Abstract
Mycobacterium tuberculosis and M. bovis infect animals and humans. Their epidemiologies in developed and developing countries differ, owing to differences in the implementation of preventive measures (World Health Organization, 1999). Identification and differentiation of these closely related mycobacterial species would help to determine the source, reservoirs of infection, and disease burden due to diverse mycobacterial pathogens. The utility of the hupB gene (Rv2986c in M. tuberculosis, or Mb3010c in M. bovis) to differentiate M. tuberculosis and M. bovis was evaluated by a PCR-restriction fragment length polymorphism (RFLP) assay with 56 characterized bovine isolates (S. Prabhakar et al., J. Clin. Microbiol. 42:2724-2732, 2004). The degree of concordance between the PCR-RFLP assay and the microbiological characterization was 99.0% (P < 0.001). A nested PCR (N-PCR) assay was developed, replacing the PCR-RFLP assay for direct detection of M. tuberculosis and M. bovis in bovine samples. The N-PCR products of M. tuberculosis and M. bovis corresponded to 116 and 89 bp, respectively. The detection limit of mycobacterial DNA by N-PCR was 50 fg, equivalent to five tubercle bacilli. M. tuberculosis and/or M. bovis was detected in 55.5% (105/189) of the samples by N-PCR, compared to 9.4% (18/189) by culture. The sensitivities of N-PCR and culture were 97.3 and 29.7, respectively, and their specificities were 22.2 and 77.7%, respectively. The percentages of animals or samples identified as infected with M. tuberculosis or M. bovis by N-PCR and culture reflected the clinical categorizations of the cattle (P of <0.05 to <0.01). Mixed infection by N-PCR was detected in 22 animals, whereas by culture mixed infection was detected in 1 animal.
Mycobacterium bovis, the causative agent of bovine tuberculosis, has no known geographical boundaries. M. bovis infection occurs in diverse groups of animals, which include farm animals of economic importance, wildlife, and humans (1, 16, 17, 31). Despite these ominous features of M. bovis, to date there have been only projected global estimates of the disease burden. There has been no international effort to determine the actual disease burden, owing to the nonavailability of a reliable user-friendly technology for early detection of M. bovis in clinical samples. Bovine tuberculosis has been on the increase in developed countries and continues to occur in developing countries (6, 14, 16). In Africa, approximately 85% of cattle and 82% of the human population live in areas where the disease is prevalent (6, 26). There are limited reports from India (24, 27, 38, 40) and from underdeveloped countries (6, 16) relating to the prevalence of and infection with M. bovis in cattle. Detection of M. bovis in bovine samples has become necessary, as infected animals are potentially capable of infecting humans (zoonotic tuberculosis) (6). Besides M. bovis, transmission of M. tuberculosis from infected humans to animals and back has been reported (reverse zoonosis) (10, 12, 41). Hence, M. bovis and M. tuberculosis pose a potential health hazard to both animals and humans (1, 15, 43).
The identification of the closely related members of the Mycobacterium tuberculosis complex (MTC) has remained a challenging task in diagnostic laboratories (7, 30, 44). MTC includes a variety of closely related mycobacteria, namely, M. tuberculosis, M. bovis, M. canetti, M. africanum, and M. microti. A panel of classical tests based on microbiological features such as growth rate and phenotypic and biochemical characteristics has conventionally been utilized to distinguish members of MTC (30). However, these tests are slow, cumbersome, unreliable, and time-consuming. The high degree of variability among these tests warrants the development of molecular biological tools for identification of MTC members. In this regard, multiple gene targets have been used to date to detect and differentiate genetically identical species, such as M. tuberculosis and M. bovis. The gene targets include pncA (2, 29, 36), gyrB (5), oxyR (42), and katG (19). Huard et al. (21) and Richter et al. (33) have targeted multiple loci and genes to differentiate M. tuberculosis from M. bovis. However, to date no single accepted protocol(s) that can unambiguously differentiate all members of the MTC is available. Identification of the etiological agent belonging to MTC is important for determination of the origin and reservoirs of infection and also for implementation of appropriate public health measures.
Our laboratory earlier described a PCR-restriction fragment length polymorphism (RFLP) method utilizing the hupB gene, encoding a histone-like protein of M. tuberculosis, as a target for detection and identification of M. tuberculosis and M. bovis from other members of the MTC and nontuberculous mycobacterial and nonmycobacterial species (32). The study revealed a 27-bp difference in the C-terminal parts of the hupB genes of M. tuberculosis and M. bovis. The present study describes the reliability of the PCR-RFLP assay in the identification of mycobacterial isolates derived from cattle and the utility of the hupB gene-based nested PCR assay (N-PCR) for direct detection of M. tuberculosis and/or M. bovis in bovine samples.
MATERIALS AND METHODS
Study design.
Samples (n = 753) collected from 144 heads of cattle housed in military farms under the jurisdiction of the Central Military Veterinary Laboratory (CMVL), Meerut, India, were used in the study. As a first step in the study, 56 randomly selected isolates derived from 544 samples of 80 animals were examined for comparison of PCR-RFLP assay-based identification of M. tuberculosis and M. bovis, as described by Prabhakar et al. (32), with conventionally identified and speciated mycobacteria. In the second part of the study, 189 samples obtained from 64 animals were screened by N-PCR for direct detection of M. tuberculosis and M. bovis. N-PCR results have been correlated with standard techniques of identification and speciation of mycobacteria.
Animals.
Clinical examination of the cattle was carried out at the Central Military Veterinary Laboratory, Meerut. The clinical signs utilized were symptoms of lymphadenopathies, loss of body weight and/or production loss, intermittent pyrexia, udder infection, and dry cough. A single intradermal tuberculin test was carried out. One hundred microliters of bovine tuberculin (2,000 U/animal), obtained from the Indian Veterinary Research Institute, Izatnagar, India (1 mg protein/ml), was injected into the skin of the cervical area. Seventy-two hours later, the injected site was examined, and the extent of induration was measured. With an induration of 5 mm or more, the animal was considered to be a reactor. Based on their in vivo tuberculin reactivities and clinical criteria, the cattle were divided into five groups: group A, tuberculin positive with signs of tuberculosis; group B, tuberculin positive and apparently healthy; group C, tuberculin negative with signs of tuberculosis; group D, tuberculin negative and apparently healthy; and group E, ailing from gastroenteritis and pyrexia of unknown origin and clinically considered to be infected with nonmycobacterial infection. C sc tuberculin testing was not done with group E. Seven samples were collected from each animal, namely, fine needle aspirate (FNA) from the prescapular lymph node (PSLN), citrated blood, milk, pharyngeal swab, urine, rectal pinch, and fecal sample. All samples were divided into two aliquots. The aliquoted samples were transported within 48 h of collection on wet ice to the laboratories of H. K. Prasad and V. M. Katoch.
Identification of mycobacteria isolated from bovine samples.
All samples were processed for isolation and cultivation of mycobacteria from bovine samples in the laboratory of V. M. Katoch by using the standard modified Petroff method. Lowenstein-Jensen media with or without pyruvate was used for primary isolation. Species level identification of isolates was done by standard biochemical tests (niacin production, nitrate reduction, catalase and aryl sulfatase activity, Tween hydrolysis, thiopen-2-carboxylic acid hydrazide sensitivity, etc.) as recommended by the Centers for Disease Control and Prevention (CDC), Atlanta, Ga., with appropriate controls (45).
Processing of samples for isolation of template DNA for PCR.
After initial screening of the seven samples by culture, PSLN, citrated blood, and milk samples were found to be suitable for isolation of M. tuberculosis and M. bovis. These samples were processed for target DNA isolation in the laboratory of H. K. Prasad by using the method as described by Chakravorty and Tyagi (3). The specific details for each sample are as follows.
(i) The FNA of the PSLN was mixed with 1 ml of sterile water and centrifuged at 12,000 × g for 15 min. The pellet was resuspended in inhibitory removing solution (IRS), pH 7.4, consisting of 25 M guanidinium isothiocyanate, 0.025 M EDTA, 0.05 M Tris, 0.5% sarcosyl, and 0.186 M β-mercaptoethanol (3), and centrifuged. The pellet was washed in sterile water, suspended in 100 μl of lysis buffer (10% Chelex-100 suspension, 0.3% Tween 20, and 0.03% Triton X-100), heated in a dry bath at 90°C for 40 min, and centrifuged at 10,000 × g for 10 min. The supernatant was used as target DNA.
(ii) Citrated blood was vortexed with ice-cold red blood cell (RBC) lysis buffer (0.83% NH4Cl, 0.1% KHCO3, 0.5 M EDTA, pH 8.0) and incubated for 10 min. The lysed RBC was separated by centrifugation at 12,000 × g for 20 min. The supernatant was discarded. The pellet was resuspended in RBC lysis buffer, incubated, and centrifuged as described above. The pellet was resuspended in IRS and processed as mentioned for PSLN.
(iii) Milk samples were centrifuged at 12,000 × g for 20 min. A sterile cotton swab was used to remove the fat layer, and the supernatant was discarded. The pellet was resuspended in IRS and processed as mentioned for PSLN.
DNA extraction from bovine mycobacterial isolates.
A loop full of isolate was taken from the Lowenstein-Jensen slant and transferred to the 1.5-ml tube with 200 μl of 0.1% Triton X-100. The resuspended bacteria was heated in a dry bath at 90°C for 40 min and centrifuged at 10,000 × g for 10 min. The supernatant was used as target DNA.
PCR-RFLP for hupB gene.
The PCR-RFLP assay for the hupB gene (All India Institute of Medical Sciences, international patent application no. PCT/IN03/00302, 1 July 2004, L. S. Davar and Co., Calcutta, India) was performed as described earlier (32). Briefly, the primers N (5′-GAGGGTTGGGATGAACAAAGCAG-3′) and S (5′-TATCCGTGTGTCTTGACCTATTTG-3′) were used to amplify the hupB gene (N-S PCR) (Fig. 1A) from the DNA extracted from various isolates. The amplified sequences were digested by the HpaII restriction enzyme. The products were analyzed on a 10% nondenaturing polyacrylamide gel. The gel was stained with ethidium bromide, and DNA fragments were visualized under UV light.
FIG. 1.
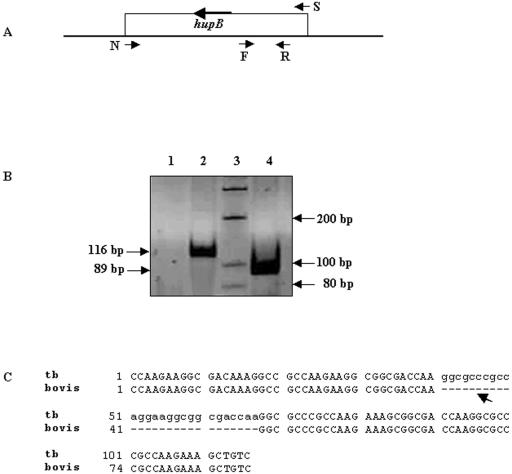
Nested PCR to amplify C-terminal part of hupB gene. (A) The positions of the primers in the hupB (Rv2986c in M. tuberculosis, or Mb3010c in M. bovis) sequence that were used to obtain the nested PCR products are depicted. Primer pair N and S was specific for the hupB gene; internal primer pair F and R was specific for the C-terminal part of the gene. The F and R primers were used to reamplify the amplified product generated by the N and S primers (N-PCR). (B) The ethidium bromide-stained amplification products of M. tuberculosis and M. bovis generated by using F and R primers were electrophoresed on nondenaturing 10% polyacrylamide gels. The 116- and 89-bp products obtained for M. tuberculosis and M. bovis, respectively, are indicated. Lanes: 1, negative control; 2, M. tuberculosis (M. tuberculosis DNA from TB research material; NIAID, NIH); 3, 100-bp molecular size marker; 4, M. bovis (AN5 strain; JALMA, Agra, India). (C) Sequences of F and R amplified PCR products of M. tuberculosis (tb) (116 bp) and M. bovis (89 bp) were aligned using ClustalW software to depict the 27-bp deletion in M. bovis, indicated by the arrow.
N-PCR for C-terminal portion of hupB DNA target.
The N-PCR for the C-terminal portion of the hupB gene (international patent application no. PCT/IN03/00302) was carried out using 4 μl of the amplified product of the N-S PCR as the template and primer pair F (5′-CCAAGAAGGCGACAAAGG-3′) and R (5′-GACAGCTTTCTTGGCGGG-3′) (Fig. 1A). Each reaction (40 μl) contained 1.25 mM MgCl2, 200 μM deoxynucleoside triphosphates, 0.5 μM of F and R primers, 10 mM Tris-HCl (pH 8.8), 50 mM KCl, 0.08% Nonidet P-40, and 1.0 U of Taq DNA polymerase (MBI Fermentas). The reaction mixture was subjected to an initial denaturation at 94°C for 10 min and 35 cycles each of 1.0 min at 94°C and annealing and extension at 59°C for 30 s, followed by a final extension at 72°C for 7.0 min. The products were analyzed on a 10% nondenaturing polyacrylamide gel and stained with ethidium bromide. The expected sizes of the amplicons for M. tuberculosis and M. bovis were 116 and 89 bp, respectively.
Sensitivities of N-S and N-PCR assays.
The sensitivities of the N-S and N-PCR assays were deciphered by using different concentrations of M. tuberculosis DNA (tuberculosis [TB] research material; NIH) ranging from 10 ng (∼106 bacilli) to 10 fg (∼1 bacillus). The expected sizes of the amplicons for the N-S and N-PCR assays were 645 and 116 bp, respectively.
Statistical analysis.
The results of the PCR assay were compared with those of culture by using agreement and kappa tests. The correlation of detection of M. tuberculosis and/or M. bovis in bovine samples with clinical categorization and diagnosis of the cattle included in the study was assessed by a trend chi-square test. The positivity of samples was also assessed by a chi-square test. All statistical analysis was done using the statistical software STATA 7.0 (STATA Corporation, College Station, Texas).
RESULTS
Correlation of identification of M. tuberculosis and M. bovis by PCR-RFLP assay and standard culture techniques.
The utility of the PCR-RFLP assay to differentiate and identify M. tuberculosis and M. bovis (32) was independently confirmed in the laboratory of V. M. Katoch (Table 1). Fifty-six isolates derived from 544 samples identified by standard criteria were used in the assay. Thirty-three isolates were identified as M. bovis, 7 as M. tuberculosis, and 15 as nontuberculous mycobacteria. One isolate identified as M. bovis failed to be identified by the PCR-RFLP assay. The degree of correlation between the two techniques was determined to be 99.0% (κ = 0.96 ± 0.11; P < 0.001).
TABLE 1.
Correlation of gold standard identification of mycobacterial isolates derived from bovine samples with PCR-RFLP assay
Among the assortment of samples screened by culture, PSLN, milk, and blood showed the highest isolation rates. Hence, pharyngeal swab, rectal pinch, urine, and fecal samples were not used subsequently.
N-PCR for detection and identification of M. tuberculosis and M. bovis.
In order to establish a routine PCR-based assay for detection and identification of M. tuberculosis and M. bovis in clinical samples not requiring RFLP analysis, a nested PCR assay was developed. The difference in the C-terminal parts of the hupB genes of M. tuberculosis (Rv2986c) and M. bovis (Mb3010c) was exploited. The ethidium bromide-stained amplified products of M. tuberculosis and M. bovis generated by the N-PCR are depicted in Fig. 1B. The 116- and 89-bp products obtained for M. tuberculosis and M. bovis, respectively, are indicated. Figure 1C shows the alignment of the N-PCR products of M. tuberculosis and M. bovis, indicating the 27-bp difference.
Sensitivity of the N-PCR assay.
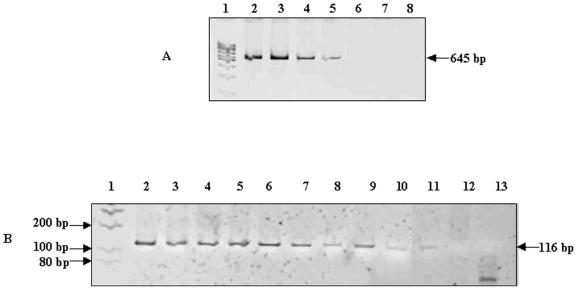
The limit of sensitivity of the N-PCR assay to detect M. tuberculosis DNA was determined by using various concentrations of DNA. The products of the N-S PCR and N-PCR are shown in Fig. 2A and B, respectively. The amplified N-S PCR product could be detected up to a 0.1-ng DNA concentration, equivalent to 104 bacilli (Fig. 2A, lanes 2 to 5). However, in the case of N-PCR, the amplified product could be visualized in the PCR mixture initiated with DNA concentrations ranging from 10 ng to 50 fg, the latter of which is equivalent to 5 tubercle bacilli (Fig. 2B, lanes 2 to 11). The sensitivity of the N-PCR assay was determined to be 2,000 times more than that of the N-S PCR assay. The sensitivity of the N-PCR for detection of M. bovis DNA was found to be identical to the sensitivity of the N-PCR for detection of M. tuberculosis DNA (data not shown).
FIG. 2.
Sensitivity of N-PCR assay. (A) The ethidium bromide-stained amplification products of the target hupB gene of M. tuberculosis generated using primers N and S were electrophoresed on nondenaturing 10% polyacrylamide gels. The 645-bp product is indicated. The M. tuberculosis DNA used was obtained from TB research materials, NIAID, NIH. Lanes: 1, 100-bp molecular size marker; 2, 10 ng DNA (106 bacilli); 3, 1 ng DNA (105 bacilli); 4, 0.5 ng DNA (5 × 104 bacilli); 5, 0.1 ng DNA (104 bacilli); 6, 10 pg DNA (103 bacilli); 7, 1 pg DNA (100 bacilli); 8, 0.5 pg DNA (50 bacilli). (B) The ethidium bromide-stained amplification products of the C terminal of the hupB gene of M. tuberculosis generated using F and R primers in N-PCR were electrophoresed on nondenaturing 10% polyacrylamide gels. N and S amplified PCR products (4 μl) were used as a template. Lanes: 1 to 8, same as described for panel A; 9, 0.25 pg DNA (25 bacilli); 10, 100 fg DNA (10 bacilli); 11, 50 fg DNA (5 bacilli); 12, 10 fg DNA (1 bacillus); 13, negative control.
N-PCR for direct detection of M. tuberculosis and/or M. bovis in bovine samples.
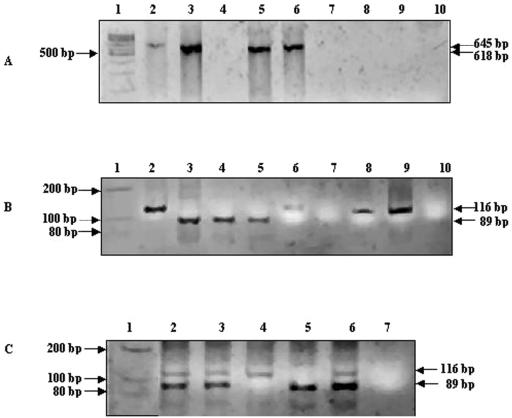
DNA extracted from bovine samples, namely, milk, blood, and FNA of PSLN, were used in an N-PCR assay. The amplified products obtained with representative bovine samples are shown in Fig. 3. Figure 3A depicts the N-S PCR products for bovine samples. PCR product sizes of 618 and 645 bp specific for M. bovis and M. tuberculosis, respectively, are seen in lanes 5 and 6, derived from milk and blood samples, respectively (Fig. 3A) (32). Figure 3B depicts the N-PCR products for the bovine samples. The molecular sizes and extents of migration of the N-PCR products generated in the samples were compared with those of the positive controls, namely, M. tuberculosis (TB research material; NIH) (Fig. 3B, lane 2) and M. bovis (AN5; JALMA, Agra, India) (Fig. 3B, lane 3). N-PCR products were seen for all samples except that in lane 7 (Fig. 3B). PCR products of milk samples loaded in lanes 4 and 5 (Fig. 3B) were identified to be M. bovis. Since the N-PCR products derived from blood (lane 6) and lymph node aspirates (lanes 8 and 9) matched with the N-PCR product of M. tuberculosis (lane 2), they were predicted to be M. tuberculosis.
FIG. 3.
N-PCR for detecting and differentiating M. tuberculosis and M. bovis in samples of bovine origin. (A) The ethidium bromide-stained amplification products of the hupB gene generated using primers N and S were electrophoresed on nondenaturing 10% polyacrylamide gels. The 645- and 618-bp products corresponding to M. tuberculosis and M. bovis, respectively, are indicated. Lanes: 1, 100-bp molecular size marker; 2, M. tuberculosis positive control; 3, M. bovis positive control; 4, milk serial no. 103; 5, milk 104; 6, blood 123; 7, blood 127; 8, PSLN 90; 9, PSLN 95; 10, negative control. (B) The ethidium bromide-stained amplification products of the C terminal of the hupB gene of M. tuberculosis generated using F and R primers in the N-PCR assay were electrophoresed on nondenaturing 10% polyacrylamide gels. N and S amplified PCR products (4 μl) were used as a template. Lanes 1 to 10 are the same as described for panel A. (C) N-PCR of bovine samples depicting mixed infection. Lanes: 1, 100-bp molecular size marker; 2, PSLN serial no. 104; 3, milk 119; 4, M. tuberculosis positive control; 5, M. bovis positive control; 6, dual positive control; 7, negative control.
Speciation of pathogenic mycobacteria in bovine samples.
Speciation of the pathogenic mycobacteria was done for 87.6% (99/113) of the samples by N-PCR (Table 2). For six samples, which were positive for the MTC, speciation could not be established by N-PCR. Neither by N-PCR nor by standard culture techniques was M. tuberculosis or M. bovis found to predominate in the samples investigated. M. bovis was detected in 40.7% of the samples and M. tuberculosis was detected in 37.1% of the samples by N-PCR (Table 2).
TABLE 2.
Detection of pathogenic mycobacteria in cattle-derived samples
| Sample type (total no. of samples positive by N-PCR and culture) | No. (%) of bovine samples positive for pathogenic mycobacteria byd:
|
|||||||
|---|---|---|---|---|---|---|---|---|
| N-PCR
|
Culturea
|
|||||||
| M. tuberculosis | M. bovis | M. tuberculosis and M. bovisb | Total | Not donec | M. tuberculosis | M. bovis | Total | |
| PSLN (35) | 10 | 15 | 3 | 28 (80.0) | 4 | 2 | 2 | 4 (11.4) |
| Blood (30) | 12 | 12 | 1 | 25 (83.3) | 1 | 5 | 2 | 7 (23.3) |
| Milk (48) | 20 | 19 | 7 | 46 (95.8) | 1 | 3 | 4 | 7 (14.2) |
| Total (113) | 42 (37.1) | 46 (40.7) | 11 (9.7) | 99 (87.6) | 6 | 10 (8.8) | 8 (7.1) | 18 (15.7) |
Identification of cultivated mycobacterial isolates by standard tests (CDC, Atlanta, Ga.).
M. tuberculosis and M. bovis detected in samples derived from a single animal/in an individual sample.
Speciation could not be established by N-PCR but samples were positive for MTC.
M. tuberculosis versus M. bovis results were not significant. Results with milk versus PSLN versus blood had a P value of <0.001.
Mycobacteria were isolated and identified by standard culture techniques in 33 samples of the 189 examined. Ten samples (8.8%) were diagnosed as infected with M. tuberculosis and eight (7.1%) with M. bovis (Table 2). In the remaining 15 samples, nontuberculous rapid-growing mycobacteria, such as M. scrofulaceum, M. kansasii, M. flavescens, M. smegmatis, M. fortuitum, M. gastri, M. phlei, M. vaccae, and M. chelonae, were identified. Among the samples investigated, milk was found to be predominantly positive for M. tuberculosis and/or M. bovis by N-PCR (46/48 samples; P < 0.001) and blood predominantly positive by culture (7/30 samples).
Mixed infection with M. tuberculosis and M. bovis in bovine samples.
A limited number of samples scrutinized by the N-PCR assay showed evidence of mixed infection by M. tuberculosis and M. bovis in individual animals. Precautions were taken, keeping in mind the possibility of laboratory-introduced contamination during processing of samples. Each sample was processed individually within a biosafety cabinet (type III), minimizing the possible introduction of contaminants from the environment by aerosols or another infected sample. Further, the PCR has always been carried out with appropriate controls, which include positive controls for M. tuberculosis and M. bovis and a negative control (Fig. 3C). The routine inclusion of a negative control in the assay ruled out the occurrence of false-positive PCR caused by contamination. Further, the organizational setup for the PCR assay was such that the sites for processing of samples for DNA extraction, setting up of the PCR, addition of extracted DNA, and screening of gels and capturing of the images were in physically separated rooms. To further rule out the possibility of false-negative results in the study due to the presence of PCR inhibitors in DNA extracts of samples, spiked controls were used. The generation of the expected PCR product in the spiked controls showed the absence of sample-derived PCR inhibitors (data not shown).
Representative N-PCR products from samples, namely, milk and lymph node aspirates, exhibiting mixed infection are depicted in Fig. 3C (lanes 2 and 3). In each of the samples, N-PCR products corresponding in molecular weight to that of the positive control, namely, M. tuberculosis (lane 4) or M. bovis (lane 5), or the dual-positive control (lane 6) were prominent and distinct.
Mixed infection was detected in 11 samples derived from nine animals (Table 2). In some instances, samples acquired from a single animal showed dual infection with M. tuberculosis and M. bovis, i.e., while one sample was positive for M. bovis, in the second sample M. tuberculosis was detected. These animals were also grouped in the mixed-infection category. Thirteen animals were identified in this group. By culture, one animal was shown to harbor both of the pathogens (mixed infection) (Table 3, serial no. 100), i.e., M. tuberculosis was isolated from the lymph node aspirate and M. bovis from milk. No individual sample was established by culture to harbor both M. tuberculosis and M. bovis, as was seen with samples examined by the N-PCR assay.
TABLE 3.
Comparative analysis of detection of pathogenic mycobacteria in cattle-derived samples by N-PCR and by standard identification tests
| Sample serial no. | Pathogenic mycobacterium(a) detected byd:
|
|||||
|---|---|---|---|---|---|---|
| N-PCR
|
Standard identificationa
|
|||||
| PSLNb | Blood | Milk | PSLN | Blood | Milk | |
| 92 | —e | M. tuberculosis | M. tuberculosis | — | M. tuberculosis | — |
| 104 | M. tuberculosis and M. bovisc | M. bovis | M. bovis | — | — | M. bovis |
| 105 | — | M. bovis | M. tuberculosis | — | — | M. tuberculosis |
| 128 | — | — | M. tuberculosis | — | — | M. tuberculosis |
| 129 | ND | M. tuberculosis | M. bovis | — | M. tuberculosis | — |
| 141 | M. bovis | — | — | M. bovis | — | — |
| 147 | — | — | M. bovis | — | — | M. bovis |
| 149 | — | — | M. bovis | — | — | M. bovis |
| 152 | M. tuberculosis and M. bovis | M. tuberculosis and M. bovis | NA | M. tuberculosis | — | NA |
| 91 | M. tuberculosis | — | M. tuberculosis | — | M. bovis | — |
| 94 | M. tuberculosis | M. tuberculosis | M. tuberculosis | M. bovis | — | — |
| 109 | — | — | M. tuberculosis | — | M. tuberculosis | — |
| 111 | — | — | M. tuberculosis | — | M. tuberculosis | — |
| 113 | — | M. bovis | M. bovis | M. tuberculosis | — | — |
| 134 | — | — | M. bovis | — | M. bovis | |
| 140 | M. bovis | M. tuberculosis | — | — | — | M. tuberculosis |
| 100 | — | — | — | M. tuberculosis | — | M. bovis |
Identification of cultivated mycobacterial isolates by standard tests (CDC, Atlanta, Ga.).
FNA derived from periscapular lymph gland.
M. tuberculosis and M. bovis detected in samples derived from a single animal/in an individual sample.
ND, speciation not done. PCR product identified as derived from mycobacteria belonging to the MTC. NA, not available.
no mycobacterial pathogen detected or isolated.
Comparative analysis of detection of M. tuberculosis and M. bovis by N-PCR and the standard culture technique.
Differences in detection and identification of M. tuberculosis and M. bovis in bovine samples by standard culture techniques and the N-PCR technique were observed. The results of the N-PCR and standard identification techniques correlated in 45% of the samples (85/189). N-PCR-based identification matched the results obtained by the standard identification techniques in nine samples (Table 3, serial no. 92, 104, 105, 128, 129, 141, 147, 149, and 152). Seventy-six samples were negative by both techniques. However, variation at the species level of identification of mycobacteria present in the samples derived from seven animals was seen (Table 3, serial no. 91, 94, 109, 111, 113, 134, and 140). Samples derived from one animal (Table 3, serial no. 100) were negative by N-PCR.
Table 4 depicts the comparative analysis of the standard culture technique with N-PCR for the detection of M. tuberculosis and M. bovis in cattle, based on tuberculin reactivity. The sensitivities of N-PCR and culture were calculated to be 97.3 and 29.7%, respectively. The specificity of N-PCR was lower (22.2%) than that of culture (77.7%).
TABLE 4.
Comparative analysis of N-PCR and culture by tuberculin reactivity status of the animals investigated
| Assay | Result | No. of animals with tuberculin statusa
|
Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | |
|---|---|---|---|---|---|---|---|
| R (n = 37) | NR (n = 27) | ||||||
| N-PCR | Positive | 36 | 21 | 97.3 | 22.2 | 63.2 | 85.7 |
| Negative | 1 | 6 | |||||
| Culture | Positive | 11 | 6 | 29.7 | 77.7 | 64.7 | 44.7 |
| Negative | 26 | 21 | |||||
R, reactor (≥5-mm induration at 72 h); NR, nonreactor (<5-mm induration at 72 h).
For all categories of animals, i.e., A, B, C, and D, and their samples, the sensitivities of detection of M. tuberculosis and/or M. bovis were dissimilar by the two assays. However, the trends of detection or isolation of M. tuberculosis and/or M. bovis from various animals were similar when taking into consideration the clinical categories of the animals examined (culture, P of <0.05; N-PCR, P of <0.01). In group A, all animals (100%, 20/20) were positive by N-PCR, whereas 45% (9/20) were positive by culture. This trend of detection decreased in the remaining groups. For groups B, C, and D, the percentages of positivity were determined to be 94, 90, and 66.6% by N-PCR and 12.5, 44, and 22.2% by culture, respectively. Identical detection patterns of M. tuberculosis and/or M. bovis were seen when considering all samples, namely, PSLN, blood, and milk. However, among the samples screened by the N-PCR assay, PSLN paralleled and reflected best the various groups of cattle studied (P < 0.01). The highest percentage of positivity was seen for group A (75%). Reductions in percent positivity were seen for the remaining groups, namely, 53% for group B, 30% for group C, and 33% for group D.
Seventy-five percent of the animals (6/8) included in group E were positive for M. tuberculosis and/or M. bovis by N-PCR. However, by culture no mycobacteria, either pathogenic or nonpathogenic, were isolated.
DISCUSSION
Handling of infected herds varies in accordance with local laws in developed countries and economic compulsions and religious norms in developing countries like India and some East Asian countries where the cow is revered. Rigorous containment and elimination of infected animals in developed countries has contributed to reducing the prevalence of bovine tuberculosis. However, despite the implementation of the test-and-slaughter policy in Great Britain bovine tuberculosis spread remains unchecked, indicating that there exist insidious mechanisms that facilitate the spread of bovine tuberculosis (14). The occurrence of bovine tuberculosis in wild animals and the movement of infected cattle from areas where the disease is endemic to regions relatively free of bovine tuberculosis have been cited as possible reasons (8, 14, 47). The implications of this in terms of habitual or organized or disorganized cattle migrations in developing countries is significant to the spread of M. bovis, M. tuberculosis, and other related and unrelated pathogens.
Reliable diagnosis of bovine tuberculosis in live animals remains a major problem among veterinarians. The tuberculin test has been used commonly to identify infected animals. Nevertheless, owing to problems of sensitivity and specificity, the currently used intradermal tuberculin test has been highly variable. Tuberculin reactivity has been known to be influenced by a variety of intrinsic host-related factors (immunological) as well as extrinsic factors, such as the technique, method, quality of the tuberculin used, etc. A negative tuberculin test does not rule out infection, especially in countries where the disease is highly endemic, whereas a positive reaction reflects a hypersensitivity reaction owing to previous exposure to mycobacteria. The tuberculin test is limited to the detection of infected animals, whereas from the viewpoint of describing the origin, link, and reservoirs of infection, identification of mycobacterial species in bovines has its merits.
Traditionally, culture followed by a panel of biochemical tests has been used for speciation of mycobacteria. This has inherent disadvantages, as most mycobacteria of clinical importance are slow growers and hence are difficult to isolate and cultivate. The time required for primary isolation ranges from 4 to 6 weeks in the case of solid culture media and 10 to 15 days by radiometric and other automated systems. Moreover, the paucibacillary nature of clinical samples also accounts for the low efficiency of isolation of pathogenic mycobacteria (11, 23, 39). In addition to difficulties in primary isolation of mycobacterial pathogens, particularly M. bovis, there have been reports of difficulty in differentiating closely related mycobacterial species (7, 30, 34, 44). Therefore, there is a need to develop molecular biological tools like PCR-based assays for reliable, early detection and speciation of mycobacteria in clinical samples and, as a consequence, for determination of the disease burden caused by diverse pathogenic mycobacteria.
Some of the difficulties that determine the success of isolation and detection of M. tuberculosis and/or M. bovis by culture or PCR-based assays are common to both assays and others are exclusive for each assay. Culture techniques depend on viable bacteria and therefore reflect ongoing infection. In the case of PCR, the test can be positive in the absence of viable integral mycobacteria. The success level of culture can be determined by (i) growth rates and the presence of associated microorganisms which would hinder the prospect of isolation of slow growers (several medium and fast growers, such as M. scrofulaceum, M. kansasii, M. flavescens, M. smegmatis, M. fortuitum, M. gastri, M. phlei, M. vaccae, and M. chelonae, were isolated from bovine samples in this study); (ii) notwithstanding prolonged incubation, the inability of potential isolates to adapt to in vitro culture conditions, especially in situations where the number of bacilli are limiting, which could result in false-negative results by culture; (iii) the variability in the tedious process of identification, which has been reported to be a problem; and (iv) the composition of the media used for primary isolation, particularly of M. bovis, from clinical isolates (17). Though PCR-based methods are useful for rapid detection of target DNA in suspected clinical samples, the efficacy of PCR assays can be influenced by the quality of target DNA extracted from appropriate samples and the presence of sample-derived PCR inhibitors. These problems have been addressed by several workers (3, 4, 9). Their methods and spiked controls have been adopted in the present study to overcome these problems. Unlike culture, the PCR technique does not distinguish between live and dead mycobacteria, a feature that is of the utmost importance when screening for viable mycobacteria in samples such as dairy products following pasteurization.
The N-PCR assay described in the present study is based on the hupB genes of M. bovis and M. tuberculosis. The specificity of the hupB-based PCR assay to detect and identify M. bovis and M. tuberculosis has been established by using a wide variety of mycobacterial and nonmycobacterial microorganisms (32). Further, the reliability of the assay was demonstrated by using M. bovis and M. tuberculosis strains from different geographical regions (32). The limit of detection by the N-PCR assay was shown to be five bacilli, equivalent to 50 fg of DNA. Kidane et al. (23) and Shah et al. (37) have reported the multiplex-PCR-based detection and differentiation of M. tuberculosis and M. bovis by use of clinical samples and mycobacterial isolates, respectively. The sensitivities of the assays were limited to detect 10 to 20 pg DNA of the tubercle bacilli. The sensitivity of the N-PCR technique may lead to false positives based on clinical criteria and in comparison to the culture techniques. The reasons for this could be due to (i) the detection of M. tuberculosis and M. bovis in clinical samples by the N-PCR prior to the onset of clinical signs and symptoms of tuberculosis and/or (ii) the presence of dead, noncultivatable bacilli in samples. The increased sensitivity of the N-PCR assay resulted in a lower specificity than that for culture (Table 4). Hence, the results of the N-PCR could potentially point to infection rather than disease. However, the probability of false-positive results being generated by the N-PCR technique is low because the likelihood of an incorrect region or nonspecific DNA being erroneously amplified twice is remote (46). Further, no correlation between tuberculin reactivity status and the results of culture and N-PCR was found among the animals examined.
We report the utility of the N-PCR assay for the direct detection of M. tuberculosis and M. bovis in bovine samples as an alternate method to the currently described spoligotyping technique, which is yet another test to distinguish members of the MTC (13, 20, 22, 35). The N-PCR assay not only permitted distinguishing M. tuberculosis and/or M. bovis in bovine samples but also facilitated categorizing different types of infection in cattle, that is, infection with either M. tuberculosis or M. bovis or both. This feature of the N-PCR has a distinct advantage over the spoligotyping technique, as mixed infections cannot be discerned by the latter. Mixed infection by M. tuberculosis and M. bovis in human lymph node biopsy specimens has also been reported (23). Besides mixed infection by M. tuberculosis and M. bovis, several other mycobacteria, such as members of Mycobacterium avium complex and M. fortuitum, have been reported to occur along with M. tuberculosis infection (25). The detection of both pathogens in the cattle investigated suggests a twin danger of infected cattle being a source of mycobacterial pathogens capable of infecting animals and humans. Contact between farm animals and humans would naturally facilitate a bidirectional infection of mycobacterial pathogens.
The presence of M. tuberculosis in bovine samples is indicative of reverse zoonosis, as has been reported for animals in contact with humans (1, 10, 12). It has been documented that animals can be infected by exposure to any individual shedding the organism (1, 12). Sjogren and Hillerdal (41) cited several examples of human-to-cattle transmission and stressed the potential danger that patients with smear-positive pulmonary tuberculosis pose to animals. Grange and Yates (18) reported that farm workers urinating in cowsheds might represent a source of infection for animals. Animals infected with M. tuberculosis constitute a potential hazard of transmission of virulent tubercle bacilli back to humans (12). Therefore, there is a compelling need to detect tuberculosis among cattle handlers and farmers, as humans are the major reservoir of M. tuberculosis, unlike with M. bovis. Speciation of these pathogens would help the formulation of public heath strategies to interrupt the transmission chain not only intrinsically among cattle but also between humans and cattle. This demands the implementation of rigorous, strict policies regarding the detection of tuberculosis among animals and cattle handlers. Besides speciation of mycobacteria isolated from cattle, molecular markers need to be included to establish the unequivocal relationship between strains isolated from humans and those isolated from cattle.
The identification of M. tuberculosis and M. bovis by the N-PCR assay in bovine samples has helped to bring into focus (i) the prevalence and the incidence of M. bovis and M. tuberculosis infections in bovines and (ii) the grave implications of the high frequency of occurrence of potential human mycobacterial pathogens among cattle of economic importance. The assay would prove especially useful in developing countries with a high incidence of infected livestock (16). M. bovis has been known to spread to humans from infected cattle (zoonotic tuberculosis) by aerosol or by consumption of contaminated dairy products (6, 28). The epidemiological impact of M. bovis infection in humans has not been assessed. This assay has been utilized for the detection of M. bovis infection in extrapulmonary samples of human origin (N. P. Shah et al., submitted for publication). The presence and occurrence of these twin pathogens in the environment have grave implications for the currently adopted strategies for prevention and control of human tuberculosis. The occurrence of simultaneous infection of M. bovis and M. tuberculosis in an individual sample reflects the concurrent infection that occurs due to the prevalence and circulation of both of these pathogens in the environment.
Therefore, the current N-PCR assay would be of immense utility in redefining research priorities and public health strategies for control and prevention of tuberculosis in farm animals as well as in humans, since the duo, M. tuberculosis and M. bovis, is capable of infection and of causing both human and bovine tuberculosis. Hence, there is a need to develop techniques similar to the currently described N-PCR which would provide evidence of the occurrence of tuberculosis in humans and cattle by these common mycobacterial pathogens. This in turn would provide a sound rationale for the generation of hitherto-elusive antitubercular vaccines to protect susceptible humans and animals alike.
Acknowledgments
We thank J. S. Tyagi for the help rendered during the execution of the project.
This work was supported by DBT (Department of Biotechnology) India. A.S. was a recipient of an SRF fellowship from UGC (University Grant Commission) India.
REFERENCES
- 1.Ayele, W. Y., S. D. Neil, J. Zinsstag, M. G. Weiss, and I. Pavlik. 2004. Bovine tuberculosis: an old disease but a new threat to Africa. Int. J. Tuberc. Lung Dis. 8:924-927. [PubMed] [Google Scholar]
- 2.Barouni, A. S., C. J. Augusto, M. T. Lopes, M. S. Zanini, and C. E. Salas. 2004. A pncA polymorphism to differentiate between Mycobacterium bovis and Mycobacterium tuberculosis. Mol. Cell. Probes 18:167-170. [DOI] [PubMed] [Google Scholar]
- 3.Chakravorty, S., and J. S. Tyagi. 2001. Novel use of guanidinium isothiocyanate in isolation of M. tuberculosis DNA from clinical materials. FEMS Microbiol. Lett. 205:113-117. [DOI] [PubMed] [Google Scholar]
- 4.Chakravorty, S., M. Dudeja, M. Hanif, and J. S. Tyagi. 2005. Utility of universal sample processing methodology, combining smear microscopy, culture, and PCR, for diagnosis of pulmonary tuberculosis. J. Clin. Microbiol. 43:2703-2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chimara, E., L. Ferrazoli, and S. C. Leão. 2004. Mycobacterium tuberculosis complex differentiation using gyrB-restriction fragment length polymorphism analysis. Mem. Inst. Oswaldo Cruz 99:745-748. [DOI] [PubMed] [Google Scholar]
- 6.Cosivi, O., J. M. Grange, C. J. Daborn, M. C. Ravigilone, T. Fujikura, D. Cousins, R. A. Robinson, H. F. A. K. Huchzermeyer, I. De Kanntor, and F. X. Meslin. 1998. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg. Infect. Dis. 4:59-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.David, H. L., J. Marie-Therese, A. Jumin, J. Grandry, and E. H. Lehman. 1978. Numerical taxonomy analysis of Mycobacterium africanum. Int. J. Syst. Bacteriol. 28:467-472. [Google Scholar]
- 8.Delahay, R. J., C. L. Cheeseman, and R. S. Clifton-Hadely. 2001. Wildlife disease reservoirs: the epidemiology of Mycobacterium bovis infection in the European badger (Meles meles) and other British mammals. Tuberculosis 81:43-49. [DOI] [PubMed] [Google Scholar]
- 9.Elisenach, K. D. 1998. Molecular diagnostics, p. 161-179. In C. Ratledge and J. Dale (ed.), Mycobacterium—molecular biology and virulence. Blackwell Science, Oxford, United Kingdom.
- 10.Erwin, P. C., D. A. Bemis, S. B. McCombs, L. L. Sheeler, I. M. Himelright, S. K. Halford, L. Diem, B. Metchock, T. F. Jones, M. G. Schilling, and B. V. Thomsen. 2004. Mycobacterium tuberculosis transmission from human to canine. Emerg. Infect. Dis. 10:2258-2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fanning, A. 1999. Tuberculosis: extrapulmonary disease. CMAJ 160:1597-1603. [PMC free article] [PubMed] [Google Scholar]
- 12.Fritsche, A., R. Engel, D. Buhl, and J. P. Zellweger. 2004. Mycobacterium bovis tuberculosis: from animal to man and back. Int. J. Tuberc. Lung Dis. 8:903-904. [PubMed] [Google Scholar]
- 13.Gibson, A. L., G. Hewinson, T. Goodchild, B. Watt, A. Story, J. Inwald, and F. A. Drobniewski. 2004. Molecular epidemiology of disease due to Mycobacterium bovis in humans in the United Kingdom. J. Clin. Microbiol. 42:431-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert, M., A. Mitchell, D. Bourn, J. Mawdsley, R. Clifton-Hadley, and W. Wint. 2005. Cattle movements and bovine tuberculosis in Great Britain. Nature 435:491-496. [DOI] [PubMed] [Google Scholar]
- 15.Goodchild, A. V., and R. S. Clifton-Hadely.2001. Cattle-to-cattle transmission of Mycobacterium bovis. Tuberculosis 81:23-41. [DOI] [PubMed] [Google Scholar]
- 16.Grange, J. M. 2001. Mycobacterium bovis infection in human beings. Tuberculosis 81:71-77. [DOI] [PubMed] [Google Scholar]
- 17.Grange, J. M., J. D. Collins, L. O'Reilly, E. Costello, and M. D. Yates. 1990. Identification and characteristics of Mycobacterium bovis isolated from cattle, badgers and deer in the Republic of Ireland. Ir. Vet. J. 43:33-35. [Google Scholar]
- 18.Grange, J. M., and M. D. Yates. 1994. Zoonotic aspects of Mycobacterium bovis infection. Vet. Microbiol. 40:137-151. [DOI] [PubMed] [Google Scholar]
- 19.Haas, W. H., K. Schilke, J. Brand, B. Amthor, K. Weyer, P. B. Fourie, G. Bretzel, V. Sticht-Groh, and H. J. Bremer. 1997. Molecular analysis of katG gene mutations in strains of Mycobacterium tuberculosis complex from Africa. Antimicrob. Agents Chemother. 41:1601-1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haddad, N., A. Ostyn, C. Karoui, M. Masselot, M. F. Thorel, S. L. Hughes, J. Inwald, R. G. Hewinson, and B. Durand. 2001. Spoligotype diversity of Mycobacterium bovis strains isolated in France from 1979 to 2000. J. Clin. Microbiol. 39:3623-3632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huard, R. C., L. C. de Oliveira Lazzarini, W. R. Butler, D. van Soolingen, and J. L. Ho. 2003. PCR-based method to differentiate the subspecies of the Mycobacterium tuberculosis complex on the basis of genomic deletions. J. Clin. Microbiol. 41:1637-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamerbeek, J., L. Schouls, A. Kolk, M. van Agterveld, D. van Soolingen, S. Kuijper, A. Bunschoten, H. Molhuizen, R. Shaw, M. Goyal, and J. van Embden. 1997. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J. Clin. Microbiol. 35:907-914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kidane, D., J. O. Olobo, A. Habte, Y. Negesse, A. Aseffa, G. Abate, M. A. Yassin, K. Bereda, and M. Harboe. 2002. Identification of the causative organism of tuberculous lymphadenitis in Ethiopia by PCR. J. Clin. Microbiol. 40:4230-4234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar, G. S., A. K. Sharma, P. K. R. Iyer, and M. C. Prasad. 1998. Tuberculosis in crossbred dairy cattle. Indian J. Vet. Pathol. 22:12-15. [Google Scholar]
- 25.Leite, C. Q. F., C. W. O. de Souza, and S. R. Leite. 1998. Identification of mycobacteria by thin layer chromatographic analysis of mycolic acids and conventional biochemical method: four years of experience. Mem. Inst. Oswaldo Cruz 93:801-805. [DOI] [PubMed] [Google Scholar]
- 26.Michel, A. L. 2002. Implications of tuberculosis in African wildlife and livestock. Ann. N. Y. Acad. Sci. 969:251-255. [DOI] [PubMed] [Google Scholar]
- 27.Mishra, J. K., S. N. Panda, and H. K. Panda. 1997. Prevalence of bovine tuberculosis among farm cattle in Orissa. Indian Vet. J. 74:195-198. [Google Scholar]
- 28.Moda, G., C. J. Daborn, J. M. Grange, and O. Cosivi. 1996. The zoonotic importance of Mycobacterium bovis. Tuber. Lung Dis. 77:103-108. [DOI] [PubMed] [Google Scholar]
- 29.Mohamed, A. M., D. R. Bastola, G. P. Morlock, R. C. Cooksey, and S. H. Hinrichs. 2004. Temperature-mediated heteroduplex analysis for detection of pncA mutations associated with pyrazinamide resistance and differentiation between Mycobacterium tuberculosis and Mycobacterium bovis by denaturing high-performance liquid chromatography. J. Clin. Microbiol. 42:1016-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niemann, S., E. Richter, and S. Rüsch-Gerdes. 2000. Differentiation among members of the Mycobacterium tuberculosis complex by molecular and biochemical features: evidence for two pyrazinamide-susceptible subtypes of M. bovis. J. Clin. Microbiol. 38:152-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pavlik, I., M. Machackova, W. Y. Ayele, et al. 2002. Incidence of bovine tuberculosis in wild and domestic animals other than cattle in six Central European countries during 1990-1999. Vet. Med. Czech. 47:122-131. [Google Scholar]
- 32.Prabhakar, S., A. Mishra, A. Singhal, V. M. Katoch, S. S. Thakral, J. S. Tyagi, and H. K. Prasad. 2004. Use of the hupB gene encoding a histone-like protein of Mycobacterium tuberculosis as a target for detection and differentiation of M. tuberculosis and M. bovis. J. Clin. Microbiol. 42:2724-2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richter, E., M. Weizenegger, A.-M. Fahr, and S. Rüsch-Gerdes. 2004. Usefulness of the GenoType MTBC assay for differentiating species of the Mycobacterium tuberculosis complex in cultures obtained from clinical specimens. J. Clin. Microbiol. 42:4303-4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rivero, A., M. Marquez, J. Santos, A. Pinedo, M. A. Sanchez, A. Esteve, S. Samper, and C. Martin. 2001. High rate of tuberculosis re-infection during a nosocomial outbreak of multi-drug-resistant tuberculosis caused by Mycobacterium bovis strain B. Clin. Infect. Dis. 32:159-161. [DOI] [PubMed] [Google Scholar]
- 35.Roring, S., M. S. Hughes, R. A. Skuce, and S. D. Neill. 2000. Simultaneous detection and strain differentiation of Mycobacterium bovis directly from bovine tissue specimens by spoligotyping. Vet. Microbiol. 74:227-236. [DOI] [PubMed] [Google Scholar]
- 36.Scorpio, A., and Y. Zhang. 1996. Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat. Med. 2:662-667. [DOI] [PubMed] [Google Scholar]
- 37.Shah, D. H., R. Verma, C. S. Bakshi, and R. K. Singh. 2002. A multiplex-PCR for the differentiation of Mycobacterium bovis and Mycobacterium tuberculosis. FEMS Microbiol. Lett. 214:39-43. [DOI] [PubMed] [Google Scholar]
- 38.Sharma, D. R., M. S. Kwatra, D. V. Joshi, and D. K. Sharma. 1994. Prevalence of tuberculosis under rural and organized farm conditions. Indian J. Comp. Microbiol. Immunol. Infect. Dis. 15:5-7. [Google Scholar]
- 39.Singh, K. K., M. Muralidhar, A. Kumar, T. K. Chattpoadhyaya, K. Kapila, M. K. Singh, N. K. Jain, and J. S. Tyagi. 2000. Comparison of in house polymerase chain reaction with conventional techniques for the detection of Mycobacterium tuberculosis DNA in granulomatous lymphadenopathy. J. Clin. Pathol. 53:355-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh, K. S., R. Verma, and D. H. Shah. 2004. Molecular fingerprinting of clinical isolates of Mycobacterium bovis and Mycobacterium tuberculosis from India by restriction fragment length polymorphism (RFLP). J. Vet. Sci. 5:331-335. [PubMed] [Google Scholar]
- 41.Sjogren, I., and O. Hillerdal. 1978. Bovine tuberculosis in man—reinfection or endogenous exacerbation. Scand. J. Respir. Dis. 59:167-170. [PubMed] [Google Scholar]
- 42.Sreevatsan, S., P. Escalante, X. Pan, D. A. Gillies II, S. Siddiqui, C. N. Khalaf, B. N. Kreiswirth, P. Bifani, L. G. Adams, T. Ficht, V. S. Perumaalla, M. D. Cave, J. D. A. van Embden, and J. M. Musser. 1996. Identification of a polymorphic nucleotide in oxyR specific for Mycobacterium bovis. J. Clin. Microbiol. 34:2007-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thoen, C. O., and J. H. Steele (ed.) 1995. Mycobacterium bovis infection in animals and humans. Iowa State University Press, Ames, Iowa.
- 44.van Soolingen, D., T. Hoogenboezem, P. E. W. de Haas, P. W. M. Hermans, M. A. Koedam, K. S. Teppema, P. J. Brennan, G. S. Besra, F. Portaels, J. Top, L. M. Scouls, and J. D. A. van Embden. 1997. A novel pathogenic taxon of the Mycobacterium tuberculosis complex, Canetti: characterization of an exceptional isolate from Africa. Int. J. Syst. Bacteriol. 47:1236-1245. [DOI] [PubMed] [Google Scholar]
- 45.Vestal, A. L. 1977. Procedures of isolation and identification of mycobacteria. U.S. Department of Health, Education, and Welfare publication no. (CDC) 77-8230, p. 65-98. Centers for Disease Control, Atlanta, Ga.
- 46.Wang, J.-Y., L.-N. Lee, C.-S. Chou, C.-Y. Huang, S.-K. Wang, H.-C. Lai, P.-R. Hsueh, and K.-T. Luh. 2004. Performance assessment of a nested-PCR assay (the RAPID BAP-MTB) and the BD ProbeTec ET system for detection of Mycobacterium tuberculosis in clinical specimens. J. Clin. Microbiol. 42:4599-4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wint, G. R., T. P. Robinson, D. M. Bourn, P. A. Durr, S. I. Hay, S. E. Randolph, and D. J. Rogers. 2002. Mapping bovine tuberculosis in Great Britain using environmental data. Trends Microbiol. 10:441-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. 1999. The world health report 1999: making a difference. World Health Organization, Geneva, Switzerland.