Abstract
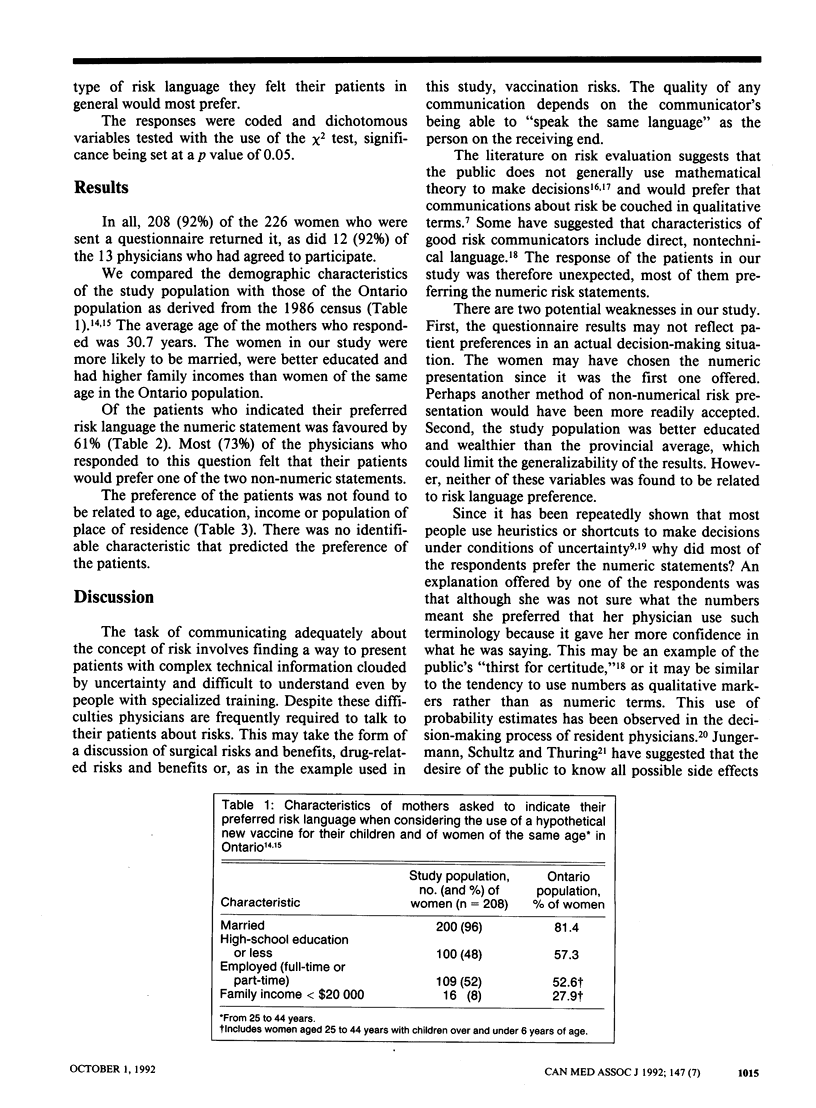
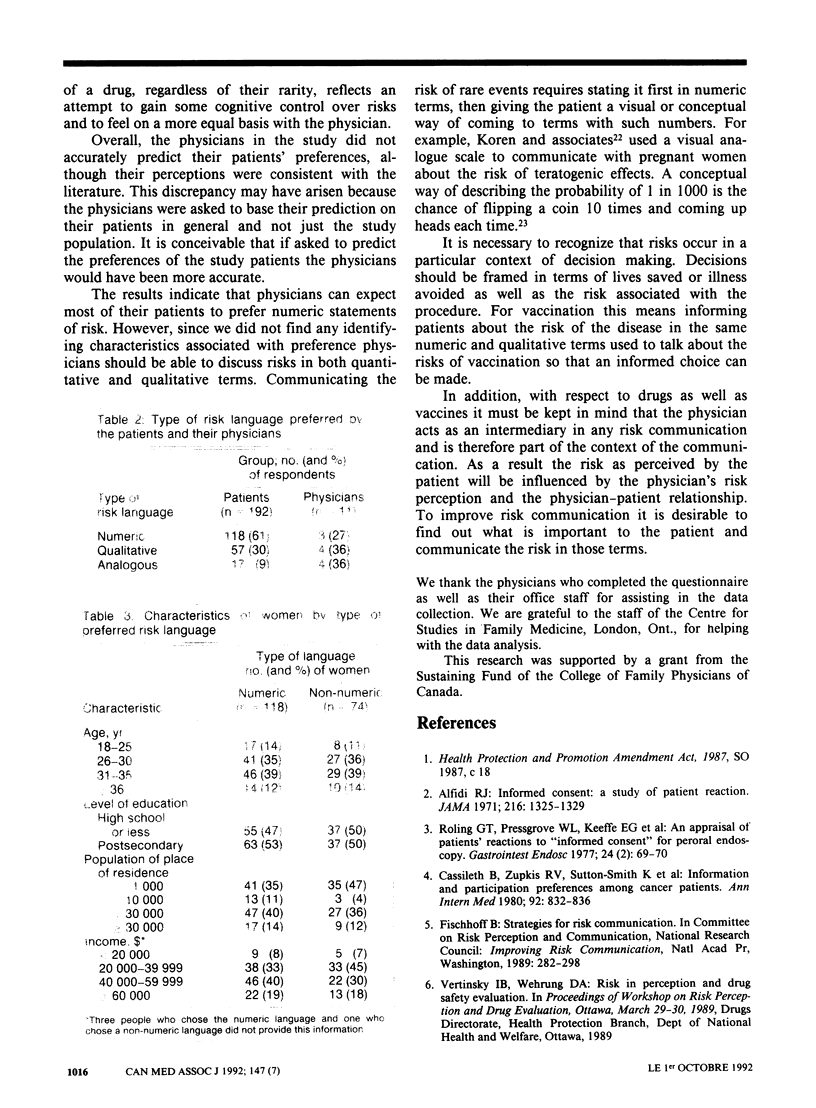
OBJECTIVES: To determine the type of risk language preferred by mothers considering the use of hypothetical new vaccine for their children and to compare their choice with what their physicians perceived they would prefer. DESIGN: Mail survey. SETTING: Thirteen family practices in southwestern Ontario. PARTICIPANTS: Women with at least one child between the ages of 6 months and 5 years and their physicians. MAIN OUTCOME MEASURES: Preferred risk language and physicians' predictions about patient preference. RESULTS: Of the 226 women sent the questionnaire 208 (92%) responded. Of the 192 who indicated their risk language preference 118 (61%) chose a numeric statement. Of the 11 physicians who answered the question 8 (73%) predicted that their parents would prefer non-numeric statements. Although the women in the study were more likely to be married, were better educated and had higher family incomes than women of the same age in the Ontario population, risk language preference was not found to be related to any of those demographic characteristics. CONCLUSION: Physicians must be prepared to outline the risks associated with vaccination in both quantitative and qualitative terms.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alfidi R. J. Informed consent. A study of patient reaction. JAMA. 1971 May 24;216(8):1325–1329. doi: 10.1001/jama.216.8.1325. [DOI] [PubMed] [Google Scholar]
- Cassileth B. R., Zupkis R. V., Sutton-Smith K., March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980 Jun;92(6):832–836. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- Freeman T. R., Bass M. J. Determinants of maternal tolerance of vaccine-related risks. Fam Pract. 1992 Mar;9(1):36–41. doi: 10.1093/fampra/9.1.36. [DOI] [PubMed] [Google Scholar]
- Jungermann H., Schütz H., Thüring M. Mental models in risk assessment: informing people about drugs. Risk Anal. 1988 Mar;8(1):147–155. doi: 10.1111/j.1539-6924.1988.tb01161.x. [DOI] [PubMed] [Google Scholar]
- Keeney R. L., von Winterfeldt D. Improving risk communication. Risk Anal. 1986 Dec;6(4):417–424. doi: 10.1111/j.1539-6924.1986.tb00954.x. [DOI] [PubMed] [Google Scholar]
- Koplan J. P., Schoenbaum S. C., Weinstein M. C., Fraser D. W. Pertussis vaccine--an analysis of benefits, risks and costs. N Engl J Med. 1979 Oct 25;301(17):906–911. doi: 10.1056/NEJM197910253011703. [DOI] [PubMed] [Google Scholar]
- Koren G., Bologa M., Long D., Feldman Y., Shear N. H. Perception of teratogenic risk by pregnant women exposed to drugs and chemicals during the first trimester. Am J Obstet Gynecol. 1989 May;160(5 Pt 1):1190–1194. doi: 10.1016/0002-9378(89)90186-5. [DOI] [PubMed] [Google Scholar]
- Politser P. Decision analysis and clinical judgment. A re-evaluation. Med Decis Making. 1981;1(4):361–389. doi: 10.1177/0272989X8100100406. [DOI] [PubMed] [Google Scholar]
- Roling G. T., Pressgrove L. W., Keeffe E. B., Raffin S. B. An appraisal of patients' reactions to "informed consent" for peroral endoscopy. Gastrointest Endosc. 1977 Nov;24(2):69–70. doi: 10.1016/s0016-5107(77)73453-4. [DOI] [PubMed] [Google Scholar]


