Abstract
Objective:
To compare technical aspects and postoperative outcomes of laparoscopic left colectomy in obese and nonobese patients.
Summary Background Data:
Obesity has been generally associated with increased surgical risk. The data regarding outcomes after laparoscopic colectomy in obese and nonobese patients are limited and quite controversial; however, most reports have suggested that obesity is associated with a greater technical difficulty as well as an increased risk for conversions and postoperative complications.
Methods:
All patients undergoing laparoscopic left colectomy for any pathologic condition between January 2001 and January 2003 were analyzed. Patients with a body mass index (BMI) above 30 kg/m2 were defined as obese and patients with BMI below 30 kg/m2 were defined as nonobese. Data collected included age, gender, BMI, American Society of Anesthesiologists score, diagnosis, technical parameters of the procedure, operative time, conversion, pathology, length of hospital stay, and complications over a 30-day postoperative course.
Results:
A total of 123 patients underwent elective laparoscopic left colectomy during the 2-year period. Twelve patients were excluded from analysis because missing data did not allow calculation of their BMI. Of the 111 patients analyzed, 23 (20.7%) were obese and 88 patients (79.3%) were nonobese. Patients’ preoperative clinical characteristics were similar in obese and nonobese patients except for BMI (P > 0.001). There were no significant differences between the 2 groups with respect to intraoperative parameters, duration of the operation, resection margin, and number of harvested nodes as well as overall postoperative complication rates. There were no conversions in the obese patients, whereas 5 procedures in the nonobese group required conversion to open surgery (P = not significant). Obese patients had shorter hospital stays than nonobese subjects (7 ± 2.5 days vs. 9.5 ± 7 days; P = 0.018).
Conclusion:
In contrast with previously reported series of laparoscopic colectomy, our findings show that obesity does not have an adverse impact on the technical difficulty and postoperative outcomes of laparoscopic left colectomy. Our study supports the safety of using laparoscopic surgery for colorectal diseases in obese patients.
In contrast with previously reported series of laparoscopic colon surgery, the present study shows that obesity does not have an adverse impact on the technical difficulty and postoperative outcomes of laparoscopic left colectomy. These findings support the safety of using laparoscopic surgery for colorectal diseases in obese patients.
Obesity, whose incidence is growing at epidemic rates in Western countries, has been considered a risk factor for complications in general surgery;1,2 however recent reports seem to challenge this long-held opinion.3
With the advent of minimally invasive techniques, we have seen operative risks fall for all patients, including those with class III obesity (body mass index [BMI] >40 kg/m2).4 However, the impact of obesity on the outcomes of laparoscopic colectomy is still a controversial matter. Indeed, whether some suggested that laparoscopic colectomy for sigmoid diverticulitis can be performed safely in overweight and obese patients,5 most surgeons have consistently reported higher rates of conversion to open surgery, and a greater risk for leak and overall complications in the obese population compared with lean subjects.6–8 The laparoscopic approach for colonic surgery in obese patients is also generally deemed as more technically demanding than in the nonobese, and some have even regarded obesity as a relative contraindication for laparoscopic colorectal resections.7,9,10
Left colon resections are the most frequent procedures performed in laparoscopic colorectal surgery.9,11 We have specifically analyzed the most recent experience with laparoscopic left colectomy at our institution with the aim to investigate the specific impact of obesity on the technical aspects and postoperative outcomes of this procedure. By limiting the investigation only to left colonic resections, we meant to avoid a possible influence by a different degree of technical standardization across less frequently performed types of resections.
MATERIALS AND METHODS
Patients
A database including all patients undergoing laparoscopic colorectal surgery between January 2001 and January 2003 was used for our retrospective analysis. Inclusion criteria took in all laparoscopic segmental left colectomies for any pathologic condition, including cancer. Criteria for exclusion from analysis were: emergency operations, right colectomy, medium and low rectal surgery, reoperations, endometriosis, and rectopexy.
Obesity was defined by a BMI value equal or higher than 30 kg/m2.
Data Collection
Preoperative clinical characteristics (age, gender, BMI, American Society of Anesthesiologists [ASA] score, previous abdominal surgery, diagnosis), intraoperative data (technique for creation of pneumoperitoneum, port number, site of vessel division, splenic flexure mobilization, conversion, operative time, technical difficulties), pathology (final diagnosis, length of resected colon segment after fixation, and, in case of colorectal carcinoma, pTNM status, margins, and node number), and 30-day postoperative course (hospitalization time, time for first flatus, complications, need for intensive-care unit, reintervention, mortality) were assessed. Complications were defined as any event that required specific medical or surgical treatment. Ileus was defined as prolongation of the time between surgery and first flatus for more than 3 days.
Surgical Procedure
In our institution, laparoscopic left colonic resections have become highly standardized12 procedures and are performed by a senior surgeon (with a personal experience of more than 1000 laparoscopic colorectal resections) or by junior surgeons under tutorial assistance by the senior surgeon. Before surgery, all patients undergo a standard bowel preparation (orthograde bowel lavage) 48 hours before the operation and receive perioperative single-shot antibiotics.
The pneumoperitoneum is most commonly induced by performing an open supraumbilical incision or, less commonly, blindly, using the Veress needle. The pneumoperitoneum is always maintained at an insufflation pressure of 12 mm Hg. For a left colectomy, 5 to 6 ports are used. A key step of the procedure is the exposure of the left mesocolon by appropriate retraction of the small bowel loops in the right upper quadrants of the abdomen. This maneuver is facilitated by placing the patient in a right lateral tilt and a slight (15°) Trendelenburg position. A medial-to-lateral approach to the inferior mesenteric vessels and left (meso)colon is systematically performed. Vessels division can be proximal (on the origin of the inferior mesenteric artery or after the origin of the left colic artery) or distal (preserving the superior rectal vessels) as appropriate for the disease. The rectum is transected intracorporeally by 1, or more commonly 2, applications of a linear cutting stapler. The proximal colon transection is obtained by using a linear cutting stapler and is performed either intracorporeally, like in the case of colon cancer, or extracorporeally after pulling the colon through a suprapubic incision, like in the case of diverticular disease. The splenic flexure is mobilized when required (complete release of parietal, gastroepiploic and pancreatic splenic flexure attachments). The specimen is extracted through a mini-Pfannenstiel incision (3–4 cm), which is obtained by enlarging the original 5-mm suprapubic port-site incision. To avoid contamination, a wound protector is used in all cases. In case of cancer, to prevent tumoral cell's spillage, the specimen is put in an impermeable bag before extraction, thus providing double protection (endobag and wound protector device).
The preparation of the proximal segment for stapled colorectal anastomosis is performed extracorporeally. Finally, after reestablishing the pneumoperitoneum, laparoscopic end-to-end stapled colorectal anastomosis is performed with a Knight-Griffen technique using a 34-mm circular stapler introduced through the anus by the assistant. No drainage is generally placed at the end of intervention. The nasogastric tube and urinary catheter are removed within 24 hours after surgery.
Statistical Analysis
Data are expressed as mean ± standard deviation (SD). The SPSS 9.0 statistical software package (SPSS Inc., Chicago, IL) was used for the descriptive statistics and univariate analysis. To evaluate the impact of obesity on operative results and postoperative course, chi-squared, Fisher tests and Student t test were performed when appropriate. Because the etiology of colonic disease is a potential confounding factor influencing significantly both the operative procedure and postoperative course, comparisons were performed either among the whole population or after sample stratification according to the indication for resection. A P value <0.05 was considered significant.
RESULTS
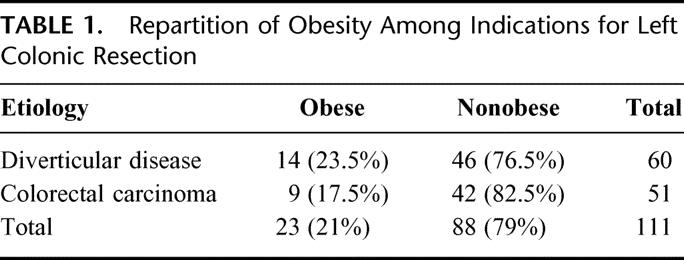
During the 2 years of the study, 123 patients underwent laparoscopic left colon resections. Sixty-six patients were operated for symptomatic diverticular disease (53.5%) and 57 for colorectal carcinoma (46.5%). The laparoscopic approach was converted to an open procedure in 5 cases (4.1%). Converted patients were included in the analysis. Ten patients presented postoperative complications (9%). No death was observed. BMI data was available for 111 patients. Among them, there were 23 patients (20.7%) with a BMI >30 kg/m2 and 88 patients (79.3%) with a BMI <30 kg/m2. Table 1 shows the repartition of obesity according to the indication for left colon resections.
TABLE 1. Repartition of Obesity Among Indications for Left Colonic Resection
Clinical Characteristics
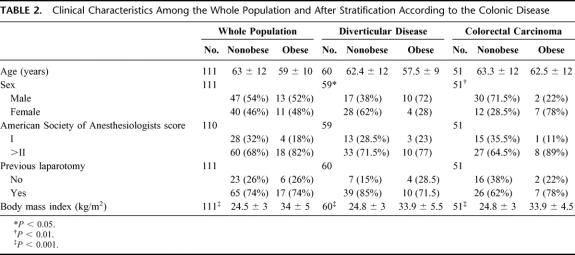
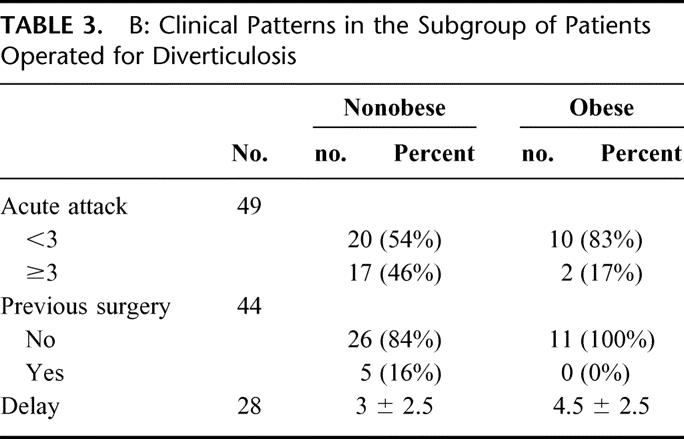
Patients’ preoperative clinical characteristics were similar in obese and nonobese patients except for BMI (P > 0.001; Table 2). After stratification, obesity appeared to be related to the patient's gender in both subgroups. In the subgroup of patients operated for diverticular disease, obesity was more frequent in men than in women (72% vs. 28%; P = 0.027). Conversely, in the subgroup of patients operated for colorectal cancer (CRC), obesity was more frequent in women than in men (78% vs. 22%; P = 0.009). Mean patient age, ASA score, and previous laparotomy were not related to obesity, even after stratification (Table 2). In the subgroup of patients operated for CRC, final diagnosis also disclosed similar repartition of pTNM between obese and nonobese patients (Table 3).
TABLE 2. Clinical Characteristics Among the Whole Population and After Stratification According to the Colonic Disease
TABLE 3. A: Repartition of pTNM in the Subgroup of Patients Operated for Colorectal Carcinoma
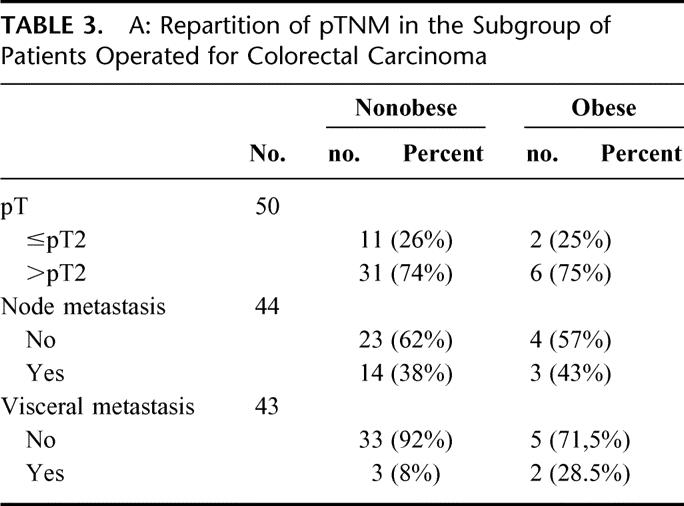
TABLE 3. B: Clinical Patterns in the Subgroup of Patients Operated for Diverticulosis
Surgical Procedure
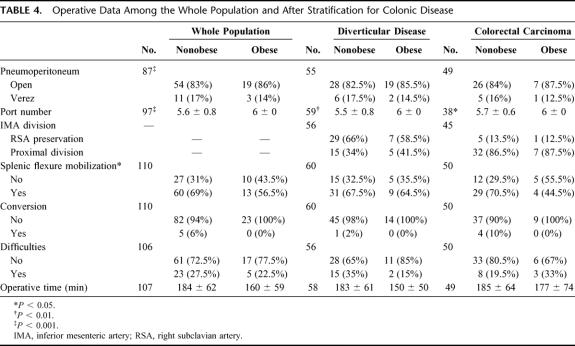
No significant difference among operative data were observed between obese and nonobese patients (Table 4). Supra umbilical minilaparotomy was used to create the pneumoperitoneum in most patients, either obese and nonobese. The superior rectal vessels were preserved in the majority of patients treated for diverticular disease, whereas proximal inferior mesenteric artery division was realized in all patients treated for CRC. Data analysis showed that the level of vessel's division was not related to obesity. Splenic flexure mobilization was also performed in the majority of cases and in a similar proportion of obese and nonobese patients.
TABLE 4. Operative Data Among the Whole Population and After Stratification for Colonic Disease
Five patients (4.5%), all of them in the nonobese group, were converted to open surgery: 4 of them had advanced CRC (pT3 or pT4) and 1 had diverticular disease. The reason for conversion was postsurgical adhesions in 4 cases and ureterolysis in 1 case. Finally, the mean operative time (considering all indications) was shorter in the group of obese patients, for all kind of indications, although this difference did not reach statistical significance.
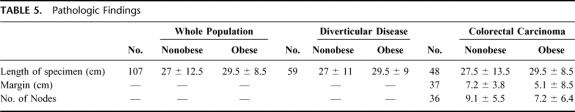
Pathologic Results (Table 5)
TABLE 5. Pathologic Findings
After fixation, the length of the resected colon was similar in obese and nonobese patients for all the indications. For patients with cancer, the resection margin and number of harvested nodes were also similar in obese and nonobese patients.
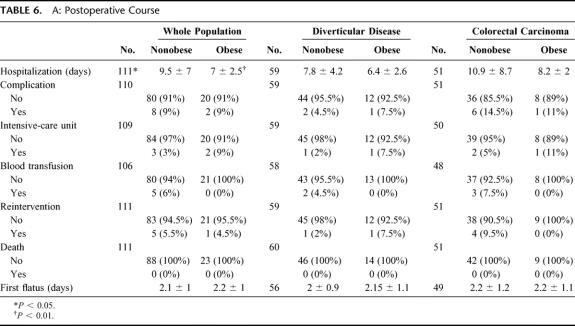
Postoperative Course
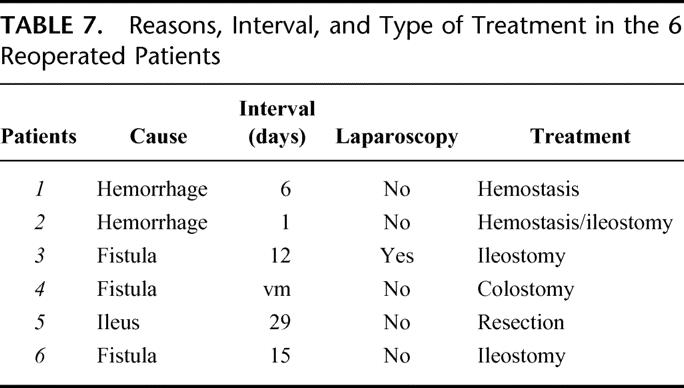
The length of hospitalization was shorter in obese patients compared with the nonobese (7 ± 2.5 vs. 9.5 ± 7, P = 0.018) (Tables 6 and 7). All other postoperative parameters did not significantly differ between obese and nonobese patients for all types of surgical indications. Noteworthy, the patients in the obese group did not need blood transfusions and did not develop leaks (leak rate in the nonobese group was 3.5%; P = not significant).
TABLE 6. A: Postoperative Course
TABLE 6. B: Postoperative Complications
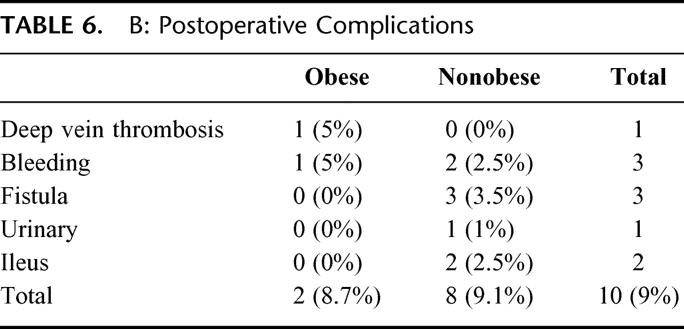
TABLE 7. Reasons, Interval, and Type of Treatment in the 6 Reoperated Patients
DISCUSSION
The aim of this study was to evaluate the impact of obesity on laparoscopic left colon resections and on the early postoperative outcomes of the procedure. The decision to restrict data analysis to the last 2 years of experience was based on the attempt to avoid significant technical changes in the operative procedure through the study period. The current technique of laparoscopic colectomy is well standardized at our institution and is followed by all surgeons. In our study, the conversion rate to open surgery and the incidence of perioperative complications observed in the whole population were similar to those reported by others11,13; however, interestingly, we had no conversions, no blood transfusions, and no anastomotic leaks in the obese group in this investigation. The comparative analysis of data showed that both the intraoperative difficulty and the postoperative course were similar between obese and nonobese patients whatever the indication for left colon resection. These findings are in quite striking contrast with previous reports of increased conversion rates and the complication risk of laparoscopic colectomy in obese patients. Although the number of obese patients we reviewed did not allow further stratification and we did not perform multivariate analysis for major end points of the procedure, our findings suggest that the laparoscopic approach for left colon resections is as feasible and at least as safe as in nonobese patients. The reasons for these particularly favorable outcomes of left colectomy in obese patients may perhaps depend on the use of a highly standardized surgical technique and perhaps on some particular aspects of it, which we analyze here.
Technical Considerations of Laparoscopic Left Colon Resections in Obese Patients
The Pneumoperitoneum
We usually performed an “open” pneumoperitoneum for the insertion of the first trocar, which is usually placed at the midline, just above the umbilicus. However, in case of previous abdominal surgery, we usually inflate the abdominal cavity using the Veress needle in the left subcostal area to insert the first trocar as far lateral as possible to avoid intraabdominal midline adhesions. The incidence of previous abdominal surgery was similar in both obese and nonobese patients in our study, thus the technique of pneumoperitoneum induction did not differ between groups.
The Number of Trocars
There is some evidence that obese patients would benefit from minimal wound traumatism more than nonobese patients4,13; however, the number of trocars, unlike their size and the length of the wound incision, have very little impact, if any, on postoperative outcomes.14 The ideal location and number of ports to perform laparoscopic left colon resections remain a matter of controversy between surgeons, varying from the 3-trocar technique advocated by Dr. Huscher, from Rome, Italy,15 to the 4- or 5-trocar technique that is most commonly used by others. In our study, the number of trocars was the only significant intraoperative parameter associated with obesity. Indeed, all the obese patients were systematically operated using with 6 ports. Conceivably, having 6 trocars and a greater availability of instruments in the abdominal cavity may help when exposure is difficult to maintain because of deepness, fatty mesentery, or an enlarged small bowel, as well as during mobilization of the splenic flexure.
Exposure
Intraabdominal adhesions and obesity are classic risk factors for conversion because they impair exposure, which is critical for laparoscopic surgery.2,7,16 Key factors for achieving proper exposure of the operative field are good bowel preparation and the optimal patient's position during the different steps of the procedures. To obtain optimal bowel preparation, in our practice, we ask the patient to adhere to a strict fiber-free diet 8 days before surgery and polyethylene glycol is prescribed 2 days before the operation to complete preparation. We found this method very efficient because it guarantees an empty digestive tract and flat small bowel, which facilitate layering of intestinal loops. Our technique of exposure imposes the patient in a slight Trendelenburg and right lateral tilt. Furthermore, small bowel loops are approached first and gently accommodated mostly in the upper right abdominal area. A trocar placed at the right hypochondrium is used to pass a grasper, which is then closed around a peritoneal fold in the right iliac fossa so that its shaft can be used to provide autostatic retraction of the small bowel loops, keeping them away from the midline and from the pelvic space. This kind of exposure's technique is an important feature of the procedure used at our institution because it allows wide access to the aortic axis, which is key for the performance of an easy medial-to-lateral approach to the mesocolon.
Dissection
We routinely perform medial-to-lateral laparoscopic dissection for all indications. In a recent randomized clinical trial comparing the medial-to-lateral laparoscopic dissection with the more classic lateral-to-medial approach for resection of rectosigmoid cancer, Liang et al17 showed that the medial approach reduces the operative time and the postoperative proinflammatory response. Besides the oncologic advantages of an early vessel division and a “no-touch” dissection, we feel that the longer the lateral abdominal wall attachments of the colon are preserved, the better the exposure and the easier the dissection. In both obese and nonobese patients in our study, the superior rectal vessels could be preserved in most patients treated for diverticulosis. With this approach, we also feel that proximal division of the inferior mesenteric artery can be performed more easily and safely in patients operated on for cancer.
In our study, obesity did not have any impact on the overall technical difficulty of the procedure as suggested by the fact that, unlike commonly reported by others, the operative time was not increased in obese patients with respect to the nonobese, and that the mobilization of the splenic flexure could be performed in a similar rate in both groups.
Oncologic Adequacy
Our results are in agreement with the findings of prospective and comparative studies demonstrating that the laparoscopic approach is as efficient as open surgery in achieving curative criteria for colorectal cancer.9,14,18 In our series, we found that resection margins and number of harvested lymph nodes are quite satisfying in terms of oncologic adequacy and that, interestingly, these parameters were not affected by obesity.
The Impact of Obesity on Surgical Outcomes
The real impact of obesity on the outcomes of general surgical procedures is a controversial matter. In a recent report published in the Lancet, Dindo and colleagues3 have evaluated the impact of obesity in a vast cohort study of more than 6300 patients undergoing different types of elective general surgery. Their findings contradict the long-held opinion that obesity is associated with increased surgical risk because they found no difference in postoperative outcomes between their subgroup of obese patients and the lean group. In their study, however, a significantly higher proportion of the obese patients had undergone minimally invasive surgery (47% obese vs. 34% normal; P <0.0001), suggesting that laparoscopy may have outweighed the risk associated with the condition of obesity.
It is probable that the opinion of obesity as a risk factor for surgery will be revised in the light of the profound changes that have occurred in general surgery since the advent of interventional laparoscopy. Indeed, others had already reported that operating on obese patients can be done as safely as in the nonobese when performing laparoscopic cholecystectomy.19 Our study now suggests that this is also true for laparoscopic left colectomy.
As a matter of fact, with the advent of minimally invasive techniques, operative risks decreased even for patients with class III obesity (BMI >40 kg/m2). Indeed, laparoscopic surgery has significantly improved postoperative outcomes of morbid obesity surgery (BMI 40 kg/m2 and higher), allowing for lower postoperative complication risks as well as earlier recovery with respect to conventional open surgery.4 Laparoscopic surgery for bowel resections has been associated with important benefits, which include decreased pulmonary complications, duration of hospital stay, perioperative stress response, incisional hernia, and small bowel occlusion.13 In obese patients, the laparoscopic approach seems also to eliminate the difference between obese and nonobese subjects in terms of wound infection rates.3
However, regarding the specific impact of obesity on complications after laparoscopic colectomy, opinions have remained, so far, controversial. Indeed, whereas some reported conversion and complication rates are similar to that of laparoscopic colectomy in the nonobese,5 most commonly, laparoscopic colectomy in the obese has been associated with at least an increased risk for conversion, which is deemed to be the result of a greater technical difficulty of the laparoscopic approach in these patients. Pikarsky et al7 reported on 31 patients undergoing laparoscopic colectomy with a BMI above 30 kg/m2 and found a conversion rate of 39% as well as a more prolonged hospital stay compared with the same operations performed in nonobese patients. Senagore et al6 have recently reported an interesting experience of laparoscopic colectomy in which they compared the outcomes of this surgery in obese and nonobese patients. In an identical way as in our present study, they identified only 2 groups in which obesity was defined as BMI over 30 kg/m2. These authors concluded that laparoscopic colectomy can be performed safely in both obese and nonobese patients with similar benefit of short hospital stay in both groups. However, their data showed that the obese group had significantly more conversions to open surgery (23.7% vs. 10.9%), longer operative time and higher morbidity rate (22% vs. 13%), and a higher anastomotic leakage rate (5.1% vs. 1.2%). In sharp contrast, data from our current study showed a 0% leak rate in the obese group versus a 3.5% in nonobese patients, which challenges the assumption of obesity as a risk factor for leakage. The absence of leaks in our obese population cannot be attributed to a selection bias in our study, which, unlike the series of Senagore et al, focused only on left colectomy. Indeed, left-sided colonic and colorectal anastomoses are known to have a higher leakage rate in open surgery.2 Furthermore, in the same study by Senagore et al, all leaks in the obese group occurred in colorectal anastomoses.
In our study also, conversion rate was not increased by obesity (actually, we observed conversions only in the nonobese group) and no significant difference was found for any other parameter evaluated.
We have discussed some technical considerations that may have determined these results of similar outcomes in both technical and postoperative complications of laparoscopic colectomy between obese and nonobese patients. We would again stress the importance of a well-standardized procedure and the crucial role of a perfect technique of exposure. It is also possible that our routine use of a medial-to-lateral approach for dissection of the mesocolon might have avoided conversions and longer operative time in our obese populations. With the surgical technique in use at our institution, it seems that obesity does not cause any greater technical challenge for laparoscopic left colectomy compared with the same procedure performed in lean subjects.
Our present findings suggest that when a laparoscopic approach can be performed in obese subjects with similar operative time and without significant risk of conversion to an open approach, the obese patients can fully benefit from the advantages of a minimally invasive surgery.
CONCLUSION
In contrast with previously reported series of laparoscopic colectomy, our findings show that obesity, intended as a BMI >30 kg/m2, does not have an adverse impact on the technical difficulty and postoperative outcomes of laparoscopic left colectomy. Our study supports the safety of using laparoscopic surgery for colorectal diseases in obese patients.
Footnotes
Reprints: Prof. Jacques Marescaux, MD, IRCAD/EITS, 1 Place de l'Hopital, 67091 Strasbourg, France. E-mail: Jacques.Marescaux@ircad.u-strasbg.fr.
REFERENCES
- 1.Eichenberger A, Proietti S, Wicky S, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg. 2002;95:1788–1792. [DOI] [PubMed] [Google Scholar]
- 2.Benoist S, Panis Y, Alves A, et al. Impact of obesity on surgical outcomes after colorectal resection. Am J Surg. 2000;179:275–281. [DOI] [PubMed] [Google Scholar]
- 3.Dindo D, Muller MK, Weber M, et al. Obesity in general elective surgery. Lancet. 2003;361:2032–2035. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234:279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tuech JJ, Regenet N, Hennekinne S, et al. Laparoscopic colectomy for sigmoid diverticulitis in obese and nonobese patients: a prospective comparative study. Surg Endosc. 2001;15:1427–1430. [DOI] [PubMed] [Google Scholar]
- 6.Senagore AJ, Delaney CP, Madboulay K, et al. Laparoscopic colectomy in obese and nonobese patients. J Gastrointest Surg. 2003;7:558–561. [DOI] [PubMed] [Google Scholar]
- 7.Pikarsky AJ, Saida Y, Yamaguchi T, et al. Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc. 2002;16:855–858. [DOI] [PubMed] [Google Scholar]
- 8.Smadja C, Sbai Idrissi M, Tahrat M, et al. Elective laparoscopic sigmoid colectomy for diverticulitis. Results of a prospective study. Surg Endosc. 1999;13:645–648. [DOI] [PubMed] [Google Scholar]
- 9.Hazebroek EJ, Color Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc. 2002;16:949–953. [DOI] [PubMed] [Google Scholar]
- 10.Marusch F, Gastinger I, Schneider C, et al.., Laparoscopic Colorectal Surgery Study Group (LCSSG). Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc. 2001;15:116–120. [DOI] [PubMed] [Google Scholar]
- 11.Kockerling F, Schneider C, Reymond MA, et al. Early results of a prospective multicenter study on 500 consecutive cases of laparoscopic colorectal surgery. Laparoscopic Colorectal Surgery Study Group (LCSSG). Surg Endosc. 1998;12:37–41. [DOI] [PubMed] [Google Scholar]
- 12.Leroy J, Okuda J, Milsom J. Laparoscopic sigmoidectomy of cancer. Available at: www.websurg.com.
- 13.Braga M, Vignali A, Gianotti L, et al. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002;236:759–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lumley J, Stitz R, Stevenson A, et al. Laparoscopic colorectal surgery for cancer: intermediate to long-term outcomes. Dis Colon Rectum. 2002;45:867–872. [DOI] [PubMed] [Google Scholar]
- 15.Huscher C. Laparoscopic sigmoidectomy. Available at: www.weebsurg.com.
- 16.Trebuchet G, Lechaux D, Lecalve JL. Laparoscopic left colon resection for diverticular disease. Surg Endosc. 2002;16:18–21. [DOI] [PubMed] [Google Scholar]
- 17.Liang JT, Lai HS, Huang KC, et al. Comparison of medial-to-lateral versus traditional lateral-to-medial laparoscopic dissection sequences for resection of rectosigmoid cancers: randomized controlled clinical trial. World J Surg. 2003;27:190–196. [DOI] [PubMed] [Google Scholar]
- 18.Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. [DOI] [PubMed] [Google Scholar]
- 19.Miles RH, Carballo RE, Prinz RA, et al. Laparoscopy: the preferred method of cholecystectomy in the morbidly obese. Surgery. 1992;112:818–822. [PubMed] [Google Scholar]