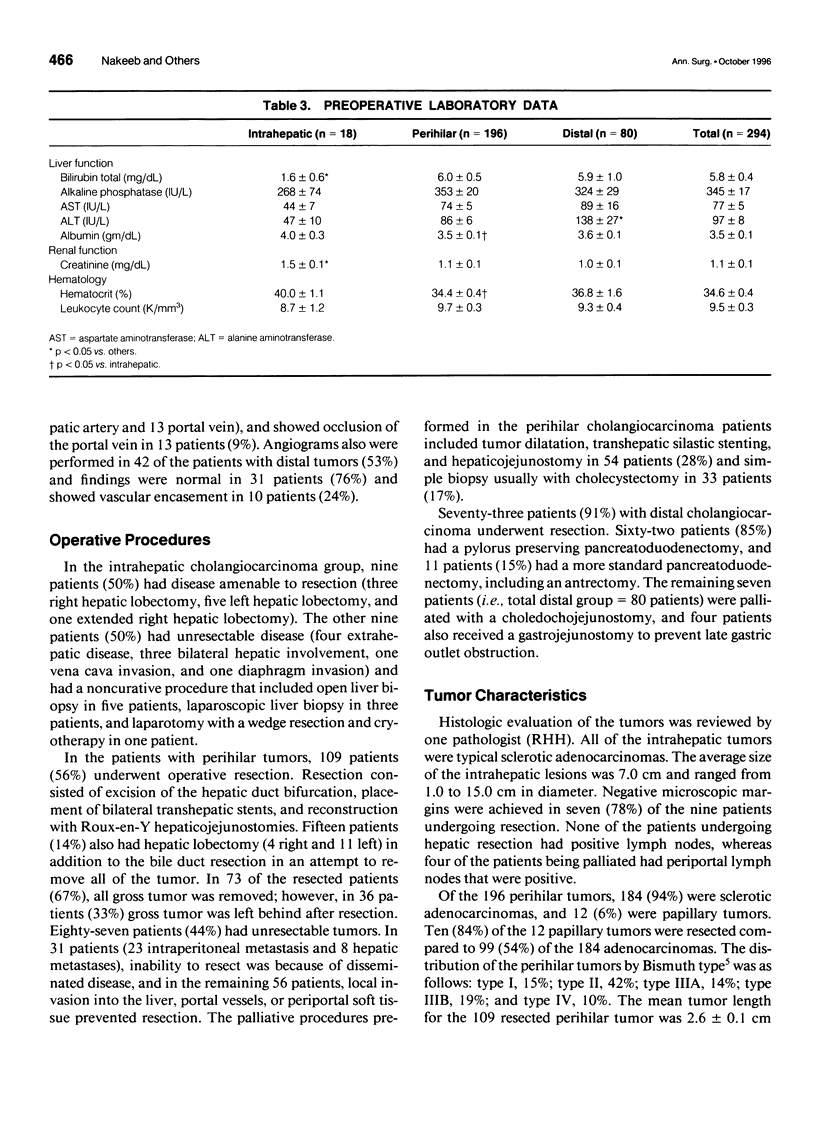
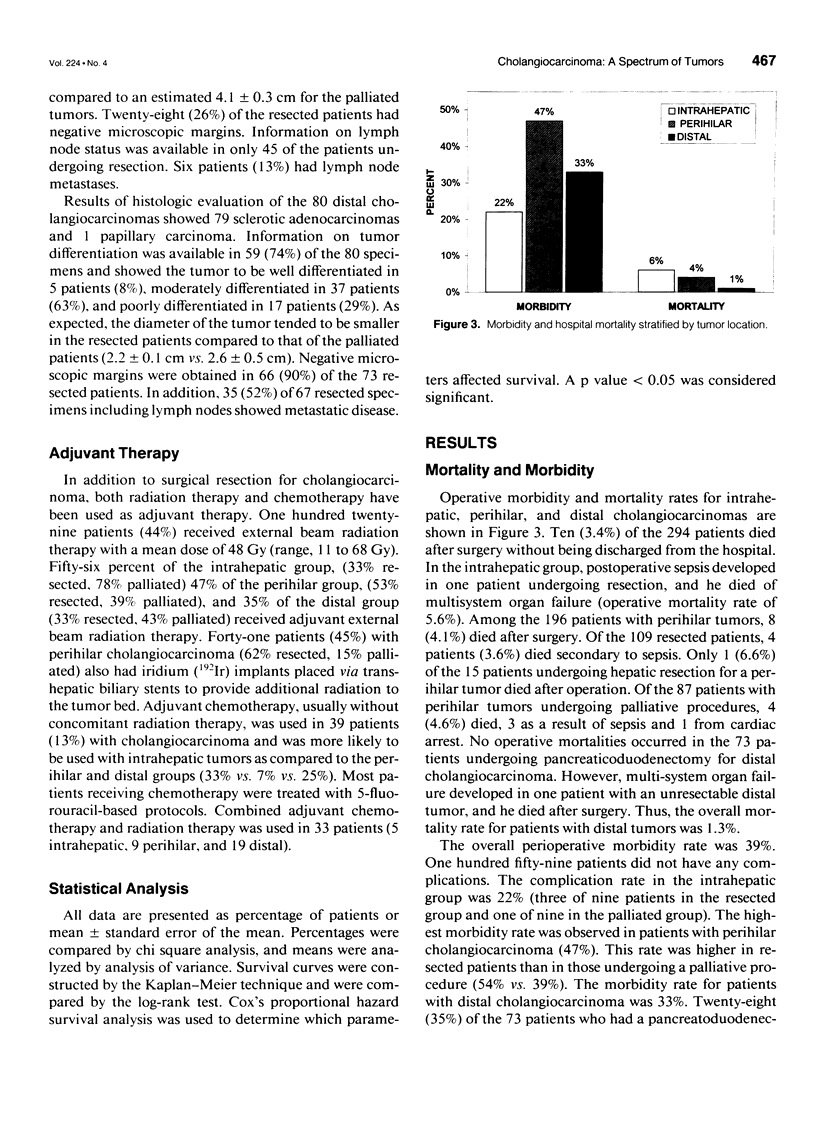
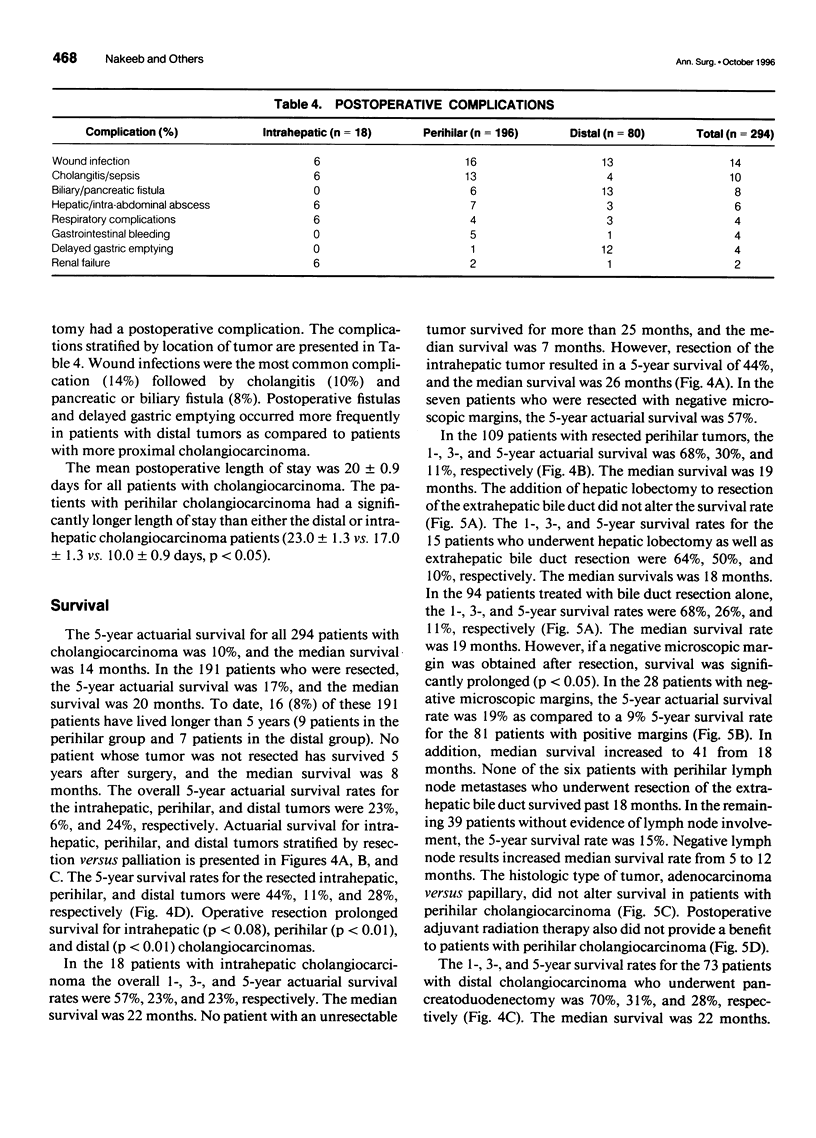
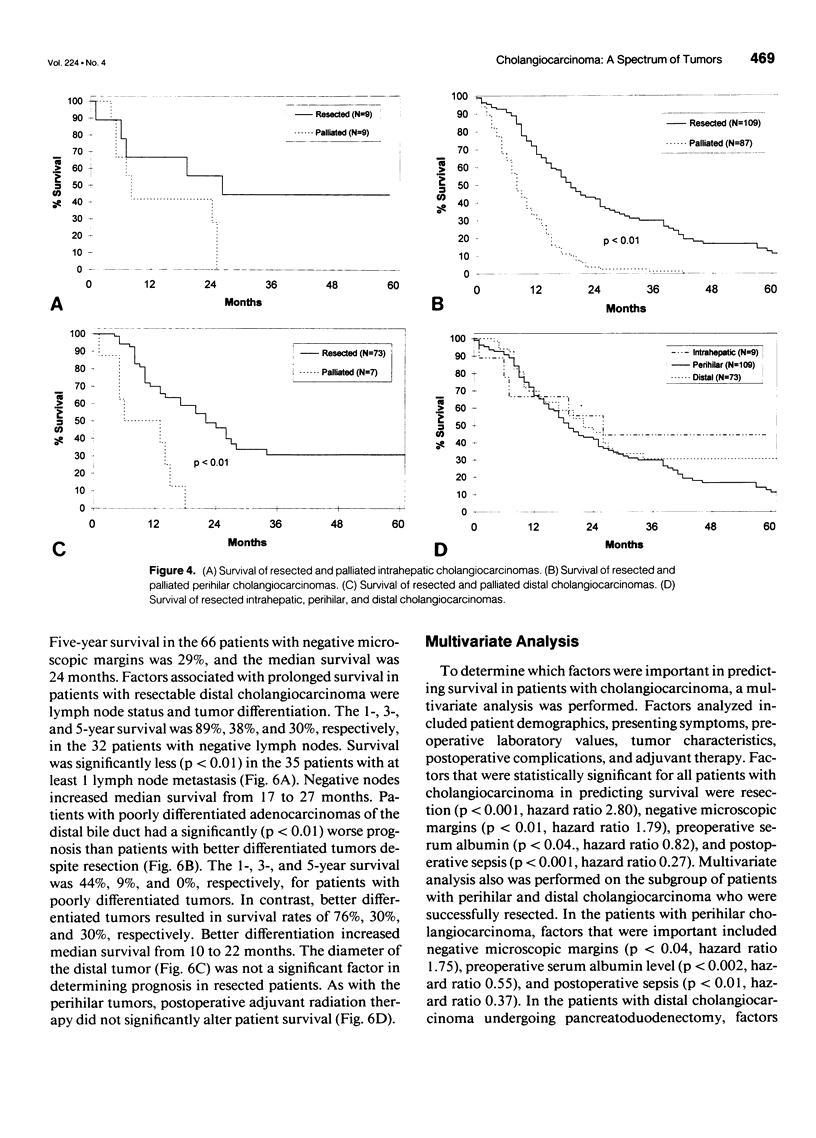
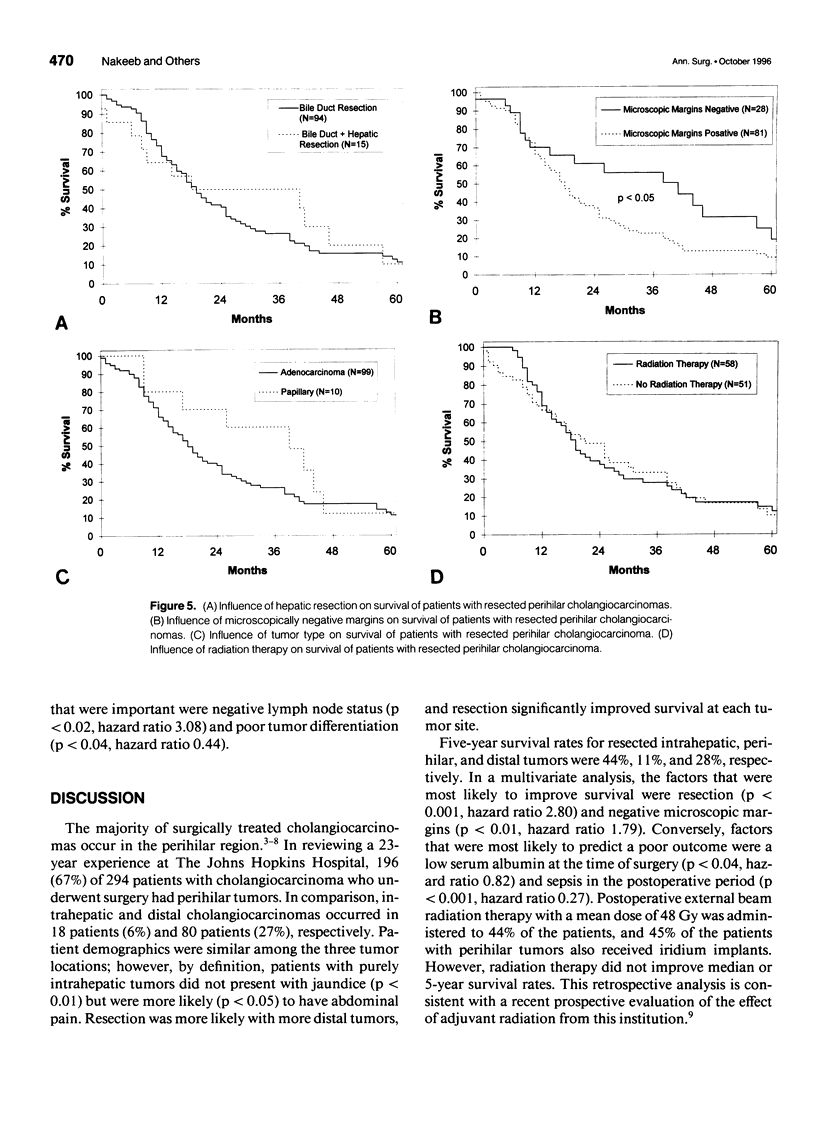
OBJECTIVE: The objective of this article is to introduce a simple method for classifying cholangiocarcinomas and to apply this system to analyze a large number of patients from a single institution. SUMMARY BACKGROUND DATA: For the past 2 decades, most western reports on cholangiocarcinoma have separated intrahepatic from extrahepatic tumors and have subclassified this latter group into proximal, middle, and distal subgroups. However, "middle" lesions are uncommon and are managed most often either with hilar resection or with pancreatoduodenectomy. The spectrum of cholangiocarcinoma, therefore, is best classified into three broad groups: 1) intrahepatic, 2) perihilar, and 3) distal tumors. These categories correlate with anatomic distribution and imply preferred treatment. METHODS: The records of all patients with histologically confirmed cholangiocarcinoma who underwent surgical exploration at The Johns Hopkins Hospital over a 23-year period were reviewed. RESULTS: Of 294 patients with cholangiocarcinoma, 18 (6%) had intrahepatic, 196 (67%) had perihilar, and 80 (27%) had distal tumors. Age, gender, race, and associated diseases were similar among the three groups. Patients with intrahepatic tumors, by definition, were less likely (p < 0.01) to be jaundiced and more likely (p < 0.05) to present with abdominal pain. The resectability rate increased with a more distal location (50% vs. 56% vs. 91%), and resection improved survival at each site. Five-year survival rates for resected intrahepatic, perihilar, and distal tumors were 44%, 11%, and 28%, and median survival rates were 26, 19, and 22 months, respectively. Postoperative radiation therapy did not improve survival. In a multivariate analysis resection (p < 0.001. hazard ratio 2.80), negative microscopic margins (p < 0.01, hazard ratio 1.79), preoperative serum albumin (p < 0.04, hazard ratio 0.82), and postoperative sepsis (p < 0.001, hard ratio 0.27) were the best predictors of outcome. CONCLUSIONS: Cholangiocarcinoma is best classified into three broad categories. Resection remains the primary treatment, whereas postoperative adjuvant radiation has no influence on survival. Therefore, new agents or strategies to deliver adjuvant therapy are needed to improve survival.
Full text
PDF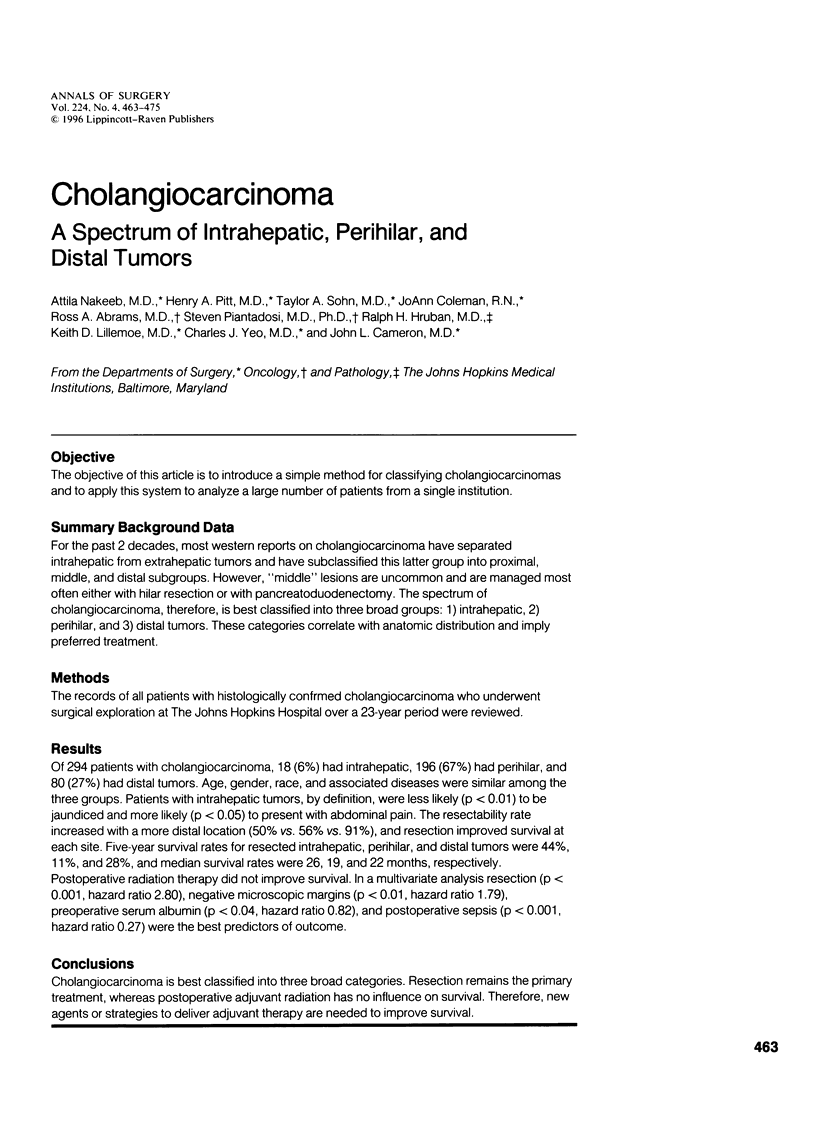
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baer H. U., Stain S. C., Dennison A. R., Eggers B., Blumgart L. H. Improvements in survival by aggressive resections of hilar cholangiocarcinoma. Ann Surg. 1993 Jan;217(1):20–27. doi: 10.1097/00000658-199301000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bismuth H., Corlette M. B. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975 Feb;140(2):170–178. [PubMed] [Google Scholar]
- Boerma E. J. Research into the results of resection of hilar bile duct cancer. Surgery. 1990 Sep;108(3):572–580. [PubMed] [Google Scholar]
- Cameron J. L., Pitt H. A., Zinner M. J., Kaufman S. L., Coleman J. Management of proximal cholangiocarcinomas by surgical resection and radiotherapy. Am J Surg. 1990 Jan;159(1):91–98. doi: 10.1016/s0002-9610(05)80612-9. [DOI] [PubMed] [Google Scholar]
- Chen M. F., Jan Y. Y., Wang C. S., Jeng L. B., Hwang T. L. Clinical experience in 20 hepatic resections for peripheral cholangiocarcinoma. Cancer. 1989 Dec 1;64(11):2226–2232. doi: 10.1002/1097-0142(19891201)64:11<2226::aid-cncr2820641107>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Childs T., Hart M. Aggressive surgical therapy for Klatskin tumors. Am J Surg. 1993 May;165(5):554–557. doi: 10.1016/s0002-9610(05)80433-7. [DOI] [PubMed] [Google Scholar]
- Chou F. F., Sheen-Chen S. M., Chen C. L., Chen Y. S., Chen M. C. Prognostic factors of resectable intrahepatic cholangiocarcinoma. J Surg Oncol. 1995 May;59(1):40–44. doi: 10.1002/jso.2930590111. [DOI] [PubMed] [Google Scholar]
- Fortner J. G., Vitelli C. E., Maclean B. J. Proximal extrahepatic bile duct tumors. Analysis of a series of 52 consecutive patients treated over a period of 13 years. Arch Surg. 1989 Nov;124(11):1275–1279. doi: 10.1001/archsurg.1989.01410110029005. [DOI] [PubMed] [Google Scholar]
- Guthrie C. M., Haddock G., De Beaux A. C., Garden O. J., Carter D. C. Changing trends in the management of extrahepatic cholangiocarcinoma. Br J Surg. 1993 Nov;80(11):1434–1439. doi: 10.1002/bjs.1800801128. [DOI] [PubMed] [Google Scholar]
- Koyama K., Tanaka J., Sato Y., Seki H., Kato Y., Umezawa A. Experience in twenty patients with carcinoma of hilar bile duct treated by resection, targeting chemotherapy and intracavitary irradiation. Surg Gynecol Obstet. 1993 Mar;176(3):239–245. [PubMed] [Google Scholar]
- Kraybill W. G., Lee H., Picus J., Ramachandran G., Lopez M. J., Kucik N., Myerson R. J. Multidisciplinary treatment of biliary tract cancers. J Surg Oncol. 1994 Apr;55(4):239–245. doi: 10.1002/jso.2930550408. [DOI] [PubMed] [Google Scholar]
- Langer J. C., Langer B., Taylor B. R., Zeldin R., Cummings B. Carcinoma of the extrahepatic bile ducts: results of an aggressive surgical approach. Surgery. 1985 Oct;98(4):752–759. [PubMed] [Google Scholar]
- Minsky B. D., Kemeny N., Armstrong J. G., Reichman B., Botet J. Extrahepatic biliary system cancer: an update of a combined modality approach. Am J Clin Oncol. 1991 Oct;14(5):433–437. doi: 10.1097/00000421-199110000-00014. [DOI] [PubMed] [Google Scholar]
- Nagorney D. M., Donohue J. H., Farnell M. B., Schleck C. D., Ilstrup D. M. Outcomes after curative resections of cholangiocarcinoma. Arch Surg. 1993 Aug;128(8):871–879. doi: 10.1001/archsurg.1993.01420200045008. [DOI] [PubMed] [Google Scholar]
- Nimura Y., Hayakawa N., Kamiya J., Maeda S., Kondo S., Yasui A., Shionoya S. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg. 1991 Jun;78(6):727–731. doi: 10.1002/bjs.1800780629. [DOI] [PubMed] [Google Scholar]
- Pichlmayr R., Lamesch P., Weimann A., Tusch G., Ringe B. Surgical treatment of cholangiocellular carcinoma. World J Surg. 1995 Jan-Feb;19(1):83–88. doi: 10.1007/BF00316984. [DOI] [PubMed] [Google Scholar]
- Pitt H. A., Dooley W. C., Yeo C. J., Cameron J. L. Malignancies of the biliary tree. Curr Probl Surg. 1995 Jan;32(1):1–90. doi: 10.1016/s0011-3840(05)80011-5. [DOI] [PubMed] [Google Scholar]
- Pitt H. A., Nakeeb A., Abrams R. A., Coleman J., Piantadosi S., Yeo C. J., Lillemore K. D., Cameron J. L. Perihilar cholangiocarcinoma. Postoperative radiotherapy does not improve survival. Ann Surg. 1995 Jun;221(6):788–798. doi: 10.1097/00000658-199506000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reding R., Buard J. L., Lebeau G., Launois B. Surgical management of 552 carcinomas of the extrahepatic bile ducts (gallbladder and periampullary tumors excluded). Results of the French Surgical Association Survey. Ann Surg. 1991 Mar;213(3):236–241. doi: 10.1097/00000658-199103000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson J. M., Lawrence T. S., Dworzanin L. M., Andrews J. C., Walker S., Kessler M. L., DuRoss D. J., Ensminger W. D. Treatment of primary hepatobiliary cancers with conformal radiation therapy and regional chemotherapy. J Clin Oncol. 1993 Jul;11(7):1286–1293. doi: 10.1200/JCO.1993.11.7.1286. [DOI] [PubMed] [Google Scholar]
- Schlinkert R. T., Nagorney D. M., Van Heerden J. A., Adson M. A. Intrahepatic cholangiocarcinoma: clinical aspects, pathology and treatment. HPB Surg. 1992;5(2):95–102. doi: 10.1155/1992/93976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenthaler R., Phillips T. L., Castro J., Efird J. T., Better A., Way L. W. Carcinoma of the extrahepatic bile ducts. The University of California at San Francisco experience. Ann Surg. 1994 Mar;219(3):267–274. doi: 10.1097/00000658-199403000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiura Y., Nakamura S., Iida S., Hosoda Y., Ikeuchi S., Mori S., Sugioka A., Tsuzuki T. Extensive resection of the bile ducts combined with liver resection for cancer of the main hepatic duct junction: a cooperative study of the Keio Bile Duct Cancer Study Group. Surgery. 1994 Apr;115(4):445–451. [PubMed] [Google Scholar]
- Tashiro S., Tsuji T., Kanemitsu K., Kamimoto Y., Hiraoka T., Miyauchi Y. Prolongation of survival for carcinoma at the hepatic duct confluence. Surgery. 1993 Mar;113(3):270–278. [PubMed] [Google Scholar]
- Tompkins R. K., Saunders K., Roslyn J. J., Longmire W. P., Jr Changing patterns in diagnosis and management of bile duct cancer. Ann Surg. 1990 May;211(5):614–621. [PMC free article] [PubMed] [Google Scholar]
- Tompkins R. K., Thomas D., Wile A., Longmire W. P., Jr Prognostic factors in bile duct carcinoma: analysis of 96 cases. Ann Surg. 1981 Oct;194(4):447–457. doi: 10.1097/00000658-198110000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuzuki T., Ueda M., Kuramochi S., Iida S., Takahashi S., Iri H. Carcinoma of the main hepatic duct junction: indications, operative morbidity and mortality, and long-term survival. Surgery. 1990 Sep;108(3):495–501. [PubMed] [Google Scholar]
- Washburn W. K., Lewis W. D., Jenkins R. L. Aggressive surgical resection for cholangiocarcinoma. Arch Surg. 1995 Mar;130(3):270–276. doi: 10.1001/archsurg.1995.01430030040006. [DOI] [PubMed] [Google Scholar]
- Yamamoto J., Kosuge T., Takayama T., Shimada K., Makuuchi M., Yoshida J., Sakamoto M., Hirohashi S., Yamasaki S., Hasegawa H. Surgical treatment of intrahepatic cholangiocarcinoma: four patients surviving more than five years. Surgery. 1992 Jun;111(6):617–622. [PubMed] [Google Scholar]


