Abstract
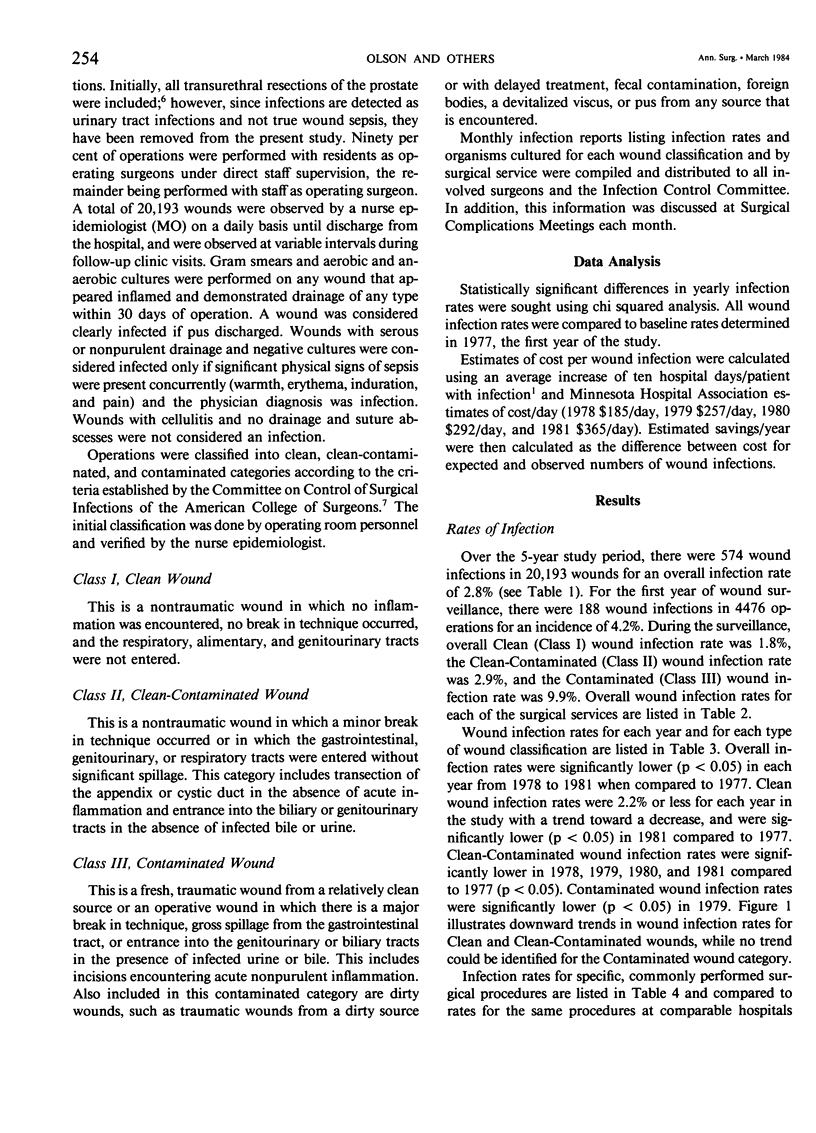
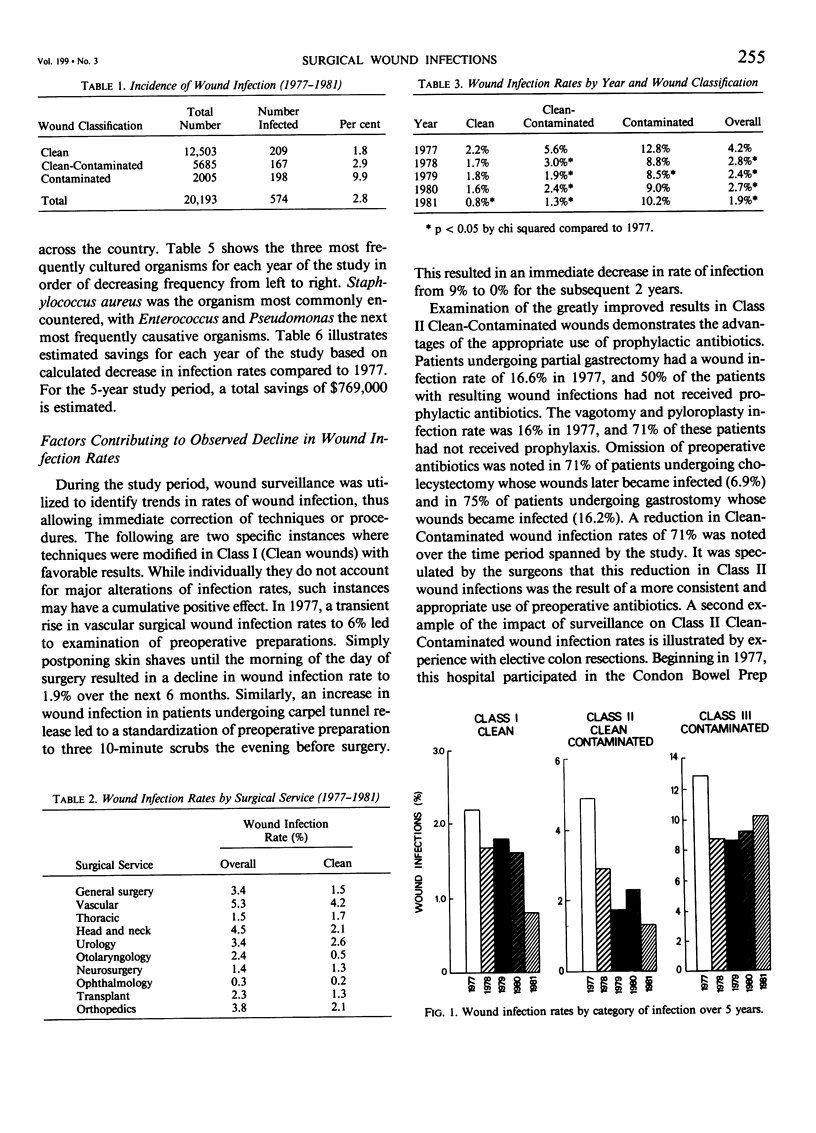
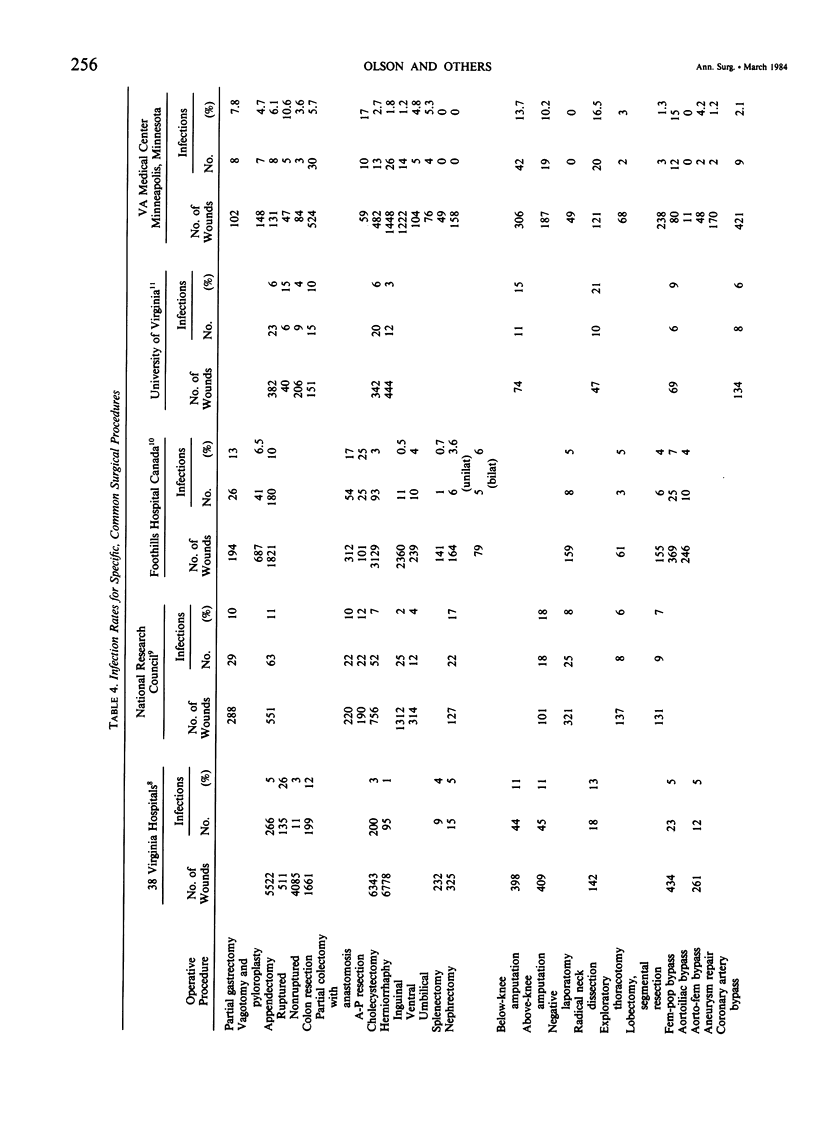
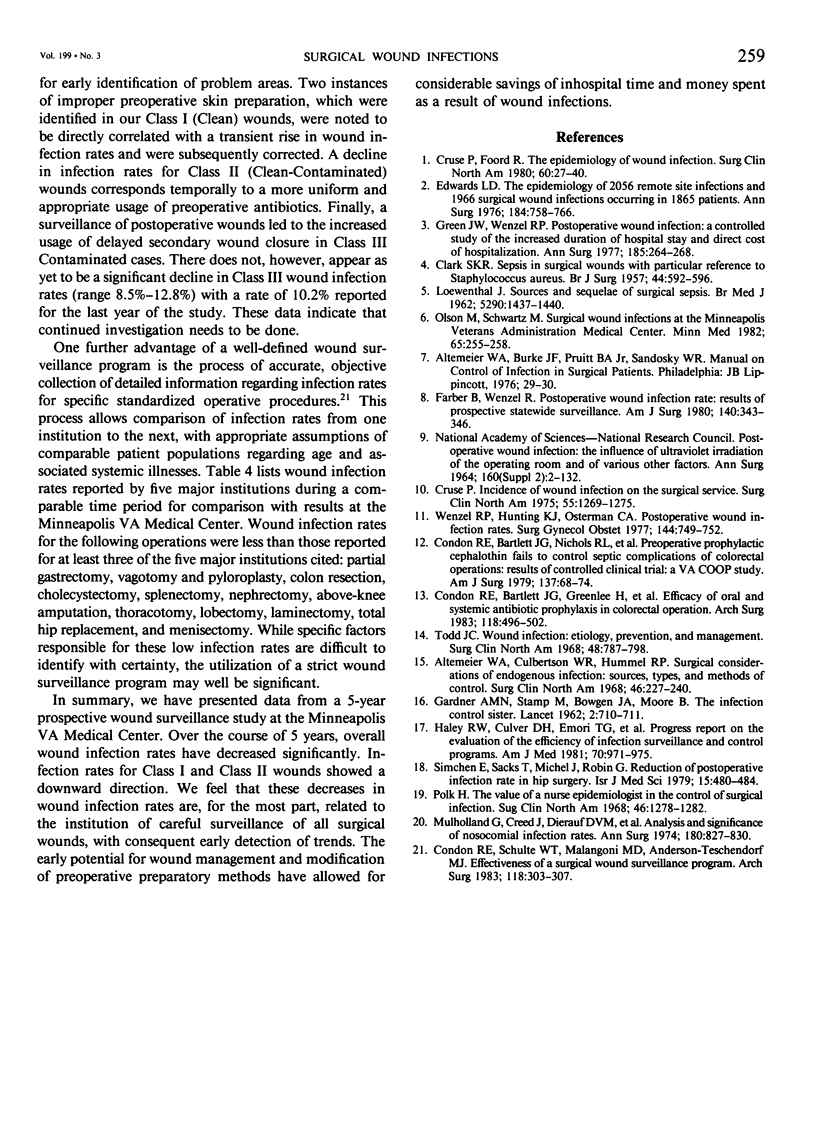
This report describes a 5-year prospective study of postoperative wound sepsis utilizing a careful program of wound surveillance. Surgical wounds following 20,193 operations on all surgical services were surveyed by a trained nurse epidemiologist. Daily examination of wounds, culture of all suspicious wounds, and 30-day outpatient clinic follow-up were performed. Results were disseminated at monthly intervals to all involved surgeons and operating room personnel. Prospective and ongoing analysis of results facilitated identification and rectification of specific problem areas. Wound infection rates demonstrated a steady decline over the course of the study, overall rates dropping from 4.2% to 1.9% (p less than 0.05). This reduction in incidence of postoperative wound sepsis of 55% is estimated to have saved 2740 inhospital days and nearly $750,000.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altemeier W. A., Culbertson W. R., Hummel R. P. Surgical considerations of endogenous infections--sources, types, and methods of control. Surg Clin North Am. 1968 Feb;48(1):227–240. doi: 10.1016/s0039-6109(16)38448-1. [DOI] [PubMed] [Google Scholar]
- CLARKE S. K. Sepsis in surgical wounds with particular reference to staphylococcus aureus. Br J Surg. 1957 May;44(188):592–596. doi: 10.1002/bjs.18004418809. [DOI] [PubMed] [Google Scholar]
- Condon R. E., Bartlett J. G., Greenlee H., Schulte W. J., Ochi S., Abbe R., Caruana J. A., Gordon H. E., Horsley J. S., Irvin G., 3rd Efficacy of oral and systemic antibiotic prophylaxis in colorectal operations. Arch Surg. 1983 Apr;118(4):496–502. doi: 10.1001/archsurg.1983.01390040100021. [DOI] [PubMed] [Google Scholar]
- Condon R. E., Bartlett J. G., Nichols R. L., Schulte W. J., Gorbach S. L., Ochi S. Preoperative prophylactic cephalothin fails to control septic complications of colorectal operations: results of controlled clinical trial. A Veterans Administration cooperative study. Am J Surg. 1979 Jan;137(1):68–74. doi: 10.1016/0002-9610(79)90013-8. [DOI] [PubMed] [Google Scholar]
- Condon R. E., Schulte W. J., Malangoni M. A., Anderson-Teschendorf M. J. Effectiveness of a surgical wound surveillance program. Arch Surg. 1983 Mar;118(3):303–307. doi: 10.1001/archsurg.1983.01390030035006. [DOI] [PubMed] [Google Scholar]
- Cruse P. J., Foord R. The epidemiology of wound infection. A 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980 Feb;60(1):27–40. doi: 10.1016/s0039-6109(16)42031-1. [DOI] [PubMed] [Google Scholar]
- Cruse P. J. Incidence of wound infection on the surgical services. Surg Clin North Am. 1975 Dec;55(6):1269–1275. doi: 10.1016/s0039-6109(16)40780-2. [DOI] [PubMed] [Google Scholar]
- Edwards L. D. The epidemiology of 2056 remote site infections and 1966 surgical wound infections occurring in 1865 patients: a four year study of 40,923 operations at Rush-Presbyterian-St. Luke's Hospital, Chicago. Ann Surg. 1976 Dec;184(6):758–766. doi: 10.1097/00000658-197612000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber B. F., Wenzel R. P. Postoperative wound infection rates: results of prospective statewide surveillance. Am J Surg. 1980 Sep;140(3):343–346. doi: 10.1016/0002-9610(80)90164-6. [DOI] [PubMed] [Google Scholar]
- GARDNER A. M., STAMP M., BOWGEN J. A., MOORE B. The infection control sister. A new member of the control of infection team in general hospitals. Lancet. 1962 Oct 6;2(7258):710–711. doi: 10.1016/s0140-6736(62)90520-2. [DOI] [PubMed] [Google Scholar]
- Green J. W., Wenzel R. P. Postoperative wound infection: a controlled study of the increased duration of hospital stay and direct cost of hospitalization. Ann Surg. 1977 Mar;185(3):264–268. doi: 10.1097/00000658-197703000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley R. W., Culver D. H., Emori T. G., Hooton T. M., White J. W. Progress report on the evaluation of the efficacy of infection surveillance and control programs. Am J Med. 1981 Apr;70(4):971–975. doi: 10.1016/0002-9343(81)90563-5. [DOI] [PubMed] [Google Scholar]
- LOEWENTHAL J. Sources and sequelae of surgical sepsis. Br Med J. 1962 May 26;1(5290):1437–1440. doi: 10.1136/bmj.1.5290.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulholland S. G., Creed J., Dierauf L. A., Bruun J. N., Blakemore W. S. Analysis and significance of nosocomial infection rates. Ann Surg. 1974 Dec;180(6):827–830. doi: 10.1097/00000658-197412000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson M., Schwartz M. L. Surgical wound infections at the Minneapolis Veterans Administration Medical Center. Minn Med. 1982 Apr;65(4):255–258. [PubMed] [Google Scholar]
- Simchen E., Sacks T., Michel J., Robin G. Reduction of postoperative infection rate in hip surgery: collaborative effort between orthopedic surgeons and control-of-infection team. Isr J Med Sci. 1979 Jun;15(6):480–484. [PubMed] [Google Scholar]
- Todd J. C. Wound infection: etiology, prevention, and management, including selection of antibiotics. Surg Clin North Am. 1968 Aug;48(4):787–798. doi: 10.1016/s0039-6109(16)38582-6. [DOI] [PubMed] [Google Scholar]
- Wenzel R. P., Hunting K. J., Osterman C. A. Postoperative wound infection rates. Surg Gynecol Obstet. 1977 May;144(5):749–752. [PubMed] [Google Scholar]


