Abstract
Introduction
The study aimed to develop and validate a 3D-printed foot length scale for predicting intramedullary nail lengths in long bone fractures. The device utilizes the European (EU) foot length scale and regression models derived from retrospective patient data to estimate nail lengths for the femur, tibia, and humerus.
Methods and materials
The study involved two phases: (1) retrospective data collection and analysis to establish correlations between foot length and nail length, and (2) design, development, and validation of the 3D-printed device. Retrospective data were collected from 205 patients who underwent intramedullary nailing. The device was designed to measure foot length and estimate nail length based on the derived regression models. The device was prospectively validated in a clinical setting.
Results
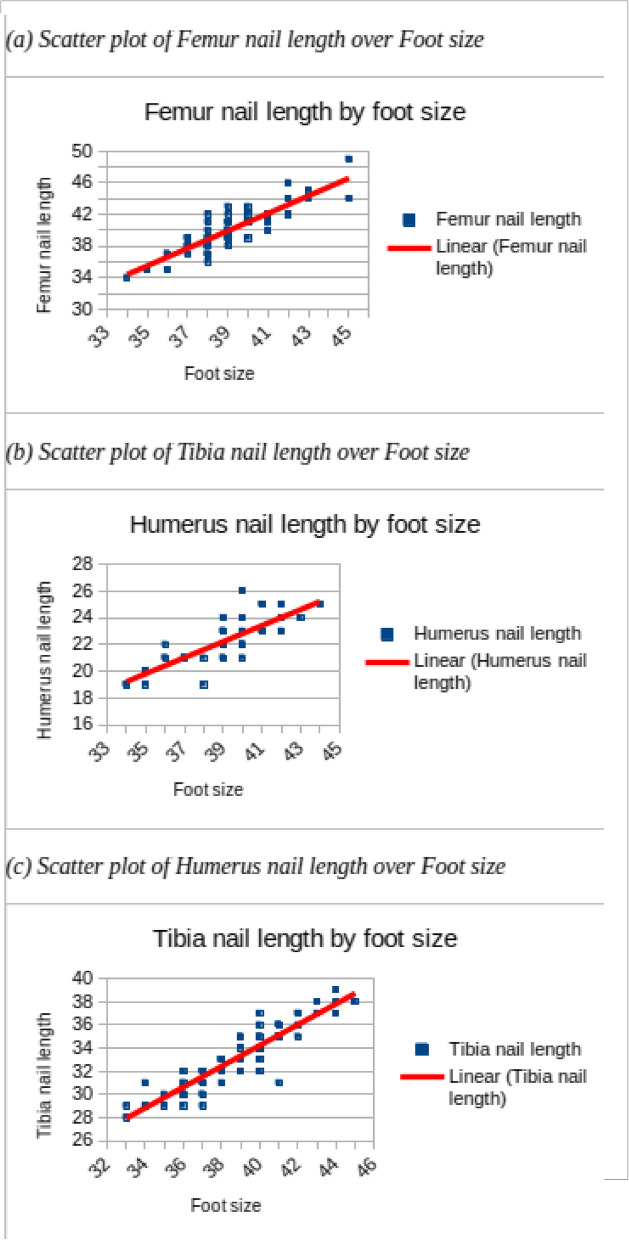
The retrospective analysis showed strong correlations between foot length and nail length for the femur (R2 = 0.98), tibia (R2 = 0.91), and humerus (R2 = 0.85). The prospective validation demonstrated high accuracy of the device, with mean absolute errors (MAE) of 0.67 cm, 0.74 cm, and 0.62 cm for femur, tibia, and humerus nail length predictions, respectively.
Conclusion
The 3D-printed foot length scale offers a practical and accurate method for predicting intramedullary nail lengths, potentially streamlining preoperative planning and improving surgical outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41205-025-00290-x.
Keywords: Foot length, Intramedullary nail, Nail length, Long bone, Fracture, 3D printing
Introduction
Intramedullary nailing is a common surgical technique for the treatment of long bone fractures, such as femur, tibia, and humerus fractures [1]. The nail length must be appropriate for the best results. Otherwise, the nails have to be taken out. Nails that are too short can cause problems such as poor alignment, rotation loss, or extraction difficulty. Nails that are too long can also cause problems such as fracture gap widening, patellar tendon irritation, or ankle joint invasion [2]. Therefore, intraoperative nail exchange is frequently required, which increases the operative time, blood loss, radiation exposure, and cost of the procedure.
The “two-guidewire technique” can help measure the nail length accurately for cannulated nails [3]. However, this technique can also lead to wrong nail size if done improperly [3]. For unreamed nails, this technique is usually not done and other methods of nail estimation are needed. Preoperative nail estimation can help avoid errors, save time, and reduce radiation during surgery. Various techniques have been proposed in the literature based on clinical and cadaveric studies. Some of the radiological techniques are scanograms, spotograms, preoperative templating, radiographic ruler measurement, the Kramer-splint technique and the nail in box technique [2–11].
The existing literature on the subject provides contrasting recommendations on the ideal preoperative measurement technique and comparison between techniques remains difficult due to differing methodologies used. Foot length can be used as a potential predictor of nail length, as it reflects the overall body size and proportion of the patient [12, 13]. Moreover, foot length is easy to measure and does not require any special equipment or expertise. Previous studies have reported a correlation between foot length and height [12, 13]. However, the correlation between foot length and intramedullary nail length has not been investigated.
In this study, we aimed to develop and validate a 3D-printed foot length scale capable of estimating intramedullary nail lengths for the femur, tibia, and humerus based on simple foot measurements. The device was designed to utilize the European (EU) foot length scale to predict the corresponding nail lengths using regression models derived from retrospective patient data. These models were then used to develop a calibration system for the foot length scale, enabling accurate nail length predictions for preoperative planning.
We hypothesize that foot length can serve as a strong predictor for intramedullary nail length, and that this device can offer a simple, cost-effective solution for orthopedic surgeons. The objectives of this study were to (1) retrospectively analyze the correlation between foot length and intramedullary nail size, (2) design and manufacture a 3D printed foot length scale based on these findings, and (3) prospectively validate the device's accuracy in predicting nail lengths in a clinical setting.
Methods and materials
This study aimed to design a 3D-printed foot length scale that could estimate femur, tibia, and humerus intramedullary nail lengths based on foot length measurements in the European (EU) shoe size scale. The study was conducted in two phases: (1) retrospective data collection and statistical analysis to establish correlations between foot length and intramedullary nail length, and (2) the design, development, and validation of the 3D-printed device.
Retrospective data collection
Data were collected retrospectively from 205 patients who had undergone intramedullary nailing procedures for femur, tibia, or humerus fractures. This included their foot length measured in the EU shoe size scale and the intramedullary nail type and length used during surgery.
Inclusion criteria required patients to be 18 years or older and have complete records of foot length and intramedullary nail size. Patients with congenital foot deformities or incomplete medical records were excluded. Calibration of the data was performed by adjusting for age, BMI, and comorbidities to minimize variability.
A total of consecutive 205 patients that fit the inclusion criteria from January 2023 to December 2024 were enrolled in the study, Intramedullary nailing was performed using standard techniques and implants, according to the manufacturer's recommendations and the surgeon's preference. The nail length was recorded as the length of the nail in centimeters. All nail types were of anterograde types and all nail lengths matched the nail length from end-to-end.
Statistical analysis and correlation models
The data were analyzed using SPSS software (version 26.0). Descriptive statistics were used to summarize the data. The correlation between foot size and nail size was assessed using Pearson's correlation coefficient (r). The correlation was considered strong if r ≥ 0.7, moderate if 0.4 ≤ r < 0.7, and weak if r < 0.4. Linear regression analysis was used to develop a prediction model for nail size based on foot size. The accuracy and precision of the prediction model were evaluated using the mean absolute error (MAE) and the root mean square error (RMSE), respectively. The MAE and RMSE were expressed in centimeters. A lower MAE and RMSE indicated a higher accuracy and precision, respectively. A p-value < 0.05 was considered statistically significant.
Table 1 shows regression equations that were derived based on the retrospective data (See the results sections for details on the analysis).
Table 1.
Equations and inverse equations for calculating the nail length from the foot length
| Measure | Regression Equation | Inverse Equation |
|---|---|---|
| Foot length in cm | ||
| Femur nail length in cm | ||
| Tibia nail length in cm | ||
| Humerus nail length in cm |
Fe Foot length in EU scale, Fc Foot length in cm, N Nail length in cm
Mean absolute error (MAE) and root mean square error (RMSE) were computed for each nail type to evaluate the model's accuracy and predictive performance. These equations were later integrated into the design of the foot length measuring device, where the nail length was determined based on a patient's foot size according to the EU scale.
Foot and nail length scale device
The 3D-printed foot length scale was designed to measure foot length and estimate intramedullary nail length based on the linear equations derived from the retrospective data. The device consisted of two primary components: the main body and the stopper. The device was constructed to accommodate both left and right feet and allowed for precise foot length measurements according to the EU shoe size scale.
The main body featured two lateral rails on which the stopper could glide. The stopper, equipped with flexible wings, snapped securely onto the rails and locked in place with flaps to provide a stable fit. It was designed to be positioned at the longest toe, ensuring accurate foot measurements. Figure 1 shows CAD renderings of the stopper. The heel stopper, located at the rear of the main body, ensured proper alignment of the foot, enabling accurate and reproducible measurements. Figure 2 shows CAD renderings of the Foot Scale device.
Fig. 1.
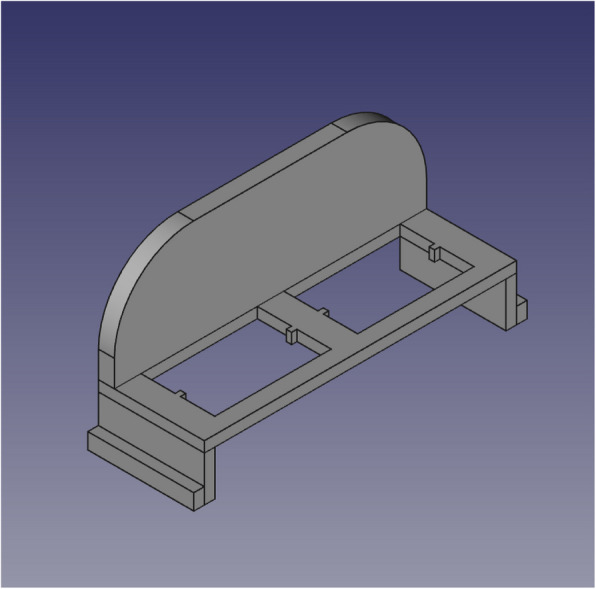
CAD drawings of the stopper part
Fig. 2.
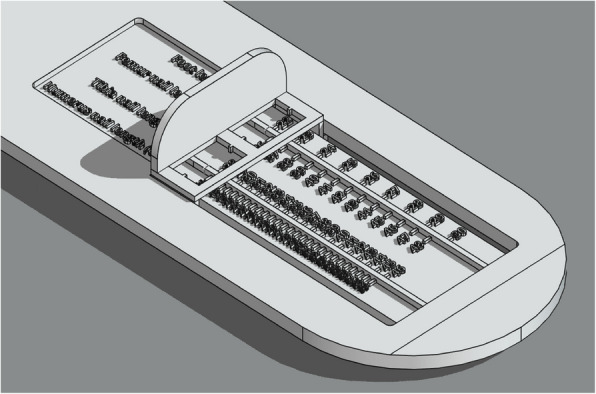
CAD drawings of the foot scale device
The rulers integrated into the device were specifically designed to account for the linear equations derived from the statistical analysis. There were two graduated rulers on the main body:
The first ruler measured foot length in centimeters on one side, and the corresponding femur intramedullary nail length in centimeters on the other. The EU scale was printed alongside the nail length to provide a direct reading.
The second ruler measured tibia nail length on one side and humerus nail length on the other.
The offsets and units for each ruler were calculated as follows:
The foot length in cm ruler started at 22 cm and extended to 30 cm, with 1 cm increments.
The EU scale and femur nail length ruler started at 36 EU (corresponding to 22.3 cm foot length) and ranged up to size 48 EU, with femur nail lengths corresponding to these foot lengths increasing in 6.5 mm steps.
The tibia nail length ruler started at 28 EU (22.3 cm foot length) and ranged up to 46 EU, with tibia nail lengths increasing in 4.25 mm steps.
The humerus nail length ruler started at 16 EU (22.3 cm foot length) and ranged up to 39 EU, with nail lengths increasing in 3.25 mm steps.
These units were designed to be precise enough to cover common ranges for nail lengths and reflect the regression models' output based on foot length. Each ruler was calibrated from the heel stopper, ensuring consistent measurements from the back of the heel to the longest toe (See the results sections for details on the analysis) (Fig. 3).
Fig. 3.
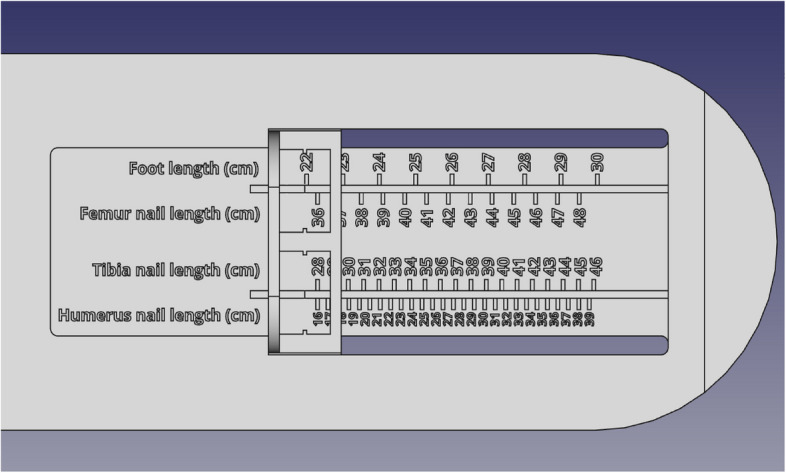
Top view of the rulers for every nail type
3D printing
The foot length scale was modeled using FreeCAD software, this solid model was then converted into a triangular mesh (STL file) within FreeCAD's Mesh Workbench, using the Standard Mesher (Delaunay triangulation) with careful selection of surface deviation of 10 µm and angular deviation of 3° parameters to ensure the accuracy required for a measuring tool, relying on robust internal surface triangulation algorithms to generate a watertight mesh, and the final design was sliced for 3D printing using Lychee Resin Slicer software. Due to the size of the main body, the model was split into two parts using the planar cut tool, enabling it to fit within the build volume of the 3D printer.
The device components were printed using an Elegoo Saturn 2 printer, with TR300 Ultra-High Temp 3D Printing Resin chosen for its durability and precision [14]. The resin had a cost of approximately 64 USD per kilogram, and the total resin volume used for the print was 132.65 mL. The prints were rotated 60° on the Y-axis to avoid staircase stepping artifacts and ensure optimal build volume use.
The main body of the device measured 360 mm (L) × 100 mm (W) × 40 mm (H), while the stopper measured 45 mm (L) × 60 mm (W) × 33 mm (H). The parts were printed with a total print time of approximately 6 h and 34 min. The burn-in layers were set to four, with an exposure time of 25 s per layer. For the normal layers, a layer thickness of 50 µm was used, with an exposure time of 2.5 s. Figure 4 shows details of the printing parameters used.
Fig. 4.
Printing settings for lychee slicer
Post-printing, the components were cleaned in an isopropyl alcohol (IPA) bath and then UV-cured for 20 min to ensure full hardening. The two parts of the main body were then assembled and glued heat resistant epoxy resin, and the stopper was fitted into the rails slots. After assembled, the parts dimensions were measured to ensure dimensional accuracy. Mechanical stability testing was not performed as it was deemed unnecessary for this specific application.
Prospective validation
The 3D-printed device was prospectively validated in a clinical setting with patients undergoing intramedullary nailing procedures. For each patient, foot length was measured using the device, and the estimated femur, tibia, or humerus nail length was recorded. During surgery, the actual intramedullary nail length used was compared to the predicted values generated by the device.
Accuracy was evaluated by calculating the mean prediction error for each nail type with the device providing accurate estimations. Mean absolute error (MAE) and root mean square error (RMSE) were calculated.
Results
Retrospective analysis
A total of 205 patients were enrolled in the retrospective study, of which 103 were males and 102 were females. The mean age of the patients was 43.6 ± 15.2 years, ranging from 18 to 78 years.
The mean measured foot length of the patients was 38.7 ± 2.4 EU, ranging from 34 to 45 EU. The mean height of the patients was 169.4 ± 9.6 cm, ranging from 147 to 192 cm. The mean nail length for the femur, tibia and humerus were 41.9 ± 3.2 cm, 35.9 ± 3.6 cm and 22.3 ± 2.8 cm, respectively. The fractured bone breakdown of the patients was femur (n = 75, 36.5%), tibia (n = 88, 42.9%), and humerus (n = 42, 20.4%). The nail length for each bone are shown in Table 2. The mean nail length for the femur, tibia and humerus were 41.9 ± 3.2 cm, 35.9 ± 3.6 cm and 22.3 ± 2.8 cm, respectively. The ratios between the height, femur, tibia and humerus nail length and the foot length (EU), and the coefficient of reliability (CR) for these ratios are shown in Table 2. The CR values for these ratios were 0.97, 0.99, 0.96, 0.85, respectively, indicating a high reliability of the ratios.
Table 2.
Ratios between height/femur/tibia/humerus nail length and foot length, and coefficient of reliability
| Ratio | Mean ± SD | CR |
|---|---|---|
| Height/Foot length (EU) | 6.52 ± 0.12 | 0.97 |
| Femur nail length/Foot length (EU) | 0.98 ± 0.07 | 0.99 |
| Tibia nail length/Foot length (EU) | 0.85 ± 0.12 | 0.96 |
| Humerus nail length/Foot length (EU) | 0.61 ± 0.15 | 0.85 |
Regression analysis
The linear regression analysis showed that foot length was a good predictor of femur nail length, with a near-perfect match. The regression equation for the femur nail length was where y is the femur nail length in cm and F is the foot length in EU. The coefficient of determination (R2) value for this model was 0.98 and the standard error of the estimate (SEE) was 0.66 cm.
Tibia nail length was also correlated with foot length, but with a larger margin of error. The regression equation for the tibia nail length was: where y is the tibia nail length in cm and F is the foot length in EU. The R2 value for this model was 0.91 and the SEE was 1.02 cm.
Humerus nail length was proportional to foot length, but with a lower coefficient of determination. The regression equation for the humerus nail length was: where y is the humerus nail length in cm and x is the foot length in EU. The R2 value for this model was 0.85 and the SEE was 1.14 cm.
The equations for calculating the nail length from the foot size for each bone are shown in Table 3. Scatter plots for the correlation between reported foot length and corresponding intramedullary nail length are shown in Fig. 5.
Table 3.
Equations and inverse equations for calculating the nail length from the foot length
| Measure | Regression Equation | Inverse Equation |
|---|---|---|
| Foot length in cm | ||
| Femur nail length in cm | ||
| Tibia nail length in cm | ||
| Humerus nail length in cm |
Fe Foot length in EU scale, Fc Foot length in cm, N Nail length in cm
Fig. 5.
Scatter plots for the correlation between reported foot length and corresponding intramedullary nail length
Offset and step size calculation
Femur nail calculations
To compute the starting, ending units and step size for the femur nail length ruler, we choose the start, and end foot length in cm to be 22.3 cm, and 30.2 cm which is roughly equal to 36, and 48 EU scales respectively. To get the starting and ending units for the femur nail ruler we plug the starting and ending foot lengths into Fe = Fc × 1.528 + 1.926 to get Foot length in EU scale (Fe) and then into N = Fe × 1.02 – 0.75 to get the nail’s length (N), this yields us the starting and ending units for femur nails lengths of 35.97, and 48.28 respectively which are rounded to 36, and 48 respectively. The step size S = dFc / dN = (Fc2-Fc1) / (N2-N2) for each unit is slope between two foot lengths (Fc1, and F2) and two corresponding nail length units (N1, and N2), to compute the step size for the femur nail we plug the corresponding values in into the step size equation to get a step size of 6.58 mm which is rounded to 6.5 mm for simplicity reasons. Starting, ending offsets, and step size for each nail type ruler are shown in Table 4.
Table 4.
Starting, ending offsets, and step size for each nail type ruler
| Nail type | Fc1 (cm) | Fc2 (cm) | N1 | N2 | N1 (round) | N2 (round) | dN (unit) | dFc (cm) | Step size (mm) |
|---|---|---|---|---|---|---|---|---|---|
| Femur nail | 22.3 | 30.2 | 35.97 | 48.28 | 36 | 48 | 12 | 7.9 | 6.58 |
| Tibia nail | 22.3 | 30.2 | 28.33 | 45.56 | 28 | 46 | 18 | 7.9 | 4.39 |
| Humerus nail | 22.3 | 30.2 | 16.37 | 38.62 | 16 | 39 | 23 | 7.9 | 3.43 |
Fe Foot length in EU scale, Fc Foot length in cm, N Nail length in cm, Fc1 Starting foot length in cm, Fc2 Ending foot length in cm, N1 Starting nail length, N2 Ending nail length, dFc Delta foot length in cm, dN Delta nail length
Tibia nail calculations
To compute the starting, ending units and step size for the tibia nail length ruler, we choose the start, and end foot length in cm to be 22.3 cm, and 30.2 cm which is roughly equal to 36, and 48 EU scales respectively. To get the starting and ending units for the tibia nail ruler we plug the starting and ending foot lengths into Fe = Fc × 1.528 + 1.926 to get Foot length in EU scale (Fe) and then into N = Fe × 1.427—23.043 to get the nail’s length (N), this yields us the starting and ending units for femur nails lengths of 28.33, and 45.56 respectively which are rounded to 28, and 46 respectively. The step size S = dFc / dN = (Fc2-Fc1) / (N2-N2) for each unit is slope between two foot lengths (Fc1, and F2) and two corresponding nail length units (N1, and N2), to compute the step size for the tibia nail we plug the corresponding values in into the step size equation to get a step size of 4.39 mm which is rounded to 4.25 mm for simplicity reasons. Starting, ending offsets, and step size for each nail type ruler are shown in Table 4.
Humerus nail calculations
To compute the starting, ending units and step size for the humerus nail length ruler, we choose the start, and end foot length in cm to be 22.3 cm, and 30.2 cm which is roughly equal to 36, and 48 EU scales respectively. To get the starting and ending units for the humerus nail ruler we plug the starting and ending foot lengths into Fe = Fc × 1.528 + 1.926 to get Foot length in EU scale (Fe) and then into N = Fe × 1.843—49.975 to get the nail’s length (N), this yields us the starting and ending units for femur nails lengths of 16.37, and 38.62 respectively which are rounded to 16, and 39 respectively. The step size S = dFc / dN = (Fc2-Fc1) / (N2-N2) for each unit is slope between two foot lengths (Fc1, and F2) and two corresponding nail length units (N1, and N2), to compute the step size for the humerus nail we plug the corresponding values in into the step size equation to get a step size of 3.43 mm which is rounded to 3.25 mm for simplicity reasons. Starting, ending offsets, and step size for each nail type ruler are shown in Table 4.
Prospective validation
The prospective validation of the 3D-printed device was conducted using data from 86 patients, with the goal of accurately estimating intramedullary nail lengths for the femur, tibia, and humerus based on foot length in the EU scale. The accuracy of the device was evaluated by calculating the mean prediction error for each nail type and comparing the predicted nail lengths to the actual lengths used in surgical procedures. Both the Mean Absolute Error (MAE) and the Root Mean Square Error (RMSE) were computed to provide a detailed assessment of the device’s performance.
For the femur nails, the device provided highly accurate predictions. The calculated MAE for femur nails was 0.67 cm, indicating that, on average, the predicted nail lengths deviated from the actual lengths by less than 1 cm. The RMSE was 0.85 cm, reflecting the close clustering of predicted values around the actual measurements, with minimal variability.
In the case of tibia nails, the MAE was 0.74 cm, similar to the femur results, demonstrating a comparable level of accuracy. The RMSE for tibia predictions was slightly higher at 1.03 cm, suggesting a wider distribution of errors but still within clinically acceptable margins. This broader range likely reflects the variability in tibia anatomy among patients.
For humerus nails, the device showed the greatest precision, with the lowest MAE of 0.62 cm. The RMSE for humerus predictions was 0.78 cm, underscoring the device’s strong accuracy for this bone type. The results indicate that the predictions for humerus nail lengths consistently fell close to the actual values, with few outliers.
The validation of the device demonstrated that it performs reliably across all three nail types. Table 5 summarizes the MAE and RMSE values for each type of nail used in the study.
Table 5.
Mean Absolute Error (MAE) and Root Mean Square Error (RMSE) for each nail type
| Nail Type | MAE (cm) | RMSE (cm) | N |
|---|---|---|---|
| Femur | 0.67 | 0.85 | 30 |
| Tibia | 0.74 | 1.03 | 30 |
| Humerus | 0.62 | 0.78 | 26 |
Discussion
The device’s potential for use in preoperative planning is particularly noteworthy. Traditionally, determining the appropriate intramedullary nail length requires radiographic measurements or intraoperative adjustments [3, 5, 9, 10], both of which can introduce variability and extend surgical time. By offering a non-invasive, quick, and accurate method for estimating nail lengths based on foot size, the device has the potential to streamline the surgical workflow, reduce the reliance on radiographs, and improve overall surgical efficiency. Additionally, the device could be particularly beneficial in resource-limited settings where access to advanced imaging technologies is constrained.
A prominent finding of this study was that foot length was a good predictor of intramedullary nail length for long bone fractures, especially for the femur. The linear regression analysis showed that self-reported foot size had a strong correlation with femur nail length, with a near-perfect match. The prediction of femur nail length from self-reported foot size had a high precision and accuracy, with a low SEE and MAE (R = 0.99). Tibia nail length was also correlated with self-reported foot size, but with a slight margin of error (R = 0.96). Humerus nail length was proportional to self-reported foot size, but with a lower coefficient of determination (R = 0.85). The prediction of height from foot size was also performed and compared with the actual height of the patients (R = 0.97).
The development and validation of the 3D-printed foot length measuring device aimed to provide a practical and non-invasive method for estimating intramedullary nail lengths for the femur, tibia, and humerus based on foot size in the EU scale. The results of the prospective validation demonstrate that the device offers high accuracy, with consistently low error margins across all three bone types. The findings suggest that foot length is a reliable predictor of nail length, which may offer significant advantages in clinical settings, particularly in preoperative planning and intraoperative decision-making.
Despite these promising findings, several limitations must be considered. The device’s accuracy could be impacted by atypical foot anatomies, such as in patients with deformities or size discrepancies between their feet and overall body proportions [15, 16]. Future studies could further investigate the device’s performance in these populations and explore whether additional adjustments or calibration methods are required for such cases.
The use of 3D printing technology in developing the foot length measuring device offers significant advantages, particularly in terms of customization, precision, and practicality. One of the primary benefits of employing 3D printing, specifically stereolithography (SLA) technology, is its ability to produce highly detailed and precise models [17, 18]. This is crucial for a medical device where exact measurements, such as the correlation between foot length and intramedullary nail length, must be consistently reliable. The fine resolution of SLA printing ensures that the device can feature accurate graduations and intricate details, such as the graduated rulers that align with clinical requirements [18]. These high-fidelity characteristics are essential to ensure that the device provides consistent and accurate measurements during surgical planning and intraoperative use.
Another critical benefit of using 3D printing, particularly in this context, is the ability to rapidly prototype and iterate designs. During the development of the device, the design could be easily adjusted and reprinted to refine both the ergonomics and the accuracy of the measurements. This flexibility allows for quick alterations based on feedback from clinicians or validation trials, leading to an optimized final product [18–20]. The cost-effectiveness of 3D printing, compared to traditional manufacturing techniques, also makes it a viable option for producing customized or small-batch medical devices. Customization is especially relevant for foot size measuring devices, where patient populations can exhibit wide variability, and bespoke or adaptable models may enhance clinical utility [18, 19].
The choice of SLA technology also offers benefits in terms of surface smoothness and structural integrity, which are particularly important for a device used in a clinical environment. The smooth surfaces reduce friction in parts such as the stopper, which needs to glide smoothly along the rails of the device without sticking. This smooth operation is necessary to maintain the precision of measurements, as any irregularity in movement could introduce errors, Additionally, Smoothness is paramount is ensuring the ease of cleansing of biological fluids such as blood and synovial fluids which can lodge in the nooks and crannies of an irregular surface provided otherwise by other printing technologies such as FDM [17, 18]. Furthermore, the dimensional accuracy achieved with SLA printing is critical in ensuring that the graduated rulers display foot size and nail length with exact correspondence to real-world values.
In terms of material choice, the use of TR300 Ultra-High Temp 3D Printing Resin is a strategic decision, providing several advantages. Firstly, this resin's high-temperature resistance allows it to withstand autoclave sterilization, an essential requirement for any medical device that may be used in a clinical setting. The ability to sterilize the device ensures that it meets stringent infection control protocols, making it safe for repeated use in sterile environments such as operating rooms. This property also increases the device’s durability, allowing it to maintain its structural and dimensional integrity even after multiple sterilization cycles [14].
In conclusion, this study demonstrates that the 3D-printed foot length measuring device is a highly accurate tool for estimating intramedullary nail lengths for the femur, tibia, and humerus. The device’s ease of use, combined with its precise predictions, makes it a valuable addition to the orthopedic surgical toolkit. Further research should focus on expanding its application to a broader range of patient populations and exploring additional predictive variables to enhance its utility even further. Nonetheless, the results presented here provide strong evidence of the device’s clinical potential in improving surgical outcomes and streamlining the preoperative planning process.
Conclusion
In conclusion, this study showed that foot length was a good predictor of intramedullary nail length in long bone fractures, especially for the femur. Warranting future applications of anthropology in orthopaedic and traumatology practice. The development of the 3D-printed foot length measuring device offers a practical solution for accurately estimating intramedullary nail lengths for the femur, tibia, and humerus. By integrating precise regression equations, the device streamlines preoperative planning and reduces the need for radiographic imaging. The use of stereolithography (SLA) technology provided high precision in the device's design, while the sterilizable resin ensures repeated clinical use. Prospective validation on 86 patients confirmed the device's accuracy, with minimal error across all nail types. However, the use of the device as a predictor of intramedullary nail length also has some limitations and challenges, as the use of foot size may not be applicable for patients with deformities or injuries of the foot, which may alter the foot size and shape.
Supplementary Information
Acknowledgements
No acknowledgment to declare.
Statement of human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Clinical trial number
Not applicable.
Authors’ contributions
All authors have made substantial contributions to all of the following: the conception and design of the study by Z.C., or acquisition of data by Z.C., B.D. and S.A., or analysis and interpretation of data by Z.C, drafting the article by Z.C. or revising it critically for important intellectual content by S.A., Y.FE. EM.B., MA.B. and I.A., all authors approved of the version to be submitted.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study was approved by the Scientific Committee and the Medical Council of our establishment. Written informed consent was obtained from the all patients for publication of this report and any accompanying images in accordance with the principles of the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from all patients for their anonymized information to be published in this study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wong Wei Kang N, Tan WPJ, Phua YMC, et al Intramedullary nail: the past, present and the future – a review exploring where the future may lead us. Orthop Rev 13:25546. 10.52965/001c.25546. [DOI] [PMC free article] [PubMed]
- 2.Waldron VD. Predicting intramedullary nail length. Am J Orthop Belle Mead NJ. 1998;27:383. [PubMed] [Google Scholar]
- 3.Venkateswaran B, Warner RM, Hunt N, et al. An easy and accurate preoperative method for determining tibial nail lengths. Injury. 2003;34:752–5. 10.1016/s0020-1383(02)00370-4. [DOI] [PubMed] [Google Scholar]
- 4.Blair S. Estimating tibial nail length using forearm referencing. Injury. 2005;36:160–2. 10.1016/j.injury.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 5.Fischmeister MF, Lang T, Reichl C, Wechselberger C. How to predict requisite nail length in tibial fractures. Arch Orthop Trauma Surg. 1994;113:194–5. 10.1007/BF00441830. [DOI] [PubMed] [Google Scholar]
- 6.Hodgson S. AO principles of fracture management. Ann R Coll Surg Engl. 2009;91:448–9. 10.1308/003588409X432419f. [Google Scholar]
- 7.Krettek C, Blauth M, Miclau T, et al. Accuracy of intramedullary templates in femoral and tibial radiographs. J Bone Joint Surg Br. 1996;78:963–4. 10.1302/0301-620x78b6.1284. [DOI] [PubMed] [Google Scholar]
- 8.Issac RT, Gopalan H, Abraham M, et al. Preoperative determination of tibial nail length: an anthropometric study. Chin J Traumatol. 2016;19:151–5. 10.3760/cma.j.issn.1008-1275.2016.03.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearson J, Hess M, McGwin G, Quade J. Accurate prediction of antegrade and retrograde femoral intramedullary implant length from patient-reported height. J Orthop Trauma. 2019;33:503. 10.1097/BOT.0000000000001560. [DOI] [PubMed] [Google Scholar]
- 10.Hegde AS, Shetty CB, Joseph N, et al. Preoperative estimation of humerus intramedullary nail length using clinical landmarks. Chin J Traumatol. 2023;26:256–60. 10.1016/j.cjtee.2023.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alao U, Liew I, Yates J, Kerin C. Correlation between the length from the elbow to the distal interphalangeal joint of the little finger and the length of the intramedullary nail selected for femoral fracture fixation. Injury. 2018;49:2058–60. 10.1016/j.injury.2018.08.024. [DOI] [PubMed] [Google Scholar]
- 12.Zeybek G, Ergur I, Demiroglu Z. Stature and gender estimation using foot measurements. Forensic Sci Int. 2008;181:54.e1-54.e5. 10.1016/j.forsciint.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Xiong S, Goonetilleke RS, Witana CP, Lee Au EY. Modelling foot height and foot shape-related dimensions. Ergonomics. 2008;51:1272–89. 10.1080/00140130801996147. [DOI] [PubMed] [Google Scholar]
- 14.TR300 Ultra-High Temp 3D Printing Resin. In: Phrozen Technol. https://phrozen3d.com/products/tr300-ultra-high-temp-resin. Accessed 15 Aug 2024
- 15.Krauss I, Grau S, Mauch M, et al. Sex-related differences in foot shape. Ergonomics. 2008;51:1693–709. 10.1080/00140130802376026. [DOI] [PubMed] [Google Scholar]
- 16.Gwani AS, Salihu AT, Garba IS, Rufa’i AA,. Estimation of stature from radiographic measurement of foot dimensions: truncated foot length may be more reliable than full foot length. J Forensic Leg Med. 2017;46:53–7. 10.1016/j.jflm.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Deshmane S, Kendre P, Mahajan H, Jain S. Stereolithography 3D printing technology in pharmaceuticals: a review. Drug Dev Ind Pharm. 2021;47:1362–72. 10.1080/03639045.2021.1994990. [DOI] [PubMed] [Google Scholar]
- 18.Lakkala P, Munnangi SR, Bandari S, Repka M. Additive manufacturing technologies with emphasis on stereolithography 3D printing in pharmaceutical and medical applications: A review. Int J Pharm X. 2023;5:100159. 10.1016/j.ijpx.2023.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martelli N, Serrano C, van den Brink H, et al. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016;159:1485–500. 10.1016/j.surg.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Balaji NS, Velmurugan C, Saravana Kumar M, et al. Experimental investigation on mechanical properties of fdm-based nylon carbon parts using ann approach. Surf Rev Lett. 2023;30:2350028. 10.1142/S0218625X23500282. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.