Abstract
Gastrointestinal infections in Germany account for 24.5 million outpatient visits annually. To enhance outbreak detection and trend monitoring, we developed and validated a syndrome definition for syndromic surveillance of gastrointestinal infections in emergency departments. We selected presenting complaints (Canadian Emergency Department Information System) and diagnoses (ICD-10) to develop the syndrome definition. Validation involved cross-correlation analysis of syndromic and laboratory-based surveillance trends (norovirus-gastroenteritis, rotavirus-gastroenteritis, campylobacteriosis and salmonellosis notifications). We included emergency departments from the German AKTIN registry with continuous data transmission (01/2019–06/2023). Our novel syndrome definition combined complaints (diarrhoea, vomiting, nausea) and diagnoses (intestinal infectious diseases). Across 864,353 visits in 7 emergency departments, 2.1% (n = 18,158) were gastrointestinal infection cases. Of those, 57% (n = 10,424) were female; 23% were aged 0–19 years (n = 4108); and 23% 20–39 years (n = 4116). Trends were similar between surveillance systems. Cross-correlation was 0.73 (95%-confidence interval 0.61–0.85; p < 0.001) at lag − 1, indicating a 1-week relative reporting delay of laboratory-based surveillance. Coherent trends and significant cross-correlation validated our syndrome definition. This novel automated syndromic surveillance complements laboratory-based surveillance while offering improved timeliness and reduced workload. Therefore, it was implemented in Germany’s national routine surveillance of emergency departments.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-025-13675-z.
Keywords: Emergency service, hospital; Emergency department; Public health surveillance; Syndromic surveillance; Sentinel surveillance; Gastrointestinal infection; Gastrointestinal diseases; Gastroenteritis
Subject terms: Public health, Epidemiology, Gastroenteritis, Gastrointestinal diseases, Infectious diseases, Diseases, Health care, Signs and symptoms, Digestive signs and symptoms, Nausea, Vomiting
Introduction
Gastrointestinal infections are of viral, bacterial, fungal or parasitic aetiology and cause gastroenteritis, which is an inflammation of stomach and intestine. The main symptoms are nausea, vomiting and diarrhoea1. These infections are among the top eight causes of death globally2, and burden health care services considerably. In 2008 and 2009, acute gastrointestinal illness was estimated to cause about 24.5 million outpatient visits and 19.9 million hospital days per year in Germany’s adult population3. Norovirus-gastroenteritis, campylobacteriosis, and rotavirus-gastroenteritis ranked among the top four in incidence of notifiable diseases in Germany in 2019 prior to the COVID-19 pandemic4. Surveillance of gastrointestinal infections is important to monitor disease trends and identify gastrointestinal outbreaks. It helps to assess the public health impact and better understand disease mechanisms and causes. Thereby surveillance improves prevention and outbreak detection to enable timely public health action.
Data on the occurrence of gastrointestinal infectious diseases in Germany is collected through the statutory surveillance system, where the majority of gastrointestinal infectious disease notifications are laboratory confirmed. Occasionally, some notifications are included based on clinical presentation and an epidemiological link alone. Importantly, this epidemiological link is again to another laboratory-confirmed case5. Although notifiable, gastrointestinal outbreaks are often not reported. Laboratory diagnostics and reporting delays cause time lags. The existing system could be complemented by establishing syndromic surveillance, which is not based on laboratory diagnoses, but on clinical signs and symptoms that constitute a “syndrome”6.
Emergency departments are suited for syndromic surveillance. Firstly, they routinely collect symptom-based information such as presenting complaints or preliminary diagnosis. Secondly, the specific setting of emergency departments is highly relevant for surveillance, since emergency departments often serve as the first point of contact for patients with the healthcare system. Surveillance in emergency departments supports the description of trends and timely detection of outbreaks, particularly regarding severe gastrointestinal infections. Additionally, the reduced specificity of syndromic surveillance may increase sensitivity for the detection of unspecific, yet relevant public health events.
In Germany, syndromic emergency department surveillance was established at the Robert Koch Institute in 2018. The system uses routinely collected case-based data provided daily by the AKTIN emergency department registry7,8. Based thereupon, the Robert Koch Institute publishes an automated weekly emergency department report9, including syndromes such as (severe) acute respiratory infection or influenza-like illness10. Gastrointestinal infections were not initially included in routine reporting. Preliminary syndrome definitions for gastrointestinal infections were developed, but required validation and further adaptation for implementation in surveillance reporting11.
To describe disease trends and facilitate timely outbreak detection, we aimed to develop and implement syndromic surveillance of gastrointestinal infections in emergency departments in Germany. Therefore, our objectives were to further develop a syndrome definition for gastrointestinal infections, to describe the distribution of identified cases over time and to validate the syndrome definition by comparison with laboratory-based reference data.
Methods
Development of a syndrome definition for gastrointestinal infections
We developed a syndrome definition (case definition) for gastrointestinal infections by selecting and combining ICD-10 coded diagnosis and presenting complaints. This was based on definitions from a previous study11 and informed by similar syndrome definitions found in the literature12,13. The syndrome definition was developed in consultation with the unit for gastrointestinal infections at the Robert Koch Institute, and further discussed and refined in collaboration with the AKTIN Research Group and clinicians from participating emergency departments.
Study data bases
We performed a retrospective registry study using data provided by the AKTIN emergency department registry7,8. AKTIN provides the emergency department surveillance system at the Robert Koch Institute with case-based routine emergency department data on a daily basis (AKTIN data request ID2019_003). The data is then transformed according to the NoKeDa (NotaufnahmeKernDatensatz) data standard14 and stored in a local database at the Robert Koch Institute. Participation in the AKTIN emergency department registry is voluntary for emergency departments, making the sample noncomprehensive and not necessarily geographically representative. Each record corresponds to one patient visit to the emergency department, described by a unique identifier. Since the data is anonymized, multiple visits for the same patient cannot be linked.
We included the following variables in our analysis: emergency department, date of visit, sex, age (in age groups 0–19, 20–39, 40–59, 60–79, 80 + years), presenting complaints (according to the Canadian Emergency Department Information System—Presenting Complaint List V.3.015), diagnosis coded according to the German modification of the 10th International Statistical Classification of Diseases and Related Health Problems (ICD-10) and ICD-10 diagnosis certainty16. We removed the relatively rare sex category “other” to ensure data protection and patient privacy in all analyses. We exported data from the database on 1 August 2023.
For the laboratory-based reference, we combined notifications of norovirus-gastroenteritis, rotavirus-gastroenteritis, campylobacteriosis, and salmonellosis from the German statutory electronic surveillance system (SurvNet) by week of notification. We included notifications fulfilling case definitions according to §11 (2) Infection Protection Act5. We did not include other notifiable gastrointestinal diseases (e.g. giardiasis, shigellosis) due to relatively small case numbers. SurvNet data was exported on 20 August 2023.
Study period, study population and selection of emergency departments
The study period ranged from calendar week 2/2019 (7 January 2019) to week 25/2023 (25 June 2023), in which data from a total of 43 emergency departments across 10 German federal states was available. Of those, we selected departments that fulfilled pre-defined quality criteria. Firstly, we assessed the continuous transmission of data, which was defined as a maximum of 1 week without any transmitted patient visits during the study period. Secondly, we considered the quality of two main variables, presenting complaint and ICD-10 diagnosis. We allowed a maximum of 1 week with 100% missing values and no trend for each of the two variables during the study period. We accepted emergency departments that consistently reported only one of the two variables (i.e. one variable continuously missing). In this case the syndrome was consistently coded using only one variable. Data from one emergency department was excluded due to additional technical problems with data quality. This strict quality control reduces fluctuations in our indicator due to variations in data quality, which could distort the subsequent absolute trend and cross-correlation analysis. The study population includes all patients that visited the selected emergency departments in the study period.
Statistical analysis, internal and external validation of syndrome definition
Using frequency measures, we described emergency department visits as well as cases of gastrointestinal infections by sex and age groups. We described weekly cases of gastrointestinal infections over time and analysed trends and seasonal patterns through time series analysis.
To internally validate the use of presenting complaints for the selection of gastrointestinal infection cases, we performed an additional analysis. We selected cases based solely on presenting complaints “254—Diarrhea” and “257—Nausea and/or vomiting”. Subsequently we analysed the frequencies of ICD-10 diagnosis captured and checked their consistency with gastrointestinal infections. For external validation of the syndrome definition, we assessed the correlation between cases of gastrointestinal infections in emergency departments (“emergency department indicator”) and data for gastrointestinal infectious diseases notifications from laboratory-based surveillance (“reference indicator”). First, we visually compared the trends of both the emergency department indicator and the reference indicator. We then quantified the correlation by estimating cross-correlation coefficients between the two indicators, both overall and stratified by sex and age groups. We estimated the standard error with the moving block bootstrap method17. We applied Loess smoothing for estimating the trend and the corresponding remainder components of each time series as a basis for the block bootstrap, and we defined blocks of length 17 each. Based on an approximation with Student’s t-distribution, we calculated confidence intervals and statistical significance (p-values) for cross-correlation coefficients at specific time lags.
We used the statistical software R (Version 4.2.2)18 and RStudio (Version 2023.03.0 Build 386)19, including the tidyverse, lubridate, ISOweek, Readxl, naniar, flextable, gtsummary, stringr, tsibble, slider, ggh4x, ggpubr, tseries packages.
Results
Syndrome definition for gastrointestinal infections
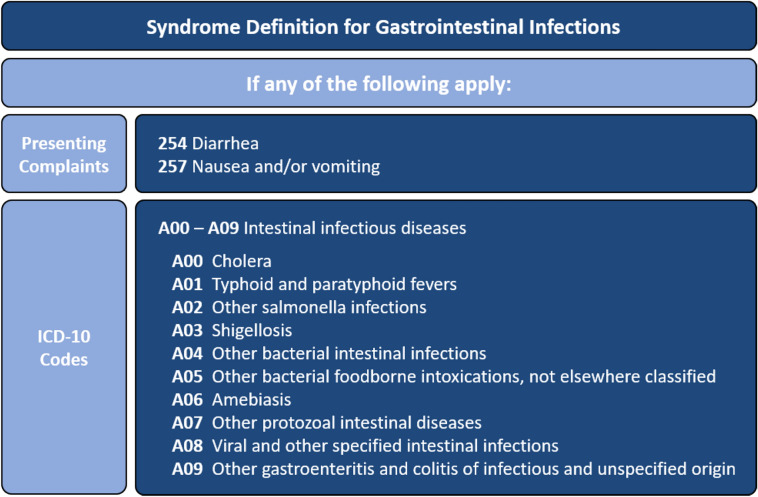
Our novel syndrome definition combined presenting complaints “254—Diarrhea” and “257—Nausea and/or vomiting” with the ICD-10 diagnoses group “A00—A09 Intestinal infectious diseases” (Fig. 1). Visits were classified as cases if they were coded with any of the relevant presenting complaints or ICD-10 diagnoses. For ICD-10 diagnosis, we accepted the diagnoses with certainty levels of “G” (confirmed), “V” (suspected), “Z” (previous) or missing certainty level, but not “A” (excluded).
Fig. 1.
Syndrome definition used for surveillance of gastrointestinal infections in emergency departments by presenting complaint according to the Canadian Emergency Department Information System and ICD-10 codes. Germany, 2019–2023.
We determined that the syndrome definitions “GI unspecific without bleeding” and “bloody diarrhoea” from a previous project11 were unsuitable for routine surveillance. Based on expert discussions regarding clinical coding practices, we identified two key reasons. First, they included presenting complaints based on the Manchester Triage System, which is currently unavailable in the AKTIN registry data. Secondly, the majority of cases with “bloody diarrhoea” were assigned ICD-10 codes “K92.1 Melaena” or “K92.2 Gastrointestinal haemorrhage, unspecified”, which experts considered too unspecific for gastrointestinal infections. Similarly, we excluded the presenting complaints “251—Abdominal pain” and “260—Blood in stool/melena”, as well as ICD-10 diagnoses like “R11—Nausea and vomiting” and “K92—Other diseases of digestive system” due to their relatively unspecific nature.
Selected emergency departments
Within the study period, data from 7 out of 43 emergency departments fulfilled the inclusion criteria. The departments were located in 6 out of 16 German federal states, namely Baden—Wurttemberg, Bavaria, Lower Saxony, North Rhine—Westphalia, Saxony and Schleswig—Holstein. The emergency departments varied in patient capacity, with the largest reporting an average of 674 weekly visits (range 420–829), three times more than the smallest with 216 weekly visits on average (range 115–284).
Characteristics of emergency department visits and cases of gastrointestinal infection cases
The 7 included emergency departments registered a total of n = 864,353 patient visits during the study period or 3710 visits per week on average (range 2413–4906 visits per week). Patients aged 20–39 and 60–79 years made up the largest age groups with 24% each of the visits. 51% of visits were by males. According to the syndrome definition, we classified 2.1% (n = 18,158) of visits as cases of gastrointestinal infections, ranging between 0.8% and 4.3% among emergency departments. Most gastrointestinal infection cases were either 0–19 years or 20–39 years old with 23% each. 57% of cases were female (Table 1).
Table 1.
Characteristics of emergency department visits and cases of gastrointestinal infection cases. Germany, 2019–2023.
| Variables | All visits | Gastrointestinal infection cases | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Total | 864,353 | 100 | 18,158 | 100 | |
| Sex | Female | 420,517 | 49 | 10,424 | 57 |
| Male | 443,836 | 51 | 7734 | 43 | |
| Age group | 0–19 | 116,794 | 14 | 4108 | 23 |
| 20–39 | 204,497 | 24 | 4116 | 23 | |
| 40–59 | 189,126 | 22 | 2747 | 15 | |
| 60–79 | 207,258 | 24 | 3917 | 22 | |
| 80 + | 146,678 | 17 | 3270 | 18 | |
Internal validation of the syndrome definition
Internal validity analysis revealed that cases captured solely through the two presenting complaints “254—Diarrhea” and “257—Nausea and/or vomiting” were predominantly characterized by ICD-10 codes consistent with gastrointestinal infections. These included “A09.9—Other and unspecified gastroenteritis and colitis of unspecified origin”, “A09.0—Other and unspecified gastroenteritis and colitis of infectious origin”, and “R11—Nausea and vomiting”. Conversely, we observed few ICD-10 codes inconsistent with gastrointestinal infections (Supplementary Tables 1 and 2).
External validation of the syndrome definition
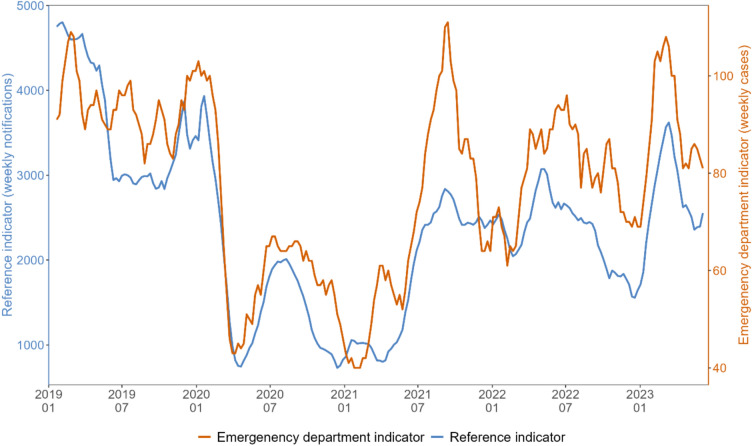
We obtained the laboratory-based reference indicator by combining statutory notifications of norovirus-gastroenteritis, rotavirus-gastroenteritis, salmonellosis and campylobacteriosis (Supplementary Fig. 1). For visual comparison of gastrointestinal infections trends over time, we plotted the emergency department indicator and the reference indicator by calendar week (Fig. 2). Both indicators exhibited similar trends. Especially, a marked decrease in the first half of 2020, followed by a slight increase over the summer 2020 and another decrease in Winter 2020/21 was apparent for emergency department and reference indicator alike. For both indicators, the number of cases rose again towards summer 2021, followed by peaks in summer 2022 and spring 2023.
Fig. 2.
Visual comparison of emergency department indicator (orange) and combined reference indicator (blue) trends as 5-week-moving-averages. Please note different scales on left and right y-axes. Germany, between week 01/2019 and up to week 23/2023.
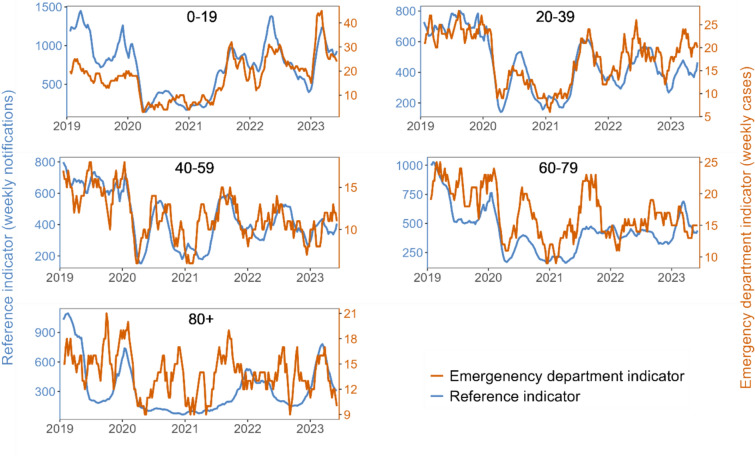
Upon stratification by age groups, younger age groups showed high coherence between the trends of both indicators. For older age groups, especially above 80 years of age, coherence between the two indicators was relatively lower than overall (Fig. 3). Cross-correlation analysis showed the highest correlation at a time lag of − 1 (in weeks), indicating that gastrointestinal infection trends in emergency departments were one week ahead of reference notification data. The overall cross-correlation coefficient at lag − 1 was 0.73 (95%-confidence interval 0.61–0.85; p < 0.001) (Supplementary Fig. 2). Cross-correlation analysis by sex and by age at lag − 1 revealed high correlation in all strata, with a lower value for patients older than 80 years of age (Table 2).
Fig. 3.
Visual comparison of emergency department indicator (orange) and reference indicator (blue) trends as 5-week-moving-averages stratified by age groups. Please note different scales on left and right y-axis. Germany, between week 01/2019 and up to week 23/2023.
Table 2.
Results of emergency department indicator and reference indicator cross-correlation analyses at lag − 1 overall, and stratified by sex and age groups. *P-values refer to the statistical significance of the cross-correlation coefficient being different from 0. Germany, 2019–2023.
| Cross-correlation coefficient | 95% confidence interval | p-value* | ||
|---|---|---|---|---|
| Overall | 0.73 | 0.61–0.85 | p < 0.001 | |
| Sex | Male | 0.67 | 0.56–0.79 | p < 0.001 |
| Female | 0.65 | 0.50–0.80 | p < 0.001 | |
| Age groups (years) | 0–19 | 0.65 | 0.53–0.77 | p < 0.001 |
| 20–39 | 0.61 | 0.47–0.74 | p < 0.001 | |
| 40–59 | 0.48 | 0.35–0.61 | p < 0.001 | |
| 60–79 | 0.48 | 0.33–0.63 | p < 0.001 | |
| 80 + | 0.22 | 0.03–0.40 | p < 0.05 | |
Discussion
We developed a syndrome definition for gastrointestinal infections in emergency departments, which combines presenting complaints (“254—Diarrhea”, “257—Nausea and/or vomiting”) and ICD-10 diagnoses (A00—A09: Intestinal infectious diseases). The observed coherent trends and high cross-correlation between our emergency department indicator and laboratory-based reference indicator validated it. Based on those results, we are confident that our syndromic surveillance will complement laboratory-based surveillance and support the detection of medium and large gastrointestinal outbreaks, and provide more detailed estimates on severe cases.
Regarding timeliness, we found the highest overall correlation at lag − 1, indicating a 1-week reporting delay for laboratory-based surveillance relative to syndromic surveillance. Compared to existing systems with time-consuming laboratory testing and reporting delays, our automated syndromic surveillance of routine data offers near real-time monitoring. This improves timely detection of disease trends and outbreaks, thereby facilitating a faster and more effective public health response.
Syndromic surveillance of gastrointestinal infections in emergency departments contributes to an all-hazards surveillance approach. Some unexpected natural or man-made health events may be missed by laboratory-based and pathogen-specific surveillance due to unavailable or delayed laboratory test results. Syndromic surveillance, on the other hand, may identify these events earlier, based on an increase of patients with respective symptoms in emergency departments. For example, the system may support the detection of (accidental or intentional) chemically-induced gastroenteritis or bioterroristic events.
By combining routine data from several sentinel emergency departments in multiple federal German states, the system supports the identification of superregional gastrointestinal disease trends and outbreaks. Moreover, our syndromic surveillance enhances real-time situational awareness during special events such as mass gatherings or sports events. For example, in 2024, syndromic surveillance was employed to monitor the 2024 UEFA European Football Championship in Germany.
Compared to laboratory-based surveillance, the system offers a reduced workload due to its automated nature. Furthermore, since it is based on routinely collected data and the existing AKTIN-infrastructure, it is comparably inexpensive. Using an established system, whose infrastructure matured and operated since 2018, ensures the stability and resilience of the gastrointestinal infection surveillance component.
Our syndrome definition combines two syndromic components. The selected ICD-10 diagnoses are more specific for gastrointestinal infections, but may be coded with a delay. Presenting complaints are coded directly upon admission and prior to detailed anamnesis. Therefore, they provide near real-time insights, but may lack diagnostic precision. In our analysis of the internal validity of presenting complaints, we observed few ICD-10 codes inconsistent with gastrointestinal infections. Integrating both data sources thus creates a suitable compromise between sensitivity and specificity to facilitate accurate and timely surveillance.
Visual trend comparison showed high coherence of trends of emergency department and reference indicators, further supported by the high cross-correlation. Observed separately, the selected reference diseases showed characteristic seasonality and peaks, albeit partially suspended during the COVID-19 pandemic (Supplementary Fig. 1). Such seasonality was not observed in either indicator, due to several diseases with shifted seasonality overlapping. This highlights that our emergency department indicator is not dominated by one disease, but rather reflects an ensemble of gastrointestinal diseases. We observed a decrease during the COVID-19 pandemic in both indicators. A similar decrease was also observed in other syndromic surveillance systems for gastrointestinal complaints at the same time, for example in the United Kingdom20.
Cross-correlation analysis corroborated the visual results with a high overall coefficient of 0.73 at lag − 1. Upon stratification by sex and age groups, we found high visual coherence in most strata, supported by high cross-correlation coefficients. Notably, cross-correlation was lower in patients over 80 years old. A possible explanation could be differences in clinical presentations of gastrointestinal infections in older patients or age-specific testing and coding practices. The number of weekly patients in this stratum was also relatively low, rendering the indicator more susceptible to fluctuations. Moreover, concurrent COVID-19 waves may have resulted in higher symptomatic gastrointestinal presentations in emergency departments, which are absent in gastrointestinal notifications. Diarrhoea has been linked to COVID-19, particularly in older patients21. Changed health-seeking behaviour may have resulted in older patients having a higher probability of admission to emergency departments due to higher risk for severe COVID-19. Potentially, this limits our ability to detect some smaller events in age-specific settings. However, syndromic surveillance does not aim to identify every small event, but rather to describe overall trends and detect events with high public health relevance.
The highest proportions of identified cases of syndromic gastrointestinal infections were among females and patients aged 39 and below. Similarly, women and younger age groups were also overrepresented in studies on gastroenteritis, e.g. from general practice in Norway22 and US emergency departments23. We identified 2.1% of all visits as cases of gastrointestinal infection, according to our syndrome definition. In comparison, a 2017 study of 5 German emergency departments reported 12% of patients presented symptoms related to the “digestive system”, based on a broader case definition and different clinical setting24. In the weekly reports of the Italian national emergency department surveillance for 2014, the percentage of patients with non-haemorrhagic gastroenteritis fluctuated between 1.3–2.3%25. Comparisons with other studies and syndromic surveillance systems remain challenging due to differences in case definitions, clinical settings and demographics.
In Germany, no other syndromic surveillance of gastrointestinal infections is currently operational. An ad-hoc surveillance for bloody diarrhoea in emergency departments during an outbreak of enterohemorrhagic E. coli was established in 2011, but later discontinued26. During a 2012 gastroenteritis outbreak associated with frozen strawberries, approximately 11,000 cases were detected via ad hoc syndromic surveillance using spreadsheets and emails27. Syndromic surveillance systems are increasingly implemented in several European countries. Since 2004 France has a surveillance system with national coverage. It includes gastroenteritis and covers ≥ 86% of emergency department visits28,29. The United Kingdom developed subnational systems, which regularly publish weekly bulletins including gastroenteritis in emergency departments30. In Italy, national and regional systems include syndromes for non- and haemorrhagic gastroenteritis25,29. Similar systems were implemented in selected hospitals in Austria and Spain12,29. Greece established a sentinel surveillance system for the 2004 Olympics31. Syndromic surveillance systems proved useful in the early identification of gastrointestinal disease trends and outbreaks, e.g. of rotavirus-gastroenteritis32 and enterohemorrhagic E. coli26 and for assessing potential health impacts of mass gatherings31,33.
Our findings should be interpreted considering some limitations. As a sentinel surveillance system, the AKTIN registry is neither geographically nor demographically representative for the German population. Consequently, we cannot estimate the prevalence of gastrointestinal infections in the general population. Our syndromic surveillance allows to monitor trends among patients presenting to emergency departments, a specific subset with distinct characteristics. Emergency department attendance and care-seeking behaviour may also vary systematically by gender, age, or other socio-demographic factors. Furthermore, data collected through routine hospital documentation is primarily intended for clinical use rather than disease surveillance. The quality of documentation may vary between emergency departments, resulting in possible misclassification bias. Particularly, the coding of diagnoses according to ICD-10 may differ due to (hospital-specific) administrative and budgetary coding regulations. Since syndromic surveillance is not based on laboratory-confirmed diagnoses but on less specific clinical symptoms, cases may be misclassified, possibly resulting in over- or underestimation of case numbers. However, since syndromic surveillance aims at identifying overall trends rather than identifying single cases, it may tolerate some deviation of the estimate. All visit data is anonymised, so there could be multiple visits by the same patient, possibly resulting in excess cases. Nevertheless, as this imprecision effect remains over time, the expected bias is likewise relatively constant over time. Additionally, delays in data entry and processing—particularly for the coding of ICD-10 diagnoses—may limit the timeliness of syndromic surveillance, although the use of presenting complaints in the syndrome definition partly mitigates this issue. Lastly, our analysis was complicated by the COVID-19 pandemic coinciding with our study period. Through multiple factors, foremost changes in health-seeking behaviour, the pandemic may have shifted the composition and numbers of patients attending emergency departments in general and cases of gastrointestinal infections specifically34,35.
In the future, syndromic surveillance of gastrointestinal infections may be expanded. For example, the system could be adapted for the early identification of relevant severe gastrointestinal conditions, such as “bloody diarrhoea” or “haemolytic uraemic syndrome”. More variables could be added to further refine the syndrome definition, such as body temperature or patient isolation. Signal algorithms could analyse data to trigger automated alerts. As of January 2022, the ICD-11 version officially replaces its ICD-10 predecessor. ICD-11 codes are not yet used by AKTIN emergency departments. Following a transitional period and their implementation, the syndrome definition may need to be adapted accordingly. The ICD-11 revisions may prove useful, as the new group “1A0—1A40 Gastroenteritis or colitis of infectious origin” combines many relevant diagnoses36. Our analysis was based on retrospective data, but eventually the performance of the system should be evaluated prospectively.
We conclude that our newly developed syndrome definition for gastrointestinal infections in emergency departments is valid and ready for implementation in routine syndromic surveillance. It was implemented in the Robert Koch Institute’s automated emergency department surveillance reporting in December 2023. Our novel automated surveillance offers advantages regarding timeliness and reduced workload compared to laboratory-based surveillance. It adds public health value by completing a real-time image of the situation in emergency departments, helps to monitor gastrointestinal infection trends and informs public health measures. The timely surveillance of gastrointestinal infections in emergency departments facilitates outbreak detection and response. In summary, syndromic surveillance in emergency departments optimally complements statutory laboratory-based surveillance in Germany.
Supplementary Information
Acknowledgements
The authors would like to express their gratitude to the authors of the R packages tidyverse, lubridate, ISOweek, Readxl, naniar, flextable, gtsummary, stringr, tsibble, slider, ggh4x, ggpubr and tseries. Moreover, the authors would like to thank the Postgraduate Training for Applied Epidemiology (PAE) and the European Programme for Intervention Epidemiology Training (EPIET) for enabling this study, particularly Sofie Gillesberg Raiser, Dr. Jan Walter and Dr. Raskit Lachmann.
Author contributions
J.H.J.B., T.S.B. and M.S. conceptualised the project. M.S. supervised the project. J.H.J.B., M.S. and H.W. developed the syndrome definition. J.H.J.B. devised the study protocol, researched literature, performed data analysis, interpreted results, created visuals, and wrote the manuscript. M.S., H.W., T.S.B., provided feedback on the study protocol, methods, data analysis, and interpretation. A.D. assisted with the statistical analysis and K.H. helped with the literature research. S.D., B.E., R.G., C.G., K.H., E.H., A.H., H.H., C.K., F.R., J.R., and T.S. gave clinical feedback on the syndrome definition. AKTIN Research Group provided the emergency department surveillance data used in this study. All authors critically reviewed the manuscript and approved the final version.
Funding
Open Access funding enabled and organized by Projekt DEAL. The Robert Koch Institute is an Institute within the portfolio of the German Federal Ministry of Health. The AKTIN emergency department registry is funded by the German Federal Ministry of Education and Research. This publication was partially funded by the German Federal Ministry of Education and Research (BMBF) Network of University Medicine 2.0: "NUM 2.0", Grant No. 01KX2121, Project: AKTIN-EZV, AKTIN@NUM.
Data availability
The data that support the findings of this study are available from the AKTIN emergency department registry but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request to office@aktin.org and with permission of the AKTIN emergency department registry.
Declarations
Ethics approval
The AKTIN emergency department registry received ethics approval from the Ethics Committee of the medical facility of the Otto von Guericke University in Magdeburg (ethics approval: 160/15 and 52/21). Primary data is stored (pseudonymized and decentralized) in local data warehouses at each hospital. AKTIN provides anonymized data to researchers after approval from their Data Use and Access Committee. Therefore, an additional ethics approval for this specific study is not required. Moreover, the use of routine emergency department data for surveillance was approved by the data protection officer at the Robert Koch Institute (BDS/ISB, 09-01-2019).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Jonathan Hans Josef Baum, Email: baumj@rki.de.
AKTIN Research Group:
Markus Baacke, Jaqueline Bauer, Michael Bernhard, Jonas Bienzeisler, Sabine Blaschke, Jörg Brokmann, Volker Burst, Hans-Jörg Busch, Harald Dormann, Christoph Duesberg, Saskia Ehrentreich, André Gries, Thomas Händl, Eric Handmann, Felix Hans, Frank Hanses, Thomas Henke, Matthias Klein, Tobias Hofmann, Marina Karg, Jan Kleinekorth, Alexander Kombeiz, Bernhard Kumle, Philipp Kümpers, Christoph Lewejohann, Alexander Dinse-Lambracht, Benjamin Lucas, Carsten Mach, Raphael W. Majeed, Jürgen Neubauer, Ronny Otto, Thomas Peschel, Norbert Pfeufer, Rainer Röhrig, Wiebke Schirrmeister, Domagoj Schunk, Wolfgang Stahl, Hartmut Stefani, Lucas Triefenbach, Bernd Uirich, Felix Walcher, Markus Wehler, Hardy Wenderoth, Sebastian Wolfrum, Christian Wrede, and Markus Zimmermann
References
- 1.National Cancer Institute. NCI’s Dictionary of Cancer Terms. n.d. [cited 2023 Feb 02]. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/gastroenteritis.
- 2.World Health Organization. Global Health Estimates 2019: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019. 2020 [cited 2022 Mar 02]. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates.
- 3.Wilking, H. et al. Acute gastrointestinal illness in adults in Germany: a population-based telephone survey. Epidemiol. Infect.141(11), 2365–2375 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robert Koch-Institut. Infektionsepidemiologisches Jahrbuch meldepflichtiger Krankheiten für 2019. Berlin 2020.
- 5.Robert Koch-Institut. Falldefinitionen des Robert Koch-Instituts zur Übermittlung von Erkrankungs-oder Todesfällen und Nachweisen von Krankheitserregern gemäß § 11 Abs. 2 des Gesetzes zur Verhütung und Bekämpfung von Infektionskrankheiten beim Menschen (Infektionsschutzgesetz-IfSG). Berlin; 2019.
- 6.Triple S Project. Assessment of syndromic surveillance in Europe. Lancet. 378(9806), 1833–1834 (2011). [DOI] [PubMed]
- 7.AKTIN-Notaufnahmeregister. Aktionsbündnis zur Verbesserung der Kommunikations-und Informationstechnik in der Intensiv-und Notfallmedizin. 2022 [cited 2023 Sep 01]. https://www.aktin.org/de-de/.
- 8.Brammen, D., Greiner, F., Kulla, M., Otto, R., Schirrmeister, W., Thun, S., et al. AKTIN—The German Emergency Department Data Registry—real-time data from emergency medicine : Implementation and first results from 15 emergency departments with focus on Federal Joint Committee’s guidelines on acuity assessment. Med. Klin. Intensivmed Notfmed. 117(1)(2193–6226 (Electronic)), 24–33 (2020). [DOI] [PMC free article] [PubMed]
- 9.Robert Koch-Institut. Routinedaten aus dem Gesundheitswesen in Echtzeit (SUMO). [cited 2023 Sep 01]. www.rki.de/sumo.
- 10.Boender, T. S., Cai, W., Schranz, M., Kocher, T., Wagner, B., Ullrich, A., et al. Using routine emergency department data for syndromic surveillance of acute respiratory illness, Germany, week 10 2017 until week 10 2021. Euro Surveill. 27(27) (2022). [DOI] [PMC free article] [PubMed]
- 11.Schranz, M. Syndromic surveillance using emergency department data for the monitoring of unspecific acute gastrointestinal infections. Master thesis Public Health. (Charité-Universitätsmedizin, 2019).
- 12.Ziemann, A. et al. A concept for routine emergency-care data-based syndromic surveillance in Europe. Epidemiol. Infect.142(11), 2433–2446 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chapman, W. W. et al. Developing syndrome definitions based on consensus and current use. J. Am. Med. Inform. Assoc.17(5), 595–601 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robert Koch Institute, Brammen D, Heitmann K, Grabenhenrich L, Schranz M, Kocher T, et al. NoKeda-Notaufnahme-Kerndatenmodell für Public-Health-Surveillance und Versorgungsforschung 2020 [cited 2023 Sep 01]. https://art-decor.org/art-decor/decor-project-nokeda.
- 15.Brammen, D. et al. Lessons learned in applying the International Society for Pharmacoeconomics and Outcomes Research methodology to translating Canadian Emergency Department Information System Presenting Complaints List into German. Eur. J. Emerg. Med.25(4), 295–299 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) im Auftrag des Bundesministeriums für Gesundheit (BMG) unter Beteiligung der Arbeitsgruppe ICD des Kuratoriums für Fragen der Klassifikation im Gesundheitswesen. ICD-10-GM Version 2021, Systematisches Verzeichnis, Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme, 10. Revision. 2020.
- 17.Kunsch, H. R. The jackknife and the bootstrap for general stationary observations. Ann. Stat.17(3), 1217–1241 (1989). [Google Scholar]
- 18.R Core Team. R: A Language and Environment for Statistical Computing (2022).
- 19.R Studio Team. RStudio: Integrated Development Environment for R (2020).
- 20.Love, N. K. et al. Impact of the COVID-19 pandemic on gastrointestinal infection trends in England, February-July 2020. BMJ Open12(3), e050469 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Comoglu, Ş et al. Evaluation of diarrhea in patients with COVID-19. Dig. Dis.39(6), 622–625 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Emberland, K. E., Wensaas, K. A., Litleskare, S. & Rortveit, G. Consultations for gastroenteritis in general practice and out-of-hours services in Norway 2006–15. Fam. Pract.36(5), 614–620 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myer, P. A. et al. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am. J. Gastroenterol.108(9), 1496–1507 (2013). [DOI] [PubMed] [Google Scholar]
- 24.Scherer, M., Lühmann, D., Kazek, A., Hansen, H. & Schäfer, I. Patients attending emergency departments. Dtsch Arztebl Int.114(39), 645–652 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Istituto Superiore di Sanità. Sistema di sorveglianza sindromica degli accessi ai Pronto soccorso. 2015 [cited 2023 Sep 01]. https://www.epicentro.iss.it/focus/sorveglianza/ProntoSoccorso.
- 26.Wadl, M., Rieck, T., Nachtnebel, M., Greutélaers, B., an der Heiden, M., Altmann, D., et al. Enhanced surveillance during a large outbreak of bloody diarrhoea and haemolytic uraemic syndrome caused by Shiga toxin/verotoxin-producing Escherichia coli in Germany, May to June 2011. Euro Surveill. 16(24) (2011). [DOI] [PubMed]
- 27.Bernard, H. et al. Large multistate outbreak of norovirus gastroenteritis associated with frozen strawberries, Germany, 2012. Euro Surveill.19(8), 20719 (2014). [DOI] [PubMed] [Google Scholar]
- 28.Nadège Caillère, A. F., Henry, V., Vilain, P., Mathieu, A., Maire, B., Viudès, G., Chansard, P., Merlen, R., Pavillon, G., Caserio-Schönemann, C. Le système français de Surveillance sanitaire des urgences et des décès (SurSaUD®). In: Institut de veille sanitaire, editor. Saint-Maurice2012, 1–12.
- 29.Ziemann, A., Fouillet, A., Brand, H. & Krafft, T. Success factors of european syndromic surveillance systems: A worked example of applying qualitative comparative analysis. PLoS ONE11(5), e0155535 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.UK Health Security Agency. Emergency Department Syndromic Surveillance System (EDSSS): weekly bulletins. 2023 [cited 2023 Aug 18]. https://www.gov.uk/government/collections/syndromic-surveillance-systems-and-analyses#emergency-department-syndromic-surveillance-system.
- 31.Dafni, U. G. et al. Algorithm for statistical detection of peaks–syndromic surveillance system for the Athens 2004 Olympic Games. MMWR Suppl.53, 86–94 (2004). [PubMed] [Google Scholar]
- 32.Caillère, N. et al. A major outbreak of gastroenteritis in Réunion Island in 2012: first identification of G12 rotavirus on the Island. Euro Surveill.18(19), 20476 (2013). [PubMed] [Google Scholar]
- 33.Elliot, A. J. et al. Establishing an emergency department syndromic surveillance system to support the London 2012 Olympic and Paralympic Games. Emerg. Med. J.29(12), 954–960 (2012). [DOI] [PubMed] [Google Scholar]
- 34.Ullrich, A. et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during week 1–2016 - week 32–2020. Lancet Reg. Health Eur.6, 100103 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schranz, M. et al. Changes in emergency department utilisation in Germany before and during different phases of the COVID-19 pandemic, using data from a national surveillance system up to June 2021. BMC Public Health23(1), 799 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. International Classification of Diseases Eleventh Revision (ICD-11) (2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the AKTIN emergency department registry but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request to office@aktin.org and with permission of the AKTIN emergency department registry.