Short abstract
Amid recent improvements in cancer care within the United Kingdom, inadequate radiotherapy capacity compromises care and is an important and underappreciated problem
A recent BMJ editorial described the exciting potential for heavy particle therapy in the management of relatively uncommon cancers and discussed responses to this development in the United Kingdom.1 Such progress should not divert attention from a much less comfortable current reality. Many UK radiotherapy departments have inadequate treatment capacity, and the problems experienced by individual patients because of extended waiting times for radiotherapy as a consequence of this are sometimes picked up by the media. After the inevitable outpourings of political concern the spotlight of media attention moves elsewhere, but the basic problem—inadequate radiotherapy capacity—remains. We describe the back-ground to this problem, the evidence that delays in starting radiotherapy may lead to poor outcomes, and some of the issues that need to be considered when managing overstretched radiotherapy services.
Background
Treatment of malignant disease often uses a combination of surgery, radiotherapy, and chemotherapy. After surgery, radiotherapy is the next greatest contributor to cancer cure rates. In the 1970s and 80s it was thought that improved systemic therapy would yield dramatic outcome improvements in common solid cancers and that the need for radiotherapy would diminish. This was fuelled by impressive results with effective cytotoxic agents in paediatric, germ cell, and haematological cancers. Consequently, until recently there was little investment in basic and clinical research in radiotherapy and a reluctance to invest in radiotherapy services.
Demand for radiotherapy has increased because of the rising incidence of cancer, more indications for treatment, greater access to treatment resulting from improved multidisciplinary care, and recognition that chemotherapy does not usually ensure long term loco-regional control of most common solid cancers. In many circumstances radiotherapy offers survival and local control outcomes similar to radical surgery, with the benefits of organ preservation.
Over the last five or so years, substantial funding has been made available for the purchase of replacement and new linear accelerators (linacs) and for supporting simulation and radiotherapy planning equipment—but many radiotherapy departments cannot meet demand because of shortages of radiographers, physicists, and dosimetrists. Increased numbers of training places have been created to improve the complement of these critical staff groups, but current shortages mean that in many centres the disparity between demand and capacity is great. Radiotherapy services in the United Kingdom are inferior to those in most developed countries and indeed in many poorer countries.2-6
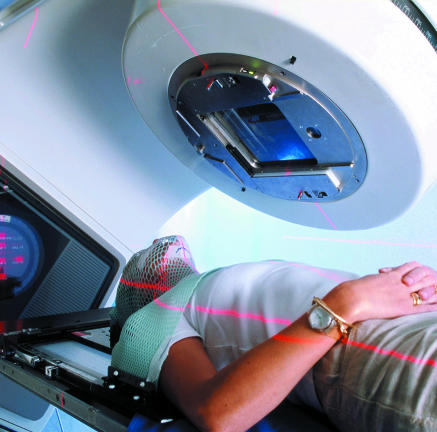
Figure 1.
The UK needs better radiotherapy services
Credit: BSIP/RAGUET/SPL
Lessening the consequences of inadequate treatment capacity
In services that deliver vital treatments, an excess of demand over supply causes a delay between referral and the start of treatment. Approaches used to lessen the consequences of inadequate treatment capacity include reducing the number of treatment sessions, transferring patients to other centres, or some form of rationing.
In palliative radiotherapy as few radiotherapy fractions as possible are used, and in traditional radical treatment protocols reducing the number of fractions may be considered in some tumour sites where there is an evidence base to support this. In most circumstances, though, concerns around efficacy and the effect on normal tissue limit this practice. In the United Kingdom, variation in fractionation has been reduced by better evidence, the use of protocols, and by extreme pressure on treatment capacity.5
Changes in work pattern and skills mix have increased treatment capacity slightly, but centres experiencing major difficulties have already made such changes. Even if other radiotherapy centres have space, transferring patients is difficult on a practical basis, hindered by cumbersome commissioning arrangements, and removes patients from the care of their local multidisciplinary team.
The demand for radiotherapy could be reduced by limiting the indications for treatment. For instance, within a patient population where postoperative radiotherapy is routine, the benefit of radiotherapy is correspondingly less than “average” in subgroups with a lower than average risk of local recurrence—but the selection of such subgroups is not necessarily supported by a statistically secure evidence base. Also, withholding radiotherapy in these circumstances may breach national (NICE) or local (Cancer Network) guidance. If the cancer recurs, this process could expose clinicians to complaints or litigation.
Delays in starting treatment
Many radiotherapy centres have substantial waiting lists despite efforts to prevent these from occurring.2-6 In patients with incurable cancer, a delay in receiving palliative radiotherapy prolongs symptoms and causes distress but is unlikely to adversely affect survival. In radical radiotherapy, where longer term disease control or cure are realistic treatment objectives, delays affect control of the cancer, organ preservation, and mortality.
It is a central tenet of modern radiobiology that the probability of controlling tumours decreases as tumours grow. Because prospective trials of delayed versus immediate radiotherapy are confounded by the use of systemic therapy, the evidence that delaying the start of radiotherapy may be harmful is derived from retrospective, cohort, and epidemiological studies. Despite this weakness, a growing body of data gives rise to concern.
Longer radiotherapy waiting times were associated with diminished survival outcomes for patients treated radically for cervical cancer and soft tissue sarcoma.7,8 In 29 patients initially suitable for radical radiotherapy for lung cancer who waited on average 94 days between first hospital visit and starting treatment, six (21%) became unfit for radical radiotherapy.9 In head and neck cancer, two large studies report a significantly increased local relapse rate if radical radiotherapy was delayed beyond 40 days,10,11 but another did not confirm these findings.12 A systematic review of 12 studies of the impact of delay in instituting adjuvant radiotherapy after surgery for head and neck cancer found a threefold increase in local recurrence if radiotherapy was delayed more than six weeks.13
The management of early breast cancer makes a colossal demand on radiotherapy services, and many studies have addressed the impact of delayed adjuvant radiotherapy in early breast cancer. A systematic review of 21 of these studies showed that local recurrence was increased by 60% if the interval between surgery and radiotherapy exceeded eight weeks.13 In a large epidemiological study involving 7800 patients treated with breast conserving surgery and postoperative radiotherapy, a surgery-radiotherapy delay of 20 weeks or more was associated with significantly increased mortality.14 These studies strongly suggest that delayed radiotherapy is harmful, and it would be specious to rely on the methodological shortcomings of these types of analyses to assert that delayed radiotherapy is safe.
Who gets which treatment?
Those with managerial, political, and clinical responsibility for managing radiotherapy services in the many UK departments with capacity problems find themselves between a rock and a hard place. They have the unenviable task of juggling competing clinical priorities and pressures from stakeholder groups in an environment that emphasises equity and speed of access as well as the primacy of patient choice. There is no apparent national guidance or precedent for the unpleasant choices that may have to be made.
Perhaps patients with potentially curable malignancy, for whom radical radiotherapy represents the only treatment option, should receive priority treatment—but such prioritisation will have a negative impact on the delays experienced by other groups of patients. In some clinical situations, selecting radical surgery rather than radiotherapy might lead to lower quality of life and organ loss but an equal chance of survival (laryngectomy in preference to radiotherapy, for example). In others, a more aggressive surgical option could obviate a need for postoperative irradiation (mastectomy in preference to breast conserving surgery, for example).
Discussions are needed
When concerns over delayed radiotherapy influence the choice of treatment, care must be taken in sharing information with patients and obtaining informed consent. Such discussions take place shortly after malignancy has been diagnosed, a time of great distress and vulnerability. When, for example, surgical treatment for early breast cancer is being considered (a treatment that places a massive demand on radiotherapy services), delayed radiotherapy cannot be confirmed to be safe; also, local control and survival in relation to the choice between mastectomy versus breast conserving surgery with (delayed) breast irradiation may not be equivalent. Patients must be involved in these discussions so they can make an informed choice about their treatment. In other services, waiting lists can be circumvented by treatment in private centres, but this does not apply to radiotherapy as no such centres exist outside London.
We believe that these dilemmas warrant discussion at a national level, although such discussions will be difficult and emotionally and politically charged as they will embrace options that represent a retrograde step in cancer care. The disparities between demand and supply that are shown in radiotherapy waiting lists will increase in the absence of intervention. In the light of growing waiting lists, avoiding discussion of active intervention represents the tacit acceptance of prioritisation by default and is not a responsible approach. Clinical oncologists in the United Kingdom are accustomed to hoping for improvements—but demographic changes, increased cancer screening, and the ongoing correction of a legacy of underutilisation will continue to place radiotherapy services under pressure.
Summary points
Cancer care has improved greatly over the past decade
Waiting lists for radiotherapy are still long
If we cannot or will not remedy shortfalls in radiotherapy treatment capacity, we must adapt patient management strategies accordingly
Novel approaches to treatment and improved applications of existing technology in radiotherapy offer better quality of treatment, improved chances of tumour control, and reduced morbidity. Evidence of better clinical outcomes with heavy particle treatment for small but critical patient groups adds to the complexity of designing a national strategy. The scale of investment required in the United Kingdom to allow capacity to match demand is complex and large. It requires a consistent national policy and priority that is not bound by political time frames and funding cycles.
Editorial by Gabbay and Walley and pp 109, 112
Sources and contributors: DD and AMC are consultant clinical oncologists with a special interest in breast and gastrointestinal cancer respectively. Both have been involved with managing the issue locally. AMC also is a member of a national group addressing the problem of radiotherapy capacity in the United Kingdom.
Conflict of interest: None declared.
References
- 1.Jones B, Burnet N. Radiotherapy for the future. BMJ 2005;330: 979-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Probst H, Holmes M, Dodwell D. Radiotherapy waiting times, resources and protocols for breast carcinoma: a survey of UK Radiotherapy centres. J Radiother Practice 2003;3: 113-21. [Google Scholar]
- 3.Royal College of Radiologists. The provision and replacement of radiotherapy equipment. London: RCR, 2000. (9BFCO(00)2.)
- 4.Royal College of Radiologists. Equipment, workload and staffing for radiotherapy in the UK 1999-2002. London: RCR, 2003. (BFCO(03)3.)
- 5.Ash D, Barrett A. Hinks A, Squire C on behalf of the Royal College of Radiologists. Re-audit of radiotherapy waiting times 2003. Clin Oncol 2004;16: 387-94. [DOI] [PubMed] [Google Scholar]
- 6.Bentzen S, Heeren G, Cottier B, Slotman B, Glimelius B, Lievens Y, et al. Towards evidence-based guidelines for radiotherapy infrastructure and staffing needs in Europe: the ESTRO QUARTS project. Radiother Oncol 2005;75: 355-65. [DOI] [PubMed] [Google Scholar]
- 7.Choan E, Dahrouge S, Samant R, Mirzaei A, Price J. Radical radiotherapy for cervix cancer: the effect of waiting time on outcome. Int J Radiat Oncol Biol Phys 2005;61: 1071-7. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz DL, Einck J, Hunt K, Bruckner J, Conrad E, Koh WJ, et al. The effect of delayed postoperative irradiation on local control of soft tissue sarcomas of the extremity and torso. Int J Radiat Oncol Biol Phys 2002;52(5): 1352-9. [DOI] [PubMed] [Google Scholar]
- 9.O'Rourke-N, Edwards-R. Lung cancer treatment waiting times and tumour growth. Clin Oncol 2000;12: 141-4. [DOI] [PubMed] [Google Scholar]
- 10.Fortin A, Bairati I, Albert M, Moore L, Allard J, Couture C. Effect of treatment delay on outcome of patients with early-stage head-and-neck carcinoma receiving radical radiotherapy. Int J Radiat Oncol Biol Phys 2002;52: 929-36. [DOI] [PubMed] [Google Scholar]
- 11.Waaijer A, Terhaard CHJ, Dehnad H, Hordijk GJ, van-Leeuwen MS, Raaymakers CPJ, et al. Waiting times for radiotherapy: consequences of volume increase for the TCP in oropharyngeal carcinoma. Radiother Oncol 2003;66: 271-6. [DOI] [PubMed] [Google Scholar]
- 12.León X, de-Vega M, Orús C, Morán J, Vergés J, Quer M. The effect of waiting time on local control and survival in head and neck carcinoma patients treated with radiotherapy. Radiother Oncol 2003;66: 277-8. [DOI] [PubMed] [Google Scholar]
- 13.Huang J, Barbera L, Brouwers M, Browman G, Mackillop WJ. Does delay in starting treatment affect the outcomes of radiotherapy? A systematic review. J Clin Oncol 2003;21: 555-63. [DOI] [PubMed] [Google Scholar]
- 14.Mikeljevic J, Haward R, Johnston C, Crellin A, Dodwell D, Jones A, et al. Trends in postoperative radiotherapy delay and the effect on survival in breast cancer patients treated with conservation surgery. Br J Cancer 2004;90: 1343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]