Abstract
Objective:
Our goal was to evaluate the clinical reliability of a new software system employing 3-dimensional (3D) virtual anatomic reconstruction and intraluminal virtual exploration for detection of choledocholithiasis and preoperative visualization of the biliary anatomy.
Summary Background Data:
Virtual reality systems have been proposed for gastroscopy, bronchoscopy, and colonoscopy, as well as for the 3D reconstruction of liver anatomy and hepatic lesions. The impact of these systems in preoperative diagnostics has not been established due to the lack of large clinical series evaluating their reliability.
Methods:
From November 2000 to July 2002, all patients presenting to our Institute with suspected choledocholithiasis were prospectively included in the study. All patients underwent conventional magnetic resonance cholangiopancreatography (MRCP) and either intraoperative cholangiogram (IOC) or endoscopic retrograde cholangiopancreatography (ERCP). The digital data from MRCP were incorporated into an original virtual reality software system to generate a 3D reconstruction. All 3D reconstructions were evaluated by a surgeon and a computer software engineer who were blind to the results of the IOC or ERCP. Sensitivity and specificity were then calculated based on the results of either the IOC or ERCP.
Results:
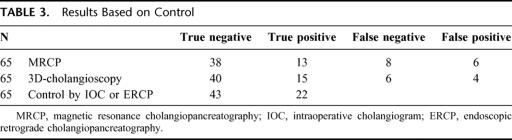
Sixty-five patients were enrolled in the study. The average time required to reconstruct the images into navigable virtual reality was 7.5 minutes (range, 4–13.5). The 3D virtual cholangioscopy had sensitivity and specificity rates of 71% and 91%, respectively, compared with 61% and 86% of the standard MRCP.
Conclusion:
The 3D virtual cholangioscopy provides detailed preoperative reconstruction of biliary anatomy and reliable identification of choledocholithiasis with acceptable sensitivity and specificity in a clinical setting. Newer software developments may further enhance its accuracy, so that virtual cholangioscopy might challenge or replace more invasive diagnostic measures in the near future.
Virtual reality and computer technologies have potential impact on preoperative diagnosis and surgical planning. We used a software developed at the European Institute of Telesurgery for obtaining 3-dimensional reconstructions of the biliary system in patients with suspected choledocholithiasis. Our findings show that this 3-dimensional virtual cholangioscopy was clinically reliable and may be a valuable alternative for the non-invasive diagnostic management of stones and anatomic abnormalities of the biliary tract.
Tools for diagnosis of choledocholithiasis include ultrasound, endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography (IOC), cholangio-computerized tomography (CCT), and magnetic resonance cholangiopancreatography (MRCP)1–3. Magnetic resonance imaging (MRI) has been used since 1991 as a modality for the evaluation of the biliary/pancreatic system, and its advantages include high diagnostic power without the risk inherent to invasive procedures, such as ERCP or IOC.4–7 The interpretation of MR images, however, is limited by individual subjectivity and the ability of human vision to discriminate along a grayscale extending from pure white to pure black. The digitized data obtained with MRI is more extensive than simple visual interpretation on a monitor or a radiograph. Because of this, there is a possibility to lose a significant amount of potentially useful data.
To facilitate the detection of choledocholithiasis, improve preoperative visualization of the biliary anatomy, and attempt to increase the objectivity of MR data, we have developed a software package in our institute that automatically reconstructs the anatomy of the biliary tract and associated lesions based on the digital information and the full grayscale generated by MRI. This software creates a virtual reality environment where interactivity and navigation into the lumen are feasible, allowing the user to perform a 3-dimensional (3D) virtual cholangioscopy.8 Virtual reality systems have been proposed for gastroscopy, bronchoscopy, and colonoscopy, as well as for 3D reconstruction of liver anatomy and hepatic lesions.9 However, the impact of these systems in preoperative diagnostics is not established due to the lack of large clinical series evaluating their reliability compared with conventional methods. Because this software has been generated at our Institute, it had no previous clinical validation for efficacy as a diagnostic tool. This study was designed to evaluate the feasibility of clinical application of this software.
MATERIALS AND METHODS
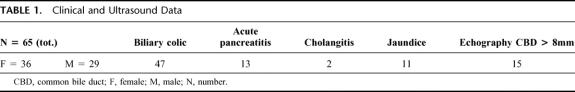
All patients presenting to the Department of Digestive and Endocrine Surgery of the University Hospital of Strasbourg France, with suspected choledocholithiasis were prospectively included in our study. The criteria used for definition of suspected choledocholithiasis were based on clinical parameters (acute pancreatitis, acute cholangitis, or jaundice), laboratory parameters (elevated: bilirubin, amylase, alkaline phosphatase, transaminases, or lipase), and echography results (common bile duct >8 mm in diameter).
All recruited patients underwent preoperative MRCP and either ERCP/sphincterotomy or IOC, in accordance with our institute's treatment policy. The policy of the institute is to perform IOC on patients younger than 70 years of age, and ERCP/sphincterotomy in patients 70 or older.
MR Protocol
MRCP was performed using a MR Philips unit (1.0 T gyroscan NT) employing an abdominal phased array coil with 4 elements. No medication or contrast medium was administered for the MR studies. For the first step in MR image acquisition, conventional T1- and T2-weighted spin echo sequences were generated in axial and coronal planes. MRCP was then performed with 2 types of fast spin echo sequences: a series of multiple, single-shot thick radial slices (TR/TE: 1800/500 ns, thickness 6cm) around the axis of the common bile duct (CBD), and a multislice 2-dimensional series (TR/TE: 1800/500 ns, thickness 0.6 mm) with MIP reconstruction in the coronal and oblique planes to simulate a right anterior oblique projection similar to standard cholangiography. Each study was performed in its entirety while the patient held his breath to reduce motion artifact.
Software Characteristics
Digital MR data obtained were elaborated by the software developed by the Virtual Surgery team at our institution, IRCAD/EITS (Institut Recherche Contre les Cancers de l'Appareil Digestif/European Institute of Telesurgery). The image processing was performed using an OCTANE II SGE Computer (Silicon Graphics computer, Mountain View, CA) with a RISC R1200 processor cadenced at 400 MHz and with 1 Gbyte of RAM. The 3D reconstruction starts from the improvement of the data obtained by the MRI. The software decreases the noise and enhances the contrast between the lithiasis (dark) and the biliary tract (white). This type of filtering, named anisotropic diffusion, is also used for automatic delineation of anatomical and pathological structures as described by Soler et al8 (Fig. 1). Next, the software performs an automatic thresholding among four values corresponding to four different degree of resolution of the biliary tract (Fig. 2). Finally, the software allows interactive virtual navigation outside and inside the biliary tree (Fig. 3).
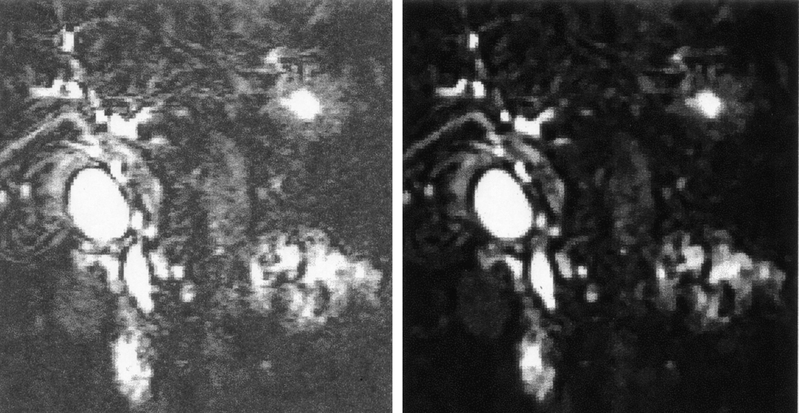
FIGURE 1. The anisotropic diffusion (right) reduces noise and increases contrast.
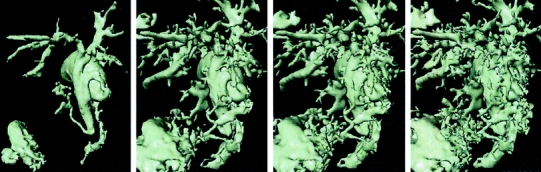
FIGURE 2. The software allows for automatic thresholding among 4 values corresponding to 4 different image resolution; the smaller the threshold, the more the details that are reconstructed. A smaller threshold is useful to identify smaller structure, but can render the figure more difficult to analyze. A larger threshold permits an easier visualization of the biliary tract, but the fine details necessary to detect stones can be lost.
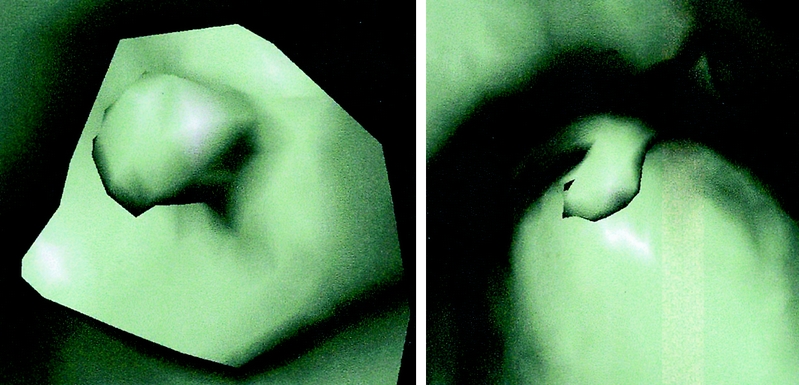
FIGURE 3. Detection of 2 stones in the CBD. The stone appears as a polyp.
From the 3D reconstruction stones can be detected through virtual cholangioscopy (Fig. 3) or through the analysis of the shape of the distal CBD (Fig. 4). Improvement of the analysis can be obtained by several tricks (Figs. 5–6), such as using superimposition, transparency and coloration.
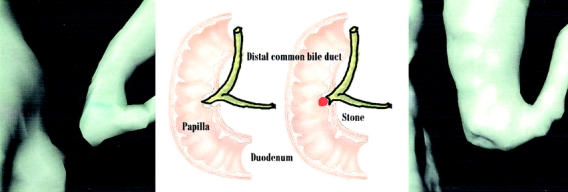
FIGURE 4. Normal (left) and pathological sphincter (right). Since MRI is less accurate for the analysis of the distal tract of CBD, the 3D reconstruction can make stone detection easier by enhancing the differences in shape of the distal tract of CBD.

FIGURE 5. The color can futher enhance detection of stones.
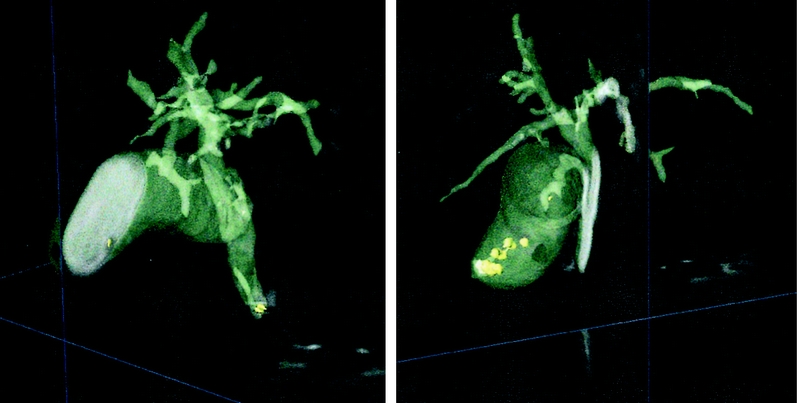
FIGURE 6. The combination and superimposition of conventional MRI onto the 3D reconstructions with transparency views also can facilitate visualization during stone detection and virtual navigation.
Patient and Image Protocol
All MR images were obtained by the on-call team of radiologists and final evaluation was performed by a single senior radiologist. IOC was performed by transcystic technique using a percutaneous cholangiography catheter with a rigid tip (Applied Medical-Rancho Santa Margarita, CA, Ref. C1002 3-20F). The ERCPs were performed by the same endoscopist. All 3D reconstructions were evaluated by a surgeon and a computer software engineer who were blind to the results of the IOC or ERCP. Sensitivity and specificity were then calculated for both the MRCP and the 3D virtual cholangioscopy, based on the results of either the IOC or ERCP, depending on which of these studies was employed. The sensitivity and specificity of the 2-dimensional images (MRCP) were then compared directly to the 3D images (virtual cholangioscopy).
RESULTS
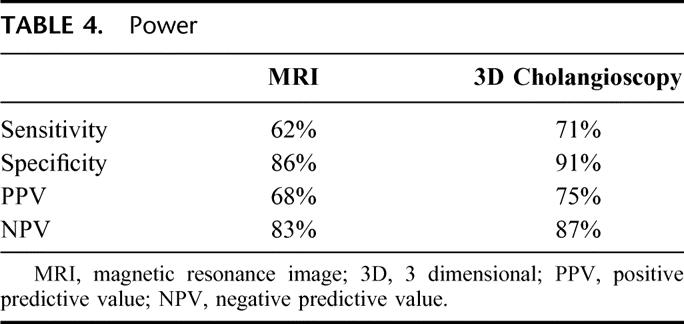
From November 2000 to July 2002, 65 patients were enrolled in the study. Clinical and ultrasonographic data are reported in Table 1; Table 2 describes treatment arm distribution. The average time required to reconstruct the images into navigable virtual reality was 7.5 minutes (range, 4–13.5 m). The virtual images generated by the software had a greater number of true negative and true positive results than standard MRCP, along with fewer false negative and false positive results (Table 3). This corresponded to a better sensitivity and specificity for the virtual images compared with MRCP, higher positive predictive value, and higher negative predictive value (Table 4).
TABLE 1. Clinical and Ultrasound Data
TABLE 2. Treatment Arm Distribution
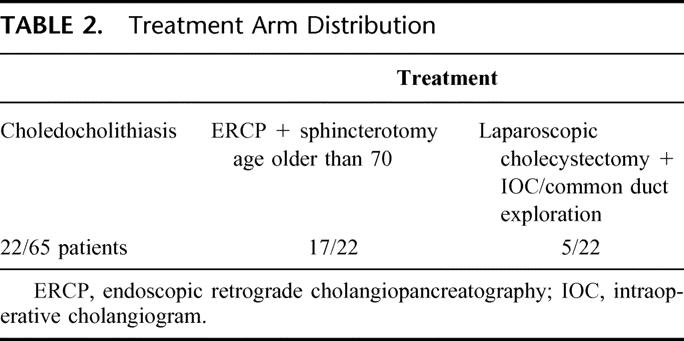
TABLE 3. Results Based on Control
TABLE 4. Power
DISCUSSION
The main goal of our study was to investigate the feasibility of the clinical application of 3D virtual cholangioscopy. A secondary goal was to evaluate the reliability of this system in performing rapid reconstructions of the common bile duct and identification of stones or anatomic abnormalities if present.
Our findings show that the automatic computer-based reconstruction was at least as efficient as the conventional MRI analysis, and approached IOC/ERCP, suggesting that 3D virtual cholangioscopy may be a valuable and reliable tool for the diagnosis of common bile duct stones. A specific advantage of our software was its expeditious generation of the images: 7.5 minutes on average.
This study has, admittedly, some clear limitations. The first is the relatively small number of patients, which, along with the infrequency of the incidence of the pathology precluded the possibility of achieving statistical significance for the observed superior sensitivity and specificity of 3D virtual cholangioscopy compared with MRI. We also recognize the low sensitivity of the standard MRI analysis performed in our study compared with the 85–95% sensitivity reported in the literature.5,10 This likely reflects the fact that, although the final images were all reviewed by a single senior radiologist, the reference was the initial data acquisition of the MRCP performed by the radiologist on call. This may account for the differences between our MRCP sensitivity compared with other specialized investigations, on the other hand, our results more likely reflect the use of MRCP in a daily setting.
This study design used ERCP and IOC as gold standard procedures. Whether we found no false-positives cases related to these procedures in this study, as all positive cases were confirmed by a successful extraction of stones, of course, no control for false negatives of IOC and ERCP was made at the time the procedure was performed. We could have considered as false negative any case in which the patient had presented with recurrent symptoms and with evidence of stones within a short period of time after the IOC or ERCP, but within the frame time of the present study there were no early recurrences.
Potential Clinical Interest of 3D Virtual Cholangioscopy
Diagnosis and management algorithms for choledocholithiasis remain controversial. Several management strategies, including laparoscopic cholecystectomy with laparoscopic common bile duct exploration, open approach to common bile duct exploration, pre, intra- or postoperative ERCP have all been proposed by different teams and no strategy so far has provided evidence-based proof for its acceptability as the strategy of choice. In addition, the possibility that small stones can migrate spontaneously and asymptomatically on one hand,11 and the morbidity and mortality associated with invasive diagnostic procedures on the other hand, stress the need for newer tools and/or strategies that could ensure both high diagnostic accuracy and reduced invasiveness. There is therefore an objective clinical interest for virtual cholangioscopy due to its potential to obtain high diagnostic accuracy without being invasive.
Currently, numerous efforts to define precise predictive criteria for the presence of common bile duct stones are frequently hampered by methodological pitfalls. Preoperatively, surgeons have to cope with choices among clinical history, transabdominal ultrasonography, endoscopic ultrasonography, CT and MRCP, and all of these modalities carry a failure rate between 5 and 10%.12 Performing systematic preoperative ERCP has not gained wide acceptance as it is associated with a morbidity and mortality rate from 3 to 6.4% and 0.2 to 0.8%, respectively10, with specific severe complications including pancreatitis and perforation. Additionally, ultrasound, CT, and MRI are purely diagnostic, whereas ERCP offers the opportunity for a therapeutic intervention if needed. Many teams perform routine IOC, but since the advent of laparoscopy up to 89% of IOCs have been associated with errors in performance13or interpretation, and up to 30% of films were shown to be inadequate to render a diagnosis, leading to a mean false positive rate between 2 and 19%, and a false negative rate of 2 to 3%.10,14 Therefore, systematic IOC still remains controversial. Its principle benefit seems to lie in the identification of common bile duct injury rather than the 5–10% incidence of identification of unsuspected common bile duct stones.15
Many authors have proposed preoperative MRCP as an alternative strategy for detecting the presence of choledocholithiasis. The sensitivity and specificity of MRI have been reported to be 88.9% and 100%, respectively10; however, much of the potential of MR imaging is lost because of limited interpretation of the grayscale. Theoretically, more than 2000 different shades of gray from pure white to pure black are generated with MR imaging, each corresponding to a specific digital value16,17. In practice, however, the number of shades of gray that the human eye can distinguish on a monitor or a radiographic film does not exceed 16,18–20 thus the basis of interpretation by a radiologist is limited by the biology of human vision. Hence, a large amount of potentially useful information is not considered.
The software developed at our institute is able to incorporate all of the digital “grays” generated by MRI to automatically detect polyps, stones or abnormalities of the duct. The data are analyzed to distinguish noise or artifact from usable data through a filtering system called anisotropic diffusion.21 The software performs automatic thresholding, which in turn allows for a completely automated reconstruction of the biliary tree and hepatic structures8. From this perspective, the 3D reconstructions seem to have an advantage over conventional imaging, and, indeed, our prospective results support this idea as evidenced by the higher sensitivity we found with the 3D reconstructions.
Virtual reality reconstructions have, admittedly, some limitations. The most important disadvantage is that they are still based on the original data of the MRI and therefore, despite improvement in data analysis performed by the software, the limitations of MRCP in detection of stones less than 5 millimeters or stones present in the last portion of the CBD over the papillary sphincter remain restrictions even with 3D reconstruction. A stone located in the terminal 5 millimeters of the common bile duct is the most difficult to identify.22–24 Likewise, a CBD less than 3 millimeters in diameter, presence of a short stenosis or aerobilia may lead to difficult identification. In this study, in 3 cases of false negative results of MRCP, 3D cholangioscopy suggested instead the presence of a choledocholithiasis. In all these patients, the stones were located at the 3rd inferior part of the CBD; in all these 3 patients also, IOC and/or ERCP confirmed the findings of the 3D and also resulted in successful stones extraction. The size varied between 1.5 cm in 2 cases to less than 0.5 mm in the other. These findings confirms the reported higher degree of failure in detecting stones of most inferior part of the CBD when using MRCP; a lower efficacy in the last third of the CMD is also a possible drawback of our 3D cholangioscopy, as the reconstruction depends on data acquired through the MRCP. This is also suggested by the present findings that all false negatives in 3D virtual cholangioscopy occurred in patients with stones of the inferior third of the CBD. On the other hand, the 3D cholangioscopy had less false negatives than MRCP and detected even stones smaller than 0.5 mm (which were instead missed at the MRCP), thus suggesting that the virtual cholangioscopy may improve outcomes of MRCP, and approach accuracy of more invasive methods.
Furthermore, the need for a routine performance of MRI could be criticized for being both expensive and an over-utilization of available resources. In fact, the hospital charges for an MRI have been reported from $361 in France,25 where this study was conducted, to $1145 in the United States.26 Although routine MRI may be too expensive to justify, selected performance of MRI with biliary tree reconstruction may gain legitimacy when weighed against the relative cost of a biliary tree injury during a cholecystectomy, which has been reported to be a mean value of $51,411,27 and mean legal costs at $507,000.28 If using 3D reconstructions could prevent even a small number of biliary tract injuries by preoperative identification of anatomic abnormalities, it may turn out to be actually cost-effective. The rationale advocated by centers that practice routine IOC is often that IOC provides information regarding potential anatomic hazards which may subsequently prevent a biliary tract injury, which has been reported to affect around 2000 patients annually in the United States.29 Centers that do not practice routine IOC may argue that these injuries are often associated with the performance of the IOC itself, and the study therefore only serves to identify the injury.15 If a virtual cholangioscopy based on MRI could eliminate the need for routine use of an invasive procedure, and thereby decrease the incidence of biliary tract injuries, one may see a very large decrease in costs. Indeed, the problem of cost related to the implementation of all new technologies may seem discouraging at first glance, but a more comprehensive evaluation of the possible clinical advantages may reveal them to be an opportunity for cost-saving.
Specific Advantages of MR-Based 3D Virtual Reality Reconstructions
An important feature of virtual reality technology is that the software generates a very accurate 3D reconstruction and avoids subjective human interpretation. The software can make stone detection easier by making the differences in shape of the distal duct in normal versus abnormal situations more apparent. Furthermore, the combination and superimposition of conventional MR images on the 3D reconstruction with transparency views can also facilitate the visualization during stone detection and virtual navigation. Benefits of using MR versus CT for data acquisition include its lack of ionizing radiation and lack of injected contrast material, which thereby eliminates the potential morbidity and mortality caused by allergic reactions.8,22,23
An inherent advantage of using virtual reality is that the reconstruction is not just a better image but a real 3D virtual representation. This means that one is able to become immersed in the image, navigate through the system, and interact with the image. In the near future, interaction with the image will likely enable performance of virtual common bile duct surgery on actual patient data.
The software is able to generate the images much faster than conventional interpretation without concerns about the quality of the radiologist's interpretation. An image that is reconstructed with a high-speed computer can be realized in a few minutes and transmitted to the operating team. Although the generation of the reconstructions requires a high-speed computer, the reconstructions themselves can be displayed and manipulated on a typical laptop computer, which can also be brought to the operating room. Abnormalities should be easily identified by the operating surgeon, thus potentially reducing or eliminating the need for IOC, as well as facilitating the management of choledocholithiasis.
The ease of transmission of digital data to the OR team or any other team in any location for consultation or collaboration almost immediately via the Internet is an additional advantage. We have demonstrated in a previous study the importance of tele-transmission of data for tele-teaching, tele-training and tele-mentoring.30 The digitization of the data can allow incorporation of prototypical cases into simulation models for virtual surgical training.31,32
Finally, using virtual reality systems opens new avenues for the future of surgery and medicine in general. Using these systems, one can imagine that teleconsultation and collaboration for difficult cases will be facilitated. Furthermore, virtual and augmented reality systems can be used not only to teach surgical skills and judgement or to facilitate intraoperative maneuvers, but also to rehearse procedures before performing them. With more perfected surgical simulators, in the near future, surgeons may work out the best operative procedure for each single patient and be able to repeat individual steps to improve surgical technique. The procedures could also be recorded and replayed from a robot automatically and at a distance.
CONCLUSIONS
Our study shows the feasibility of applying 3D virtual reality reconstructions of the biliary system in a clinical setting. Virtual cholangioscopy may be a valuable tool for the preoperative diagnosis of choledocholithiasis and anatomic anomalies of the biliary tree. Future advances in computer technology will certainly improve virtual reality systems and perhaps decrease the need for potentially dangerous invasive procedures.
Footnotes
Reprints: Prof Jacques Marescaux, MD, IRCAD/EITS, 1 Place de l'Hopital, 67091 Strasbourg, France. E-mail: Jacques.Marescaux@ircad.u-strasbg.fr.
REFERENCES
- 1.Millat B, Borie F. Common bile duct stones and their complications. Rev Prat. 2000;50:2123–2129. [PubMed] [Google Scholar]
- 2.Hugier M. Prospective analysis of a scoring system to predict choledocholithiasis (Br J Surg 2000;87:1176–1181). Br J Surg. 2001;88:314–315. [DOI] [PubMed] [Google Scholar]
- 3.Lincender L, Sadagic E, Vrcic D, et al. Magnetic resonance cholangiography in patients with bile duct obstruction. Radiol Oncol. 2000;34:319–324. [Google Scholar]
- 4.Kyoung KT, Soo KB, Kwon HH, et al. Diagnosis of intrahepatic stones: Superiority of MR cholangiopancreatography over endoscopic retrograde cholangiopancreatography. AJR. 2002;179:429–434. [DOI] [PubMed] [Google Scholar]
- 5.Laokpessi A, Bouillet P, Sautereau D, et al. Value of magnetic resonance cholangiography in the preoperative diagnosis of common bile duct stones. Am J Gastroenterol. 2001;96:2354–2359. [DOI] [PubMed] [Google Scholar]
- 6.Pelletier G. Gallstones and their complications. Rev Prat. 2002;52:427–433. [PubMed] [Google Scholar]
- 7.Boytchev I, Pelletier G, Prat F, et al. Late biliary complications after endoscopic sphincterotomy for common bile duct stones in patients older than 65 years of age with gallbladder in situ. Gastroenterol Clin Biol. 2000;24:995–1000. [PubMed] [Google Scholar]
- 8.Soler L, Delingette H, Malandain G, et al. Fully automatic anatomical, pathological, and functional segmentation from CT scans for hepatic surgery. Com Aid Surg 2001;6:131–142. [DOI] [PubMed] [Google Scholar]
- 9.Rubino F, Soler L, Marescaux J, et al. Advances in virtual reality are wide ranging. BMJ 2002;324:612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tham TC, Lichtenstein DR, Vandervoort J, et al. Role of endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in patients undergoing laparoscopic cholecystectomy. Gastrointest Endosc. 1998;47:50–56. [DOI] [PubMed] [Google Scholar]
- 11.Yamakawa T, Sakai S, Mu ZB, et al. Laparoscopic management of common bile duct stones. J Hepatobiliary Pancreat Surg. 2000;7:9–14. [DOI] [PubMed] [Google Scholar]
- 12.Prat F, Meduri B, Ducot B, et al. Prediction of common bile duct stones by noninvasive tests. Ann Surg. 1999;229:362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohtani T, Kawai C, Shirai Y, et al. Intraoperative ultrasonography versus cholangiography during laparoscopic cholecystectomy: a prospective comparative study. J Am Coll Surg. 1997;185:274–282. [DOI] [PubMed] [Google Scholar]
- 14.Cotton PB, Baillie J, Pappas TN, et al. Laparoscopic cholecystectomy and the biliary endoscopist [Editorial]. Gastrointest Endosc. 1991;37:94–96. [DOI] [PubMed] [Google Scholar]
- 15.Falcone RA Jr, Fegelman EJ, Nussbaum MS, et al. A prospective comparison of laparoscopic ultrasound vs intraoperative cholangiogram during laparoscopic cholecystectomy. Surg Endosc. 1999;13:784–788. [DOI] [PubMed] [Google Scholar]
- 16.Sodickson DK, McKenzie CA, Ohliger MA, et al. Recent advances in image reconstruction, coil sensitivity calibration, and coil array design for SMASH and generalized parallel MRI. MAGMA. 2002;13:158–163. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y. Description of parallel imaging in MRI using multiple coils. Magn Reson Med. 2000;44:495–499. [DOI] [PubMed] [Google Scholar]
- 18.Dwyer SJ III, Stewart BK, Sayre JW, et al. Performance characteristics and image fidelity of gray scale monitors. Radiographics. 1992;12:765–772. [DOI] [PubMed] [Google Scholar]
- 19.Hangiandreou NJ, Fetterly KA, Felmlee JP. Optimisation of contrast detail based method for electronic image display quality evaluation. J Digit Imaging. 1999;12:60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hess RF, Liu CH, Wang YZ. Luminance spatial scale and local stereo-sensivity. Vision Res. 2002;42:331–342. [DOI] [PubMed] [Google Scholar]
- 21.Krissian K, Malandain G, Ayache N. Directional anisotropic diffusion applied to segmentation of vessels in 3D images. INRIA France, RR-3064 (1996).
- 22.Cannard L, Leclerc JC, DeBelle L, et al. Exploration de la patologie de l'ampoule de Vater en cholangio IRM. Feuillets de Radiol. 2001;41:215–222. [Google Scholar]
- 23.Vasilescu C, Filippi della Palavesa M, Coumaros D, et al. Cholangite sclerosante primitive: rôle de la cholangio-pancreatographie par IRM. Feuillets de Radiol. 2001;41:340–347. [Google Scholar]
- 24.Atkinson D, Hill DLG, Stoyle PNR, et al. Automatic compensation of motion artifacts in MRI. Magn Reson Med. 1999;41:163–170. [DOI] [PubMed] [Google Scholar]
- 25.Burtin P. Cost-effectiveness of various diagnostic and therapeutic approaches to lithiasis of the common bile duct. Gastroenterol Clin Biol. 1998;22(5 Suppl):B30–B38. [PubMed] [Google Scholar]
- 26.Scheiman JM, Carlos RC, Barnett JL, et al. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? A prospective trial and cost analysis. Am J Gastroenterol. 2001;96:2900–2904. [DOI] [PubMed] [Google Scholar]
- 27.Savader SJ, Lillemoe KD, Prescott CA, et al. Laparoscopic cholecystectomy-related bile duct injuries: a health and financial disaster. Ann Surg. 1997;225:268–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kern KA. Malpractice litigation involving laparoscopic cholecystectomy. Cost, cause, and consequences. Arch Surg 1997;132:392–397; discussion 397–398. [DOI] [PubMed]
- 29.Hugh TB. New strategies to prevent laparoscopic bile duct injury–surgeons can learn from pilots. Surgery. 2002;132:826–835. [DOI] [PubMed] [Google Scholar]
- 30.Demartines N, Mutter D, Vix M, et al. Assessment of telemedicine in surgical education and patient care. Ann Surg. 2000;231:282–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Docuo Le pointe H. Teleradiology. Biomed Pharm. 1998;52:64–68. [DOI] [PubMed] [Google Scholar]
- 32.Gallagher AG, Richie K, McClure N, et al. Objective psychomotor skills assessment of experienced, junior, and novice laparoscopists with virtual reality. World J Surg. 2001;25:1478–1483. [DOI] [PubMed] [Google Scholar]