Abstract
Background
Coiled microcatheters have substantially contributed to the success of retrograde chronic total occlusion percutaneous coronary intervention (CTO-PCI), thanks to their ability to cross challenging anatomies with only a marginal compromise in terms of support, but the increasing complexity is exposing new limitations associated with potential complications.
Case Summary
A patient undergoing CTO-PCI developed a rare complication with donor vessel occlusion due to a microcatheter coiling around a previously implanted stent. Despite the severity of the situation, artery patency was successfully restored. The patient experienced arrhythmic events in the intensive care unit, requiring ongoing hemodynamic support to stabilize the condition.
Discussion
This scenario raises a crucial issue regarding complications related to coiled microcatheters, highlights the lifesaving value of CTO techniques in non-CTO settings, and remarks on the importance of percutaneous hemodynamic support in life-threatening complications.
Take-Home Messages
Coiled microcatheter entrapment can lead to severe complications during CTO-PCI, including stent crushing and donor vessel occlusion. Timely intervention with CTO techniques and hemodynamic support is crucial in managing life-threatening complications and stabilizing the patient.
Key words: cardiogenic shock, coronary chronic total occlusion percutaneous intervention, hemodynamic support, microcatheter fracture, PCI complication
Graphical Abstract

Case Presentation
A 77-year-old man with a history of previous left anterior descending artery (LAD) coronary stent implantation (2008), with a recent LAD stent-in-stent implantation (drug-eluting stent 3 × 34 mm) (Figures 1A to 1C), and with an unsuccessful attempt at chronic total occlusion percutaneous coronary intervention (CTO-PCI) of the distal right coronary artery (RCA) (Figures 1D to 1F) was referred to our institution 2 months later for RCA CTO-PCI because of persistence of angina. The RCA CTO involved the distality of the vessel, the crux, and the proximal tract of the posterolateral (PL) and posterior descending (PD) branches (Video 1 S1). The first attempt resulted in subintimal tracking and false lumen stent implantation from the crux to the PL branch, which also was complicated by a dissection of the right aortic sinus, necessitating an emergent ostial protruding stent implantation (Figure 1F, Video 1 S2 and 1 S3). As a result, PD remained occluded and excluded from the true lumen by the subintimal stent, the PL branch resulted in no flow (TIMI [flow grading system] <1), and the RCA engagement was compromised by the large protrusion (7 mm) of the ostial stent, as confirmed by a computed tomography scan (Figure 2A). This scenario, confirmed by our dual injection angiography, made the retrograde approach the only option for performing CTO-PCI (Figure 2B, Video 1 S4). With a protection wire distal in the LAD, the retrograde approach was performed by septal surfing. A distal septal branch was selected to avoid those originating from stent struts; it was engaged and surfed with a SION standard wire supported by a 150-cm Turnpike-LP microcatheter overcoming 2 sharp bends (Figures 2C and 2D, Video 1 S5). Having reached the PD branch, a Gladius wire successfully crossed the proximal PD occlusion and entered the true lumen at the level of the crux, located outside the stent. The microcatheter was then advanced and a Gaia Next 3 wire was used to re-enter the stent (Figure 3A, Video 1 S6). Then, having the microcatheter advanced in the proximal RCA, a U-shaped Gladius was advanced until the aorta to avoid the passage in the struts of the ostial stent (Video 1 S7). The RG3 externalization wire was snared in the brachiocephalic trunk for externalization (Figure 3B, Video 1 S8). The true lumen was recovered, and an atraumatic cannulation of the RCA was possible (Video 1 S9). After predilatation, an intravascular ultrasound (IVUS) run showed the true lumen wire position and the crush of the previously implanted subintimal stents due to dilatation, and a 2.75 × 26 mm stent was implanted in an IVUS-guided fashion. A dual-lumen microcatheter was used to wire the PL with an UltimateBros3, followed by a kissing-balloon and proximal optimization technique. A drug-coated balloon was then inflated for the mid-distal PD and PL disease. The angiographic and IVUS control showed a good result (Figure 3C, Video 1 S10). At this time, we encountered significant resistance when attempting to readvance the microcatheter for the externalized wire removal, and then we realized that the microcatheter was stuck, with RG3 jailed inside it. After considerable effort, we could advance the microcatheter until the mid-tract of PD and retract the externalized wire, even though the friction was tremendous. We attempted to insert a more supportive wire in the microcatheter, with the hope that it would support the extraction, but it could not cross the distal part of it. Then we tried to retract the Turnpike with constant and vigorous force, as we had done with the RG3, but it was elongating without any movement. At this point, the patient became symptomatic, experiencing chest pain and hemodynamic instability. We trapped the microcatheter with a 2.5 × 20 mm balloon to change the retraction force point and prevent further elongation. Initially, this maneuver seemed effective, but unexpectedly, we lost tension, and the catheter suddenly jumped out of the coronary. While part of the microcatheter was extracted, another section remained in the coronary. The angiographic control revealed a catastrophic situation, with a fractured microcatheter body in the septal branch and the previously implanted stent in the LAD crushed, fractured, and collapsed (Video 1 S11). The artery was dissected and occluded, and the patient's condition suddenly worsened; in a few minutes, cardiogenic shock occurred. After unsuccessful attempts to cross the broken stent with a SION standard and SION Black wire (Figure 4A, Video 1 S12), we managed to advance a Gladius EX, which reached the distal true lumen. However, using the mother-child technique, we could not cross the scrunched part of the stent, even with a low-profile microcatheter or balloon. Realizing that we were in failure mode, we decided to change our strategy. We punctured the scrunched part of the stent with a Gaia Next 3, which crossed in subintimal space (Figure 4B, Video 1 S13). This time, the Caravel microcatheter successfully crossed, and then a STAR technique (subintimal tracking and re-entry—a CTO-PCI technique) was performed with a Fielder XT-A wire to re-enter the true lumen (Figure 4C, Video 1 S14). After several attempts and 3 grenadoplasties, we were able to successfully cross with balloons in an inchworming fashion (Figures 5A and 5B, Video 1 S15) and proceeded with dilatation. At this point, the patient's hemodynamics recovered stability, but the angiography revealed a high thrombotic burden involving the LAD and the diagonal (Figure 5C) necessitating intracoronary administration of glycoprotein IIb-IIIa inhibitors. Two stents were then implanted: one distally, where the previous stent had been crushed, and another proximally, where the stent had fractured. The first diagonal branch and central sections were treated with drug-coated balloons with a good result (Figure 6A, Video 1 S16). The IVUS examination was performed to optimize the result (Figure 6B). A good angiographic result was confirmed again in the RCA (Figure 6C). Given the stable hemodynamics and the very high hemorrhagic risk due to the use of glycoprotein IIb/IIIa inhibitors in the context of an activated clotting time of 400 seconds, we decided not to provide further hemodynamic support, despite the patient's very low ejection fraction (Video 1 S17). The patient was then admitted to the intensive care unit, where initially the hemodynamics improved and inotrope dosage de-escalation was started, but 2 days later, an episode of atrial fibrillation caused a new hemodynamic collapse. Both electrical and pharmacologic cardioversion were ineffective, resulting in cardiac arrest in a pulseless electrical activity fashion. The cardiopulmonary resuscitation was successful, but the patient remained in cardiogenic shock. The angiography demonstrated the patency of the coronary (Video 1 S18), and the decision was made to implant an Impella CP device. The ventricular support succeeded in stabilizing the patient; in fact, hemodynamics, lactate levels, and ejection fraction improved considerably (Video 1 S19). On the fifth day, the Impella support was removed. Eight days later, the patient was discharged in stable clinical condition.
Figure 1.
Past Percutaneous Coronary Interventions
(A, C) LAD PCI with 3 × 34 mm provisional stenting and POT-side-POT bifurcation optimization. (D, F) Unsuccessful right CTO-PCI complicated by right sinus dissection and false lumen stenting (D, E), necessitating an ostial protruding stent implantation (F). CTO = chronic total occlusion; LAD = left anterior descending artery; PCI = percutaneous coronary intervention; POT = proximal optimization technique.
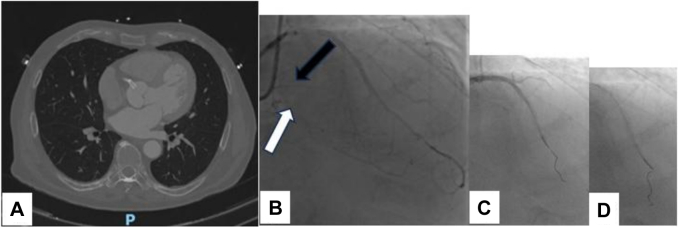
Figure 2.
Initial Phase of Our Attempt
(A) CT scan showing right sinus hematoma with an ostial protruding stent. (B, D) Good result of LAD PCI and occlusion of the DP (white arrow) and PL (black arrow) branches as demonstrated by heterocoronary collateralization (B); third tortuous septal surfing (C). CT = computed tomography; DP = descending posterior artery; LAD = left anterior descending artery; PCI = percutaneous coronary intervention; PL = posterolateral artery.
Figure 3.
Retrograde Approach
(A) Crux true lumen rescue from retrograde and in stent distal RCA re-entry. (B) RG3 wire snaring in the brachiocephalic trunk. (C) Final angiographic result in RCA. RCA = right coronary artery.
Figure 4.
Complex Scenario
(A) Uncrossable and impenetrable crushed stent, with crushed stent (white arrow); crossing attempt with a SION Black wire (red arrow) and fractured microcatheter (black arrow). (B) Subintimal position of a Gaia Next 3 wire. (C) STAR technique with a Fielder XT-A wire to re-enter. STAR = subintimal tracking and re-entry.
Figure 5.
Management
(A) Grenadoplasty, (B) balloon passage (red arrow), and (C) thrombus burden after dilatation involving the LAD and a large diagonal. LAD = left anterior descending artery.
Figure 6.
Final Result
(A) Complication management final result. (B) IVUS confirmation of the good result with the presence of a microcatheter body under the stent. (C) Final angiographic result of the RCA. IVUS = intravascular ultrasound; RCA = right coronary artery.
Discussion
The frequency and severity of complications during CTO-PCI are higher (1%-3%) compared with most PCI procedures in chronic coronary syndromes. The retrograde approach to CTO-PCI has significantly contributed to the success rates of this procedure, and it is usually performed in complex CTO lesions.1 However, compared with the antegrade approach, it has been associated with a higher complication rate in 5 of the 8 currently available CTO-PCI risk scores (PROGRESS CTO complication, PROGRESS-CTO MACE [major adverse cardiac event], PROGRESS-CTO mortality, PROGRESS-CTO perforation, and PROGRESS-CTO pericardiocentesis scores).2 The main complications described are coronary perforation, periprocedural myocardial infarction (MI), donor vessel injury, and vascular access complications.3 The rate of periprocedural MI during retrograde CTO-PCI is 0.8% to 5.7%.1 It can be caused by side branch loss that can occur with retrograde dissection re-entry. Another mechanism for periprocedural MI is prolonged obstruction of the collateral channel, leading to ischemia and infarction in the target vessel territory.
The advent of coiled microcatheters has improved the retrograde approach. However, rotational maneuvers, especially when navigating sharp bends, can lead to donor artery dissections or other coil-related complications like endothelial avulsion of small brunches.4 The interaction between a recently implanted stent and a torque microcatheter must be considered, particularly during aggressive manipulation, which probably happened in this case and caused the cascade of events that brought about complications. The microcatheter overmanipulation was needed to succeed in this complex retrograde scenario, However, this led to kinking and ultimately coiling around the stent. The stent was distorted during the retraction, and the microcatheter was entrapped and ultimately fractured. To our knowledge, this is the first report describing a rupture of a microcatheter body in a donor artery. However, applying CTO techniques and equipment in this scenario helped us overcome the problem in the donor vessel. Moreover, the rapid onset of cardiogenic shock makes our case more challenging, and the subsequent occurrence of atrial fibrillation determining a recurrence of clinical deterioration 2 days after PCI opens the issue of the best timing for hemodynamic circulatory support implantation.
Conclusions
The increase in the complexity of PCI will bring more knowledge about the potential complications derived from extreme material manipulations, specifically in our case, by the torqueable microcatheters. The case highlights how precarious the hemodynamic is in these scenarios and makes us reflect on the more appropriate timing of hemodynamic support. Finally, it showed how CTO-PCI techniques could help manage complications even in non-CTO vessels.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Take-Home Messages
-
•
Coiled microcatheter entrapment can lead to severe complications during chronic total occlusion percutaneous coronary intervention, including stent crushing and donor vessel occlusion.
-
•
Timely intervention with chronic total occlusion techniques and hemodynamic support is crucial in managing life-threatening complications and stabilizing the patient.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
Visual Summary.
| Event | |
|---|---|
| Initial presentation | 77-year-old man with angina and prior PCI history |
| First CTO-PCI attempt | False lumen stent implantation from the crux to the PL branch and dissection of the right aortic sinus |
| Retrograde approach | Retrograde CTO-PCI via a septal collateral; the wire successfully crossed the PD branch |
| Microcatheter complication | Microcatheter stuck with the wire, chest pain, and instability |
| Cardiogenic shock | Stent crush and LAD occlusion, leading to cardiogenic shock |
| Re-establish LAD patency | CTO techniques to cross and stent the LAD successfully |
| Hemodynamic support | Five days later Impella CP used for support after atrial fibrillation and cardiopulmonary resuscitation |
| Final outcome | Patient stabilized and discharged 8 days later after removal of Impella |
Equipment List.
| Imaging |
|
| CTO-PCI procedure |
|
| Impella implantation |
|
Appendix
Challenging CTO PCI with microcatheter ropture a step by step rescue
References
- 1.Allana S.S., Gondi K., Goyal A., Vallabhajosyula S. Retrograde approach to chronic total occlusion percutaneous coronary interventions- Technique and outcomes. Prog Cardiovasc Dis. 2025;88:28–38. doi: 10.1016/j.pcad.2024.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Simsek B., Rempakos A., Kostantinis S., et al. A systematic review of periprocedural risk prediction scores in chronic total occlusion percutaneous coronary intervention. Am J Cardiol. 2023;193:118–125. doi: 10.1016/j.amjcard.2023.01.044. [DOI] [PubMed] [Google Scholar]
- 3.Megaly M., Ali A., Saad M., et al. Outcomes with retrograde versus antegrade chronic total occlusion revascularization. Catheter Cardiovasc Interv. 2020;96(5):1037–1043. doi: 10.1002/ccd.28616. [DOI] [PubMed] [Google Scholar]
- 4.El Jattari H., Zivelonghi C., Scott B., Luykx M., Agostoni P. Endothelial avulsion of the septal branch during retrograde chronic total occlusion intervention. Cardiovasc Revasc Med. 2021;28:219–221. doi: 10.1016/j.carrev.2021.02.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Challenging CTO PCI with microcatheter ropture a step by step rescue