Abstract
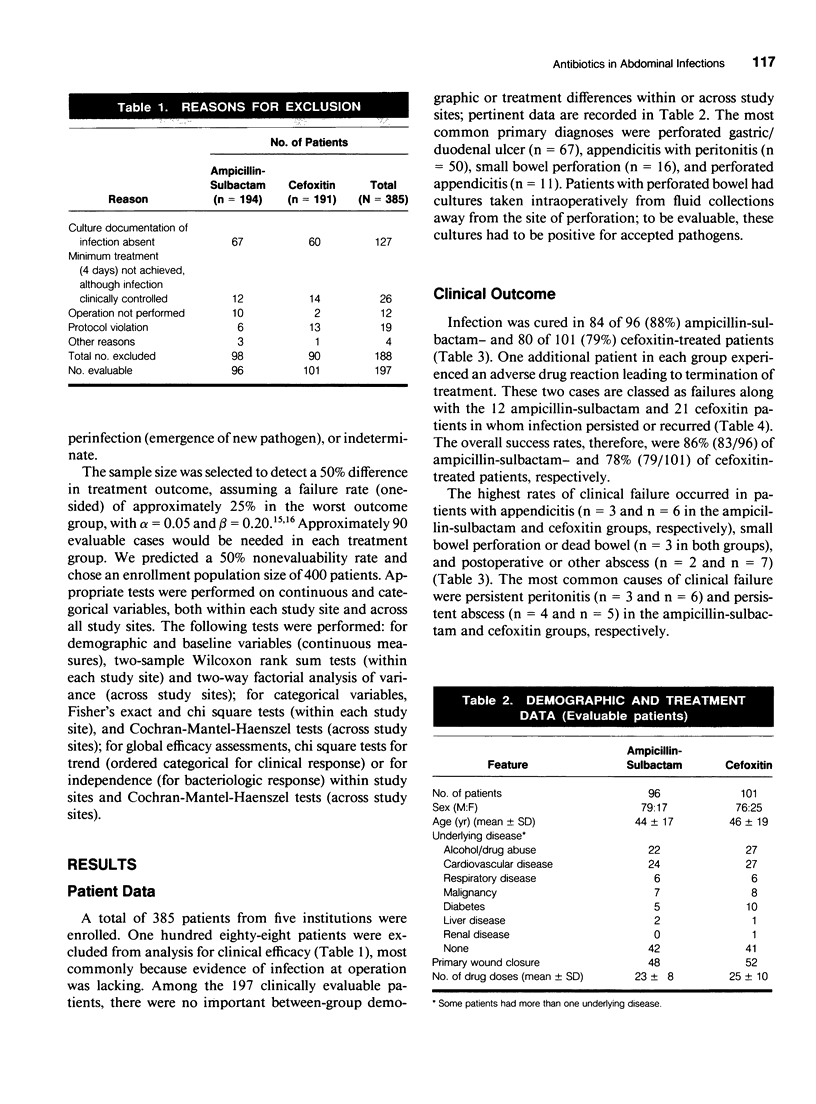
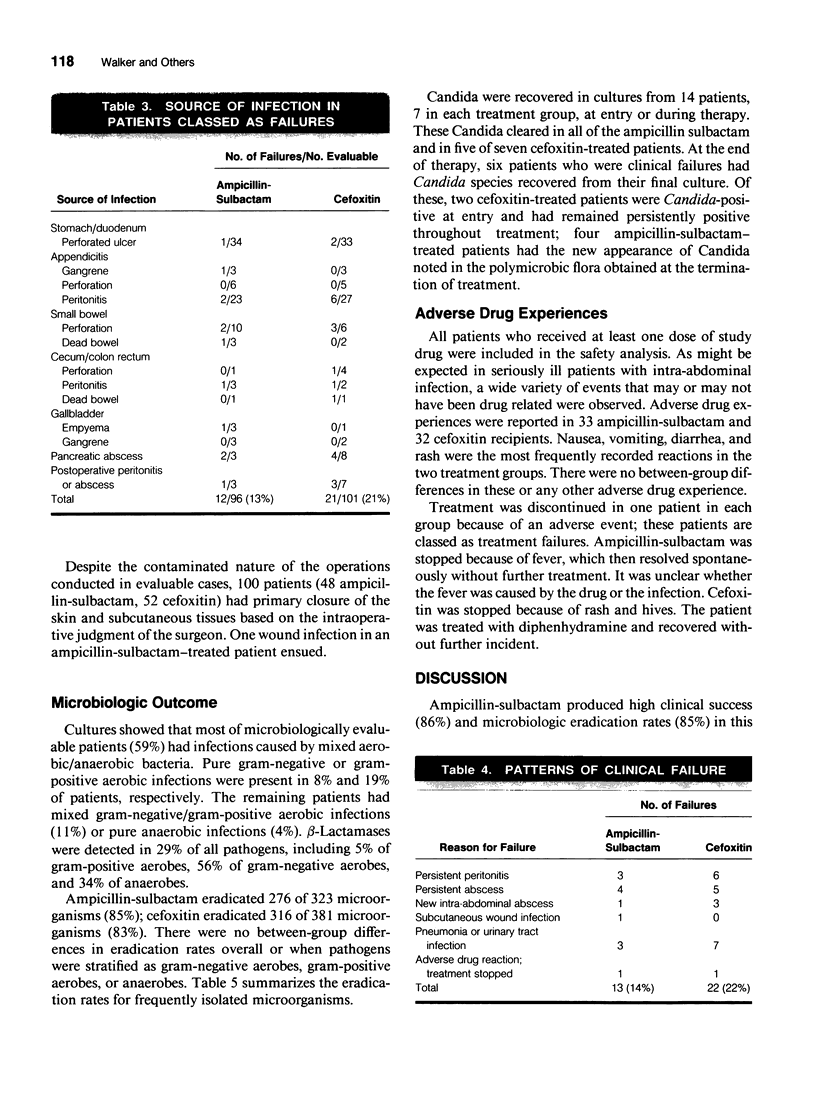
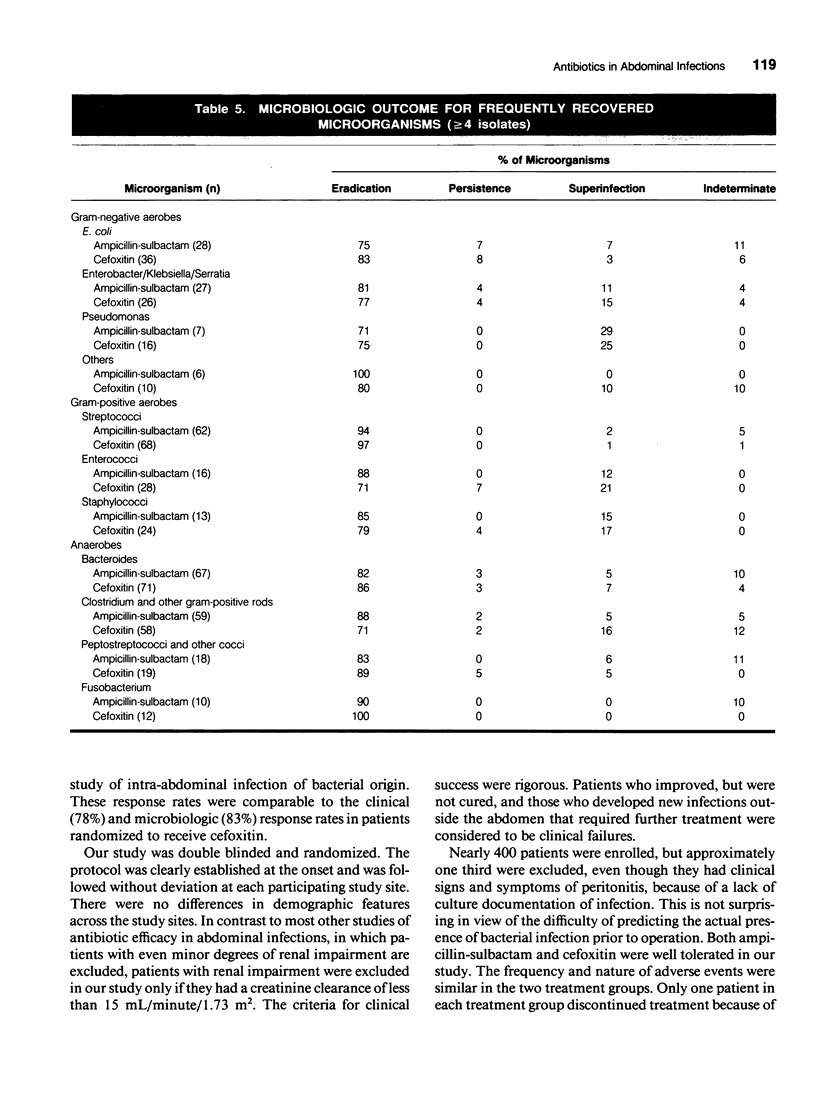
A double-blind trial was conducted in 385 patients with suspected bacterial intra-abdominal infections to compare the efficacy and safety of ampicillin-sulbactam with cefoxitin. Patients were randomized to receive either 3 g ampicillin-sulbactam (2 g ampicillin-1 g sulbactam), or 2 g cefoxitin, every 6 hours. To be evaluable, patients had to demonstrate positive culture evidence of peritoneal infection at the time of operation. A total of 197 patients were evaluable for clinical efficacy. The two treatment groups were comparable in demographic features and in the presence of risk factors for infection. Clinical success (absence of infection and of adverse drug reaction) was observed in 86% of patients in the ampicillin-sulbactam group and 78% in the cefoxitin group. Eradication of infection occurred in 88% of the ampicillin-sulbactam group and 79% of the cefoxitin group. There were no differences in the nature or frequency of side effects observed in the two groups. Ampicillin-sulbactam demonstrated no difference in safety or efficacy when compared with cefoxitin in the treatment of serious intra-abdominal infections of bacterial origin.
Full text
PDF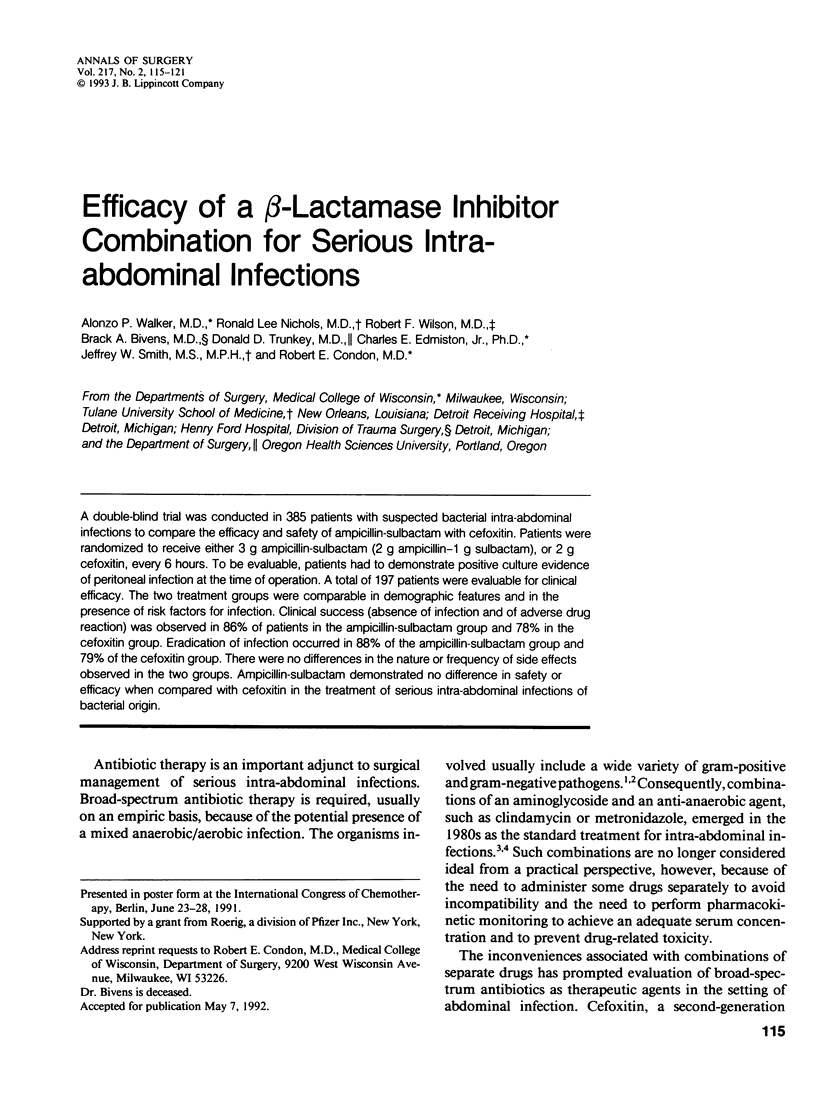
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aronoff S. C., Olson M. M., Gauderer M. W., Jacobs M. R., Blumer J. L., Izant R. J., Jr Pseudomonas aeruginosa as a primary pathogen in children with bacterial peritonitis. J Pediatr Surg. 1987 Sep;22(9):861–864. doi: 10.1016/s0022-3468(87)80656-5. [DOI] [PubMed] [Google Scholar]
- Bohnen J. M., Solomkin J. S., Dellinger E. P., Bjornson H. S., Page C. P. Guidelines for clinical care: anti-infective agents for intra-abdominal infection. A Surgical Infection Society policy statement. Arch Surg. 1992 Jan;127(1):83–89. doi: 10.1001/archsurg.1992.01420010097015. [DOI] [PubMed] [Google Scholar]
- Bohnen J., Boulanger M., Meakins J. L., McLean A. P. Prognosis in generalized peritonitis. Relation to cause and risk factors. Arch Surg. 1983 Mar;118(3):285–290. doi: 10.1001/archsurg.1983.01390030017003. [DOI] [PubMed] [Google Scholar]
- Dellinger E. P. Use of scoring systems to assess patients with surgical sepsis. Surg Clin North Am. 1988 Feb;68(1):123–145. doi: 10.1016/s0039-6109(16)44436-1. [DOI] [PubMed] [Google Scholar]
- Drusano G. L., Warren J. W., Saah A. J., Caplan E. S., Tenney J. H., Hansen S., Granados J., Standiford H. C., Miller E. H., Jr A prospective randomized controlled trial of cefoxitin versus clindamycin-aminoglycoside in mixed anaerobic-aerobic infections. Surg Gynecol Obstet. 1982 May;154(5):715–720. [PubMed] [Google Scholar]
- Fink M. P. Antibiotic therapy of intra-abdominal sepsis in the elderly: experience with ticarcillin and clavulanic acid. Surg Gynecol Obstet. 1991;172 (Suppl):36–41. [PubMed] [Google Scholar]
- Fry D. E., Garrison R. N., Heitsch R. C., Calhoun K., Polk H. C., Jr Determinants of death in patients with intraabdominal abscess. Surgery. 1980 Oct;88(4):517–523. [PubMed] [Google Scholar]
- Hau T., Ahrenholz D. H., Simmons R. L. Secondary bacterial peritonitis: the biologic basis of treatment. Curr Probl Surg. 1979 Oct;16(10):1–65. doi: 10.1016/s0011-3840(79)80011-8. [DOI] [PubMed] [Google Scholar]
- Ho J. L., Barza M. Role of aminoglycoside antibiotics in the treatment of intra-abdominal infection. Antimicrob Agents Chemother. 1987 Apr;31(4):485–491. doi: 10.1128/aac.31.4.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inthorn D., Mühlbayer D., Hartl W. H. Ticarcillin/clavulanate in the treatment of severe peritonitis. J Antimicrob Chemother. 1989 Nov;24 (Suppl B):141–146. doi: 10.1093/jac/24.suppl_b.141. [DOI] [PubMed] [Google Scholar]
- Lee C. Y., Lin T. Y., Chu M. L., Lee M. J., Hsu C. Y., Huang L. M., Chen C. M. Intravenous sulbactam/ampicillin in the treatment of pediatric infections. Diagn Microbiol Infect Dis. 1989 Jul-Aug;12(4 Suppl):179S–183S. doi: 10.1016/0732-8893(89)90133-8. [DOI] [PubMed] [Google Scholar]
- Meakins J. L., Solomkin J. S., Allo M. D., Dellinger E. P., Howard R. J., Simmons R. L. A proposed classification of intra-abdominal infections. Stratification of etiology and risk for future therapeutic trials. Arch Surg. 1984 Dec;119(12):1372–1378. doi: 10.1001/archsurg.1984.01390240010002. [DOI] [PubMed] [Google Scholar]
- Mehtar S., Croft R. J., Hilas A. A non-comparative study of parenteral ampicillin and sulbactam in intra-thoracic and intra-abdominal infections. J Antimicrob Chemother. 1986 Mar;17(3):389–396. doi: 10.1093/jac/17.3.389. [DOI] [PubMed] [Google Scholar]
- Nyström P. O., Bax R., Dellinger E. P., Dominioni L., Knaus W. A., Meakins J. L., Ohmann C., Solomkin J. S., Wacha H., Wittmann D. H. Proposed definitions for diagnosis, severity scoring, stratification, and outcome for trials on intraabdominal infection. Joint Working Party of SIS North America and Europe. World J Surg. 1990 Mar-Apr;14(2):148–158. doi: 10.1007/BF01664867. [DOI] [PubMed] [Google Scholar]
- Pine R. W., Wertz M. J., Lennard E. S., Dellinger E. P., Carrico C. J., Minshew B. H. Determinants of organ malfunction or death in patients with intra-abdominal sepsis. A discriminant analysis. Arch Surg. 1983 Feb;118(2):242–249. doi: 10.1001/archsurg.1983.01390020084014. [DOI] [PubMed] [Google Scholar]
- Retsema J. A., English A. R., Girard A., Lynch J. E., Anderson M., Brennan L., Cimochowski C., Faiella J., Norcia W., Sawyer P. Sulbactam/ampicillin: in vitro spectrum, potency, and activity in models of acute infection. Rev Infect Dis. 1986 Nov-Dec;8 (Suppl 5):S528–S534. doi: 10.1093/clinids/8.supplement_5.s528. [DOI] [PubMed] [Google Scholar]
- Sirinek K. R., Levine B. A. A randomized trial of ticarcillin and clavulanate versus gentamicin and clindamycin in patients with complicated appendicitis. Surg Gynecol Obstet. 1991;172 (Suppl):30–35. [PubMed] [Google Scholar]
- Solomkin J. S., Dellinger E. P., Christou N. V., Busuttil R. W. Results of a multicenter trial comparing imipenem/cilastatin to tobramycin/clindamycin for intra-abdominal infections. Ann Surg. 1990 Nov;212(5):581–591. doi: 10.1097/00000658-199011000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomkin J. S., Dellinger E. P., Christou N. V., Mason A. D., Jr Design and conduct of antibiotic trials. A report of the Scientific Studies Committee of the Surgical Infection Society. Arch Surg. 1987 Feb;122(2):158–164. doi: 10.1001/archsurg.1987.01400140040004. [DOI] [PubMed] [Google Scholar]
- Solomkin J. S., Meakins J. L., Jr, Allo M. D., Dellinger E. P., Simmons R. L. Antibiotic trials in intra-abdominal infections. A critical evaluation of study design and outcome reporting. Ann Surg. 1984 Jul;200(1):29–39. doi: 10.1097/00000658-198407000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tally F. P., McGowan K., Kellum J. M., Gorbach S. L., O'Donnell T. F. A randomized comparison of cefoxitin with or without amikacin and clindamycin plus amikacin in surgical sepsis. Ann Surg. 1981 Mar;193(3):318–323. doi: 10.1097/00000658-198103000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wexler H. M., Harris B., Carter W. T., Finegold S. M. In vitro efficacy of sulbactam combined with ampicillin against anaerobic bacteria. Antimicrob Agents Chemother. 1985 May;27(5):876–878. doi: 10.1128/aac.27.5.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yellin A. E., Heseltine P. N., Berne T. V., Appleman M. D., Gill M. A., Riggio C. E., Chenella F. C. The role of Pseudomonas species in patients treated with ampicillin and Sulbactam for gangrenous and perforated appendicitis. Surg Gynecol Obstet. 1985 Oct;161(4):303–307. [PubMed] [Google Scholar]
- Young M. J., Bresnitz E. A., Strom B. L. Sample size nomograms for interpreting negative clinical studies. Ann Intern Med. 1983 Aug;99(2):248–251. doi: 10.7326/0003-4819-99-2-248. [DOI] [PubMed] [Google Scholar]


