Abstract
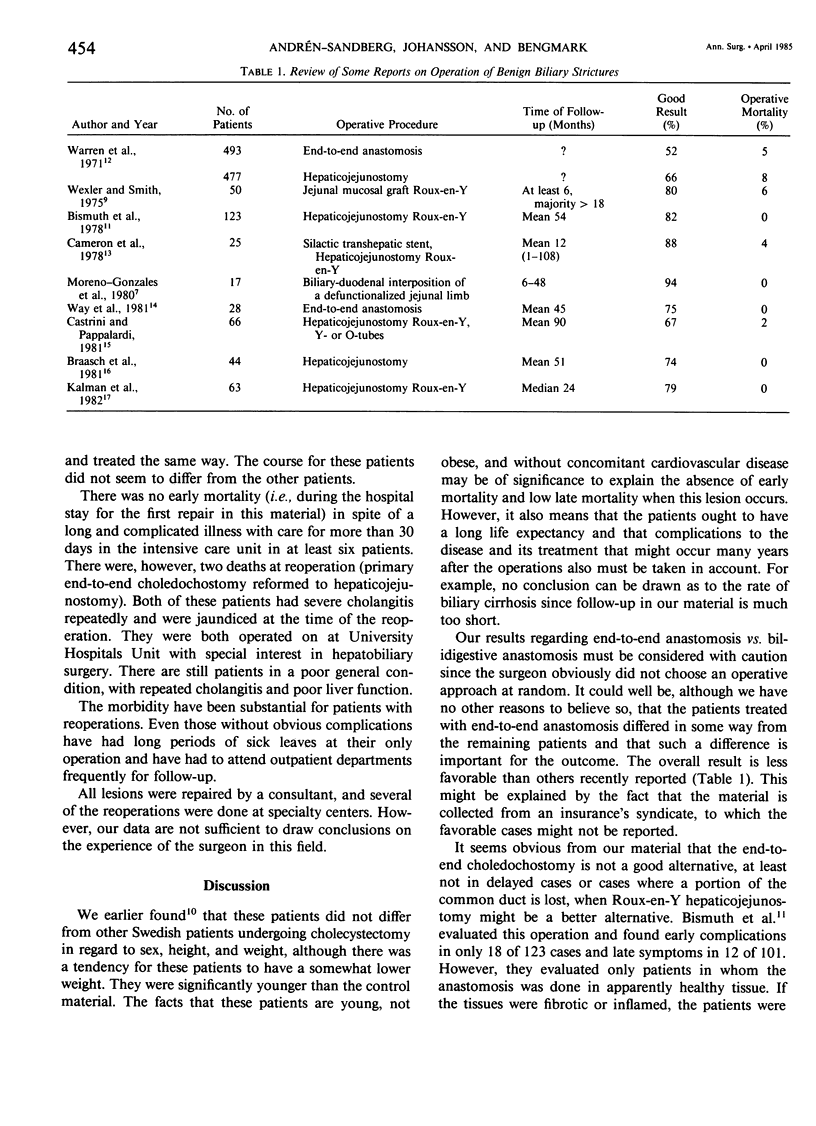
Sixty-five cases of accidental lesion of the choledochus at cholecystectomy reported from 51 Swedish hospitals to the Patients' Insurance Syndicate in Stockholm 1975-1981 were studied. The results were evaluated as to the time of detection and the primary surgical repair done. Fifty-five of the 65 lesions were detected and repaired at the cholecystectomy and ten were detected and repaired the first 10 days after the primary operation. In 38 of 55 lesions detected before surgery, an end-to-end choledochostomy was performed. Good results without further surgical intervention were achieved in 22%. The 17 other preoperatively detected lesions were treated with choledocho/hepaticoenterostomy, and good results were achieved without further surgical intervention in 54%. Of the ten patients in whom the lesions were detected after surgery, three were reconstructed with an end-to-end choledochostomy; all of these developed obstruction that led into further reoperations. In the remaining seven patients the lesions were repaired within 10 days with a choledocho/hepaticoenterostomy; three of them did not require further surgical intervention and four had to be reoperated. There was no mortality at the first repair, but two cases of hospital mortality at reoperations. However, the morbidity have been substantial for patients with as well as without obvious further surgical complications. The results indicate that in this selected group choledocho/hepaticoenterostomy should be the procedure of choice. However, the accumulated rate of biliary strictures increased with time, which requires a considerably longer follow-up to know the end results of this of avoidable complication to "a straightforward cholecystectomy."
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andrén-Sandberg A., Alinder G., Bengmark S. Accidental lesions of the common bile duct at cholecystectomy. Pre- and perioperative factors of importance. Ann Surg. 1985 Mar;201(3):328–332. [PMC free article] [PubMed] [Google Scholar]
- BORGSTROM S. Operative injury to the choledochus. Acta Chir Scand. 1959 Nov 25;118:25–31. [PubMed] [Google Scholar]
- Bismuth H., Franco D., Corlette M. B., Hepp J. Long term results of Roux-en-Y hepaticojejunostomy. Surg Gynecol Obstet. 1978 Feb;146(2):161–167. [PubMed] [Google Scholar]
- Braasch J. W., Bolton J. S., Rossi R. L. A technique of biliary tract reconstruction with complete follow-up in 44 consecutive cases. Ann Surg. 1981 Nov;194(5):635–638. doi: 10.1097/00000658-198111000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron J. L., Gayler B. W., Zuidema G. D. The use of silastic transhepatic stents in benign and malignant biliary strictures. Ann Surg. 1978 Oct;188(4):552–561. doi: 10.1097/00000658-197810000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castrini G., Pappalardo G. Iatrogenic strictures of the bile ducts: our experience with 66 cases. World J Surg. 1981 Sep;5(5):753–758. doi: 10.1007/BF01657948. [DOI] [PubMed] [Google Scholar]
- Kalman P. G., Taylor B. R., Langer B. Iatrogenic bile-duct strictures. Can J Surg. 1982 May;25(3):321–324. [PubMed] [Google Scholar]
- Moreno-González E., Sanmartin J. H., Azcoita M. M., Serna A. B. Reconstruction of the biliary tract using biliary-duodenal interposition of a defunctionalized jejunal limb. Surg Gynecol Obstet. 1980 May;150(5):678–682. [PubMed] [Google Scholar]
- Rutledge R. H. Methods of repair of noncircumferential bile duct defects. Surgery. 1983 Feb;93(2):333–342. [PubMed] [Google Scholar]
- Warren K. W., Mountain J. C., Midell A. I. Management of strictures of the biliary tract. Surg Clin North Am. 1971 Jun;51(3):711–731. doi: 10.1016/s0039-6109(16)39447-6. [DOI] [PubMed] [Google Scholar]
- Way L. W., Bernhoft R. A., Thomas M. J. Biliary stricture. Surg Clin North Am. 1981 Aug;61(4):963–972. doi: 10.1016/s0039-6109(16)42492-8. [DOI] [PubMed] [Google Scholar]
- Wexler M. J., Smith R. Jejunal mucosal graft: a sutureless technic for repair of high bile duct strictures. Am J Surg. 1975 Feb;129(2):204–211. doi: 10.1016/0002-9610(75)90299-8. [DOI] [PubMed] [Google Scholar]


