Abstract
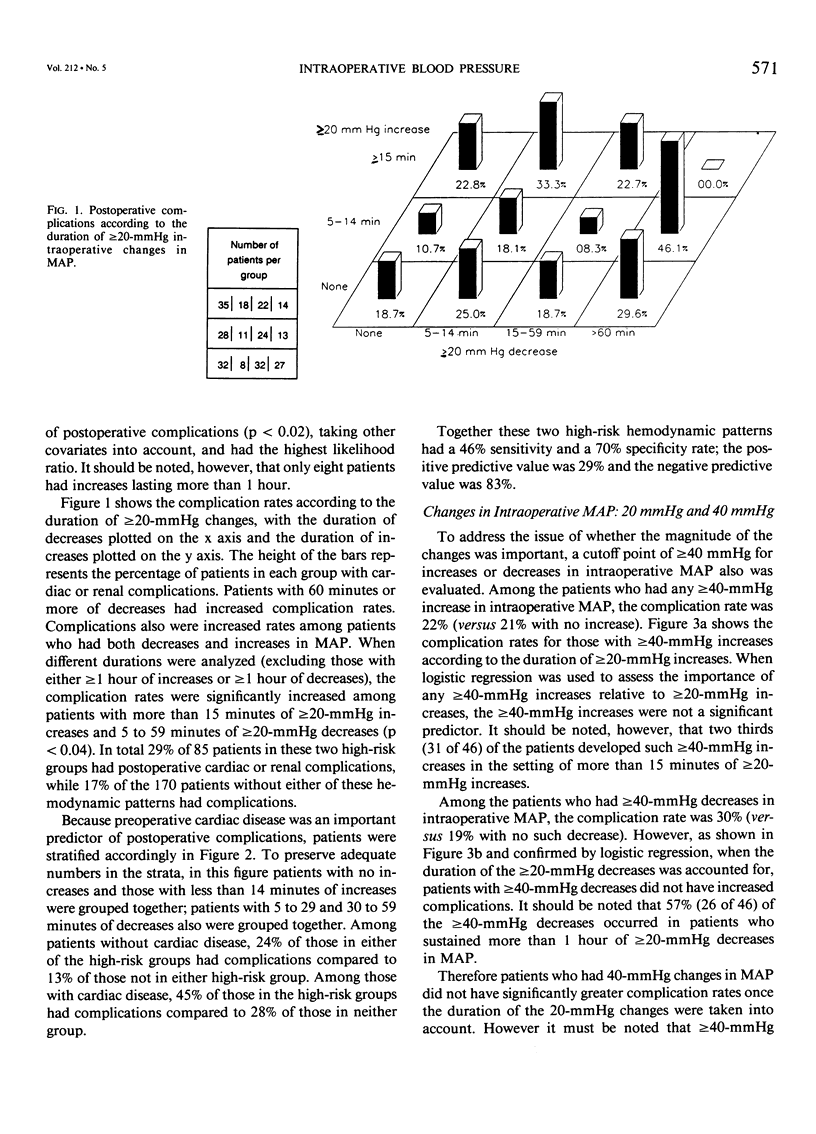
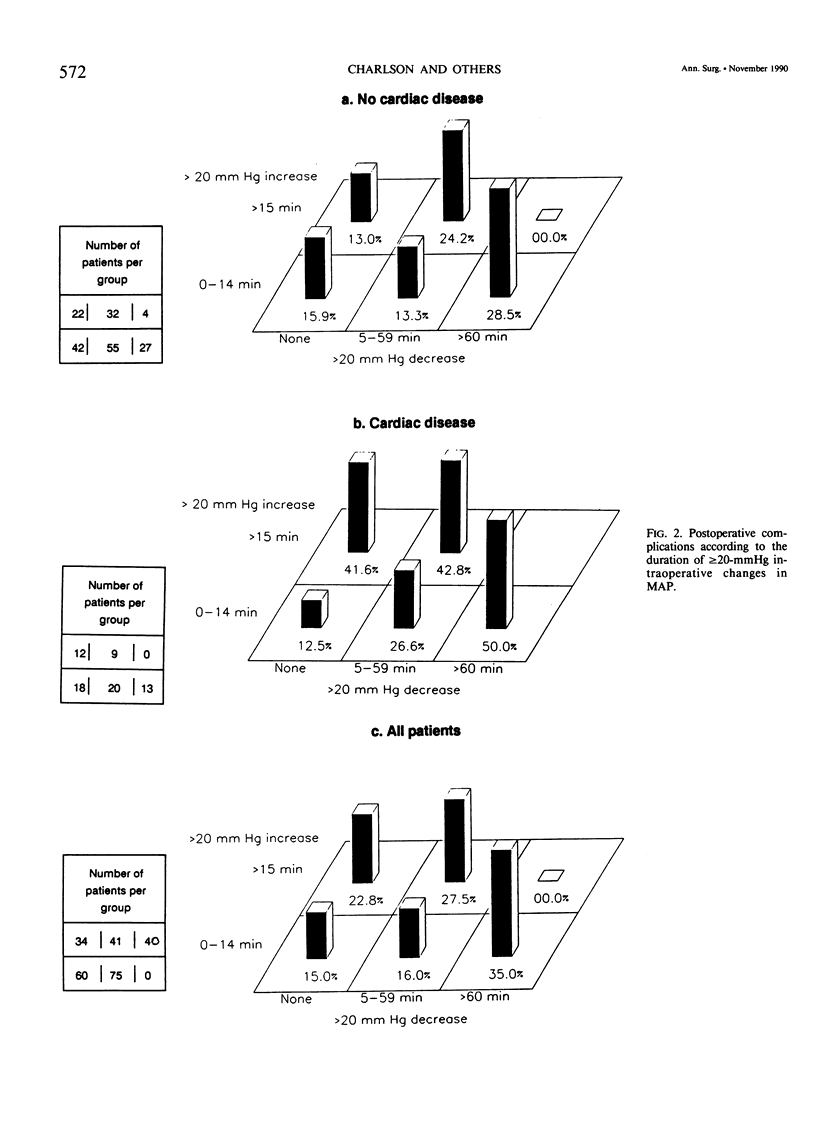
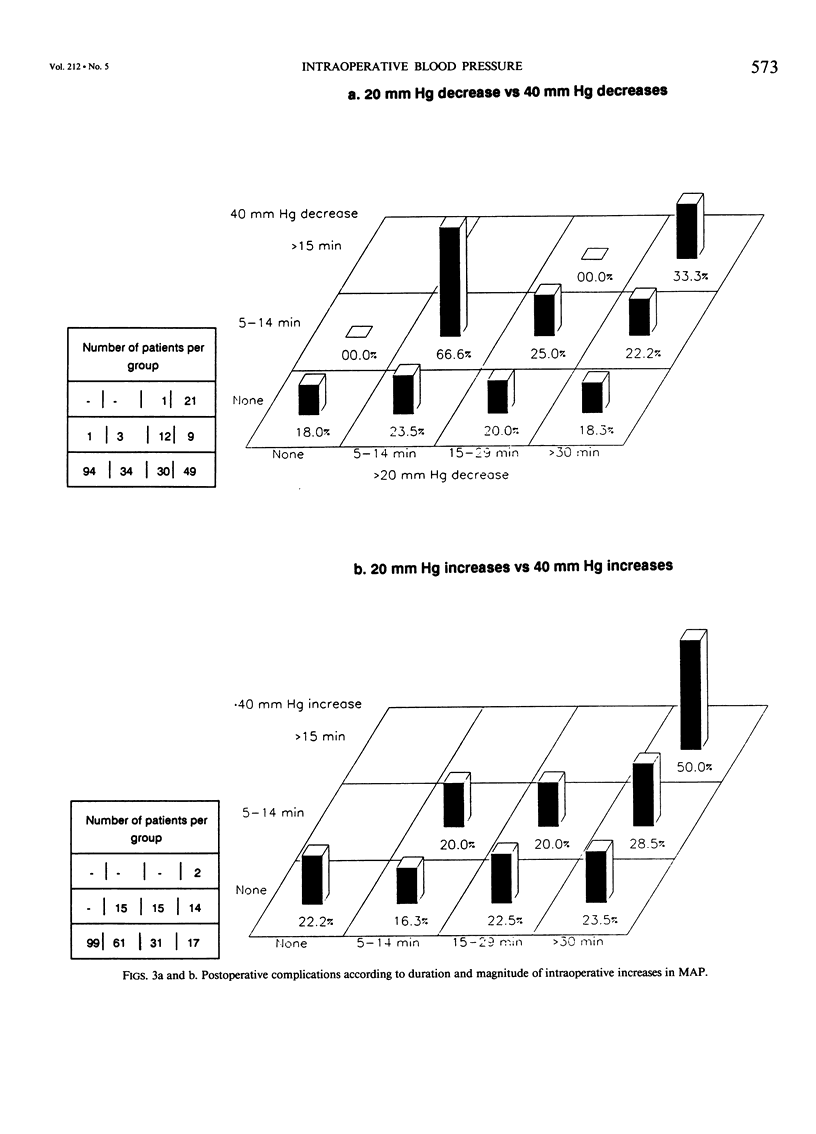
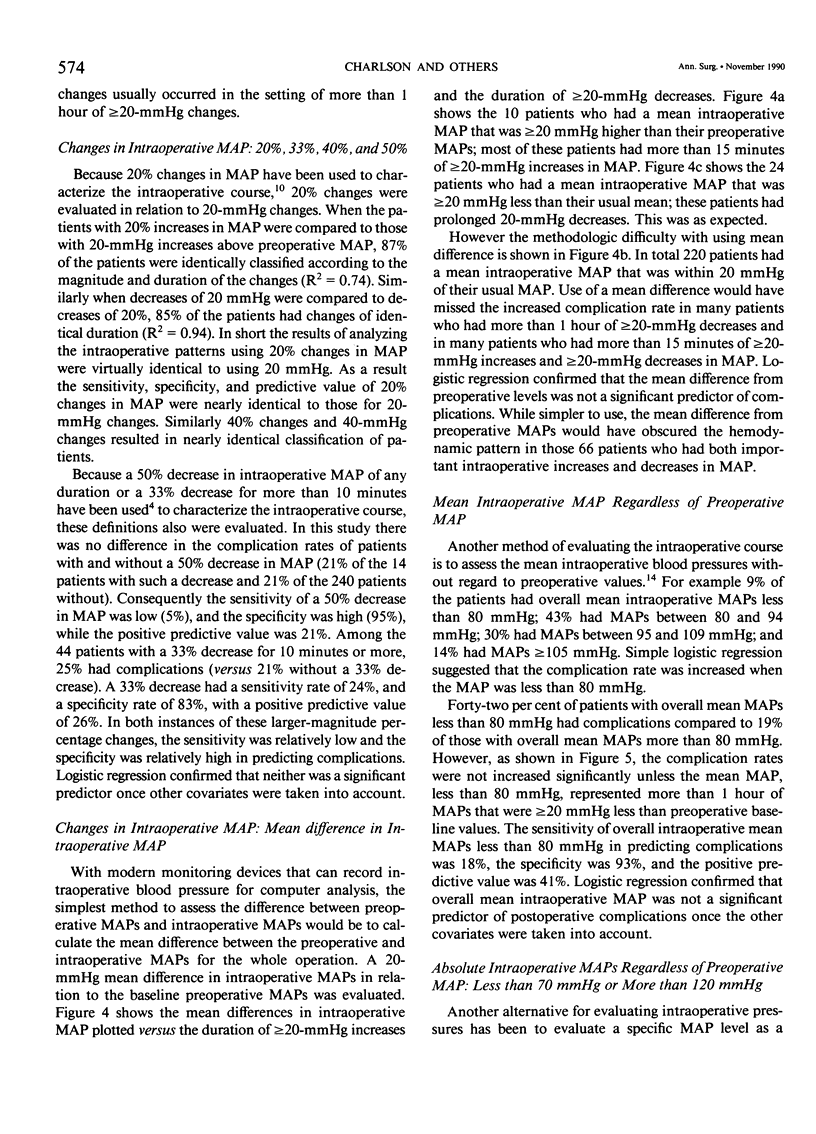
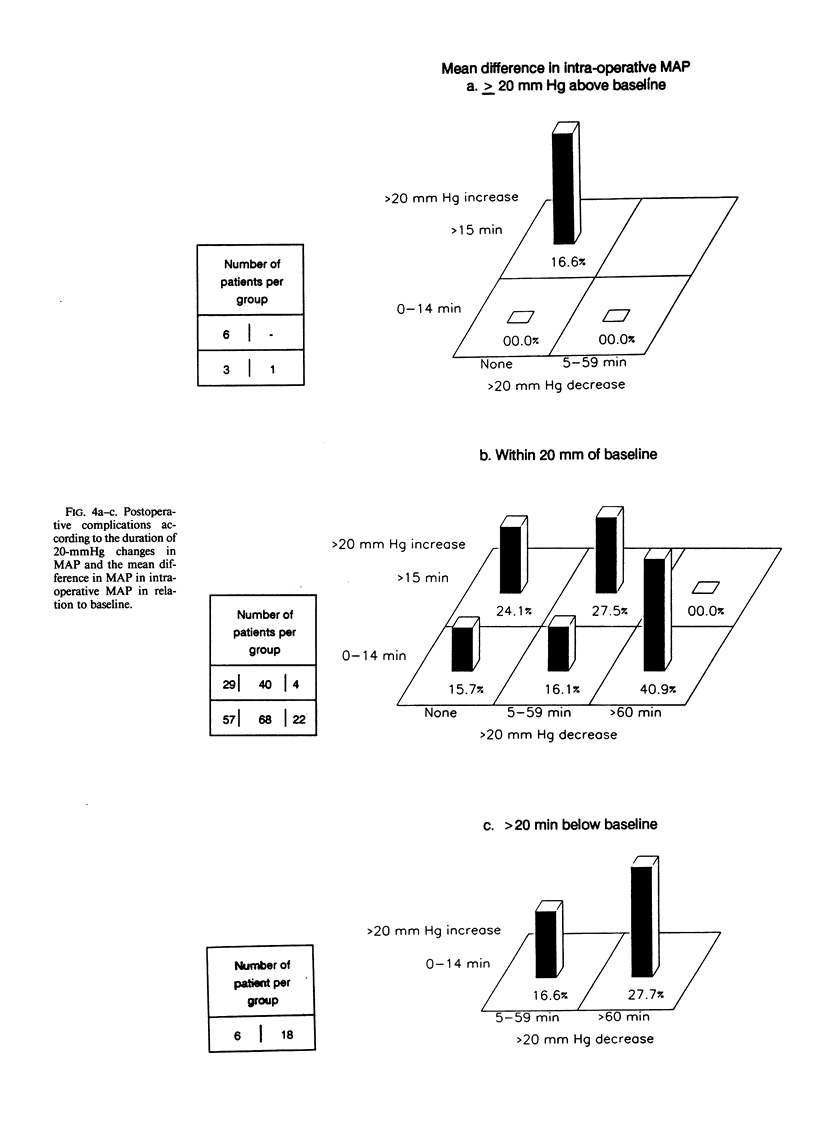
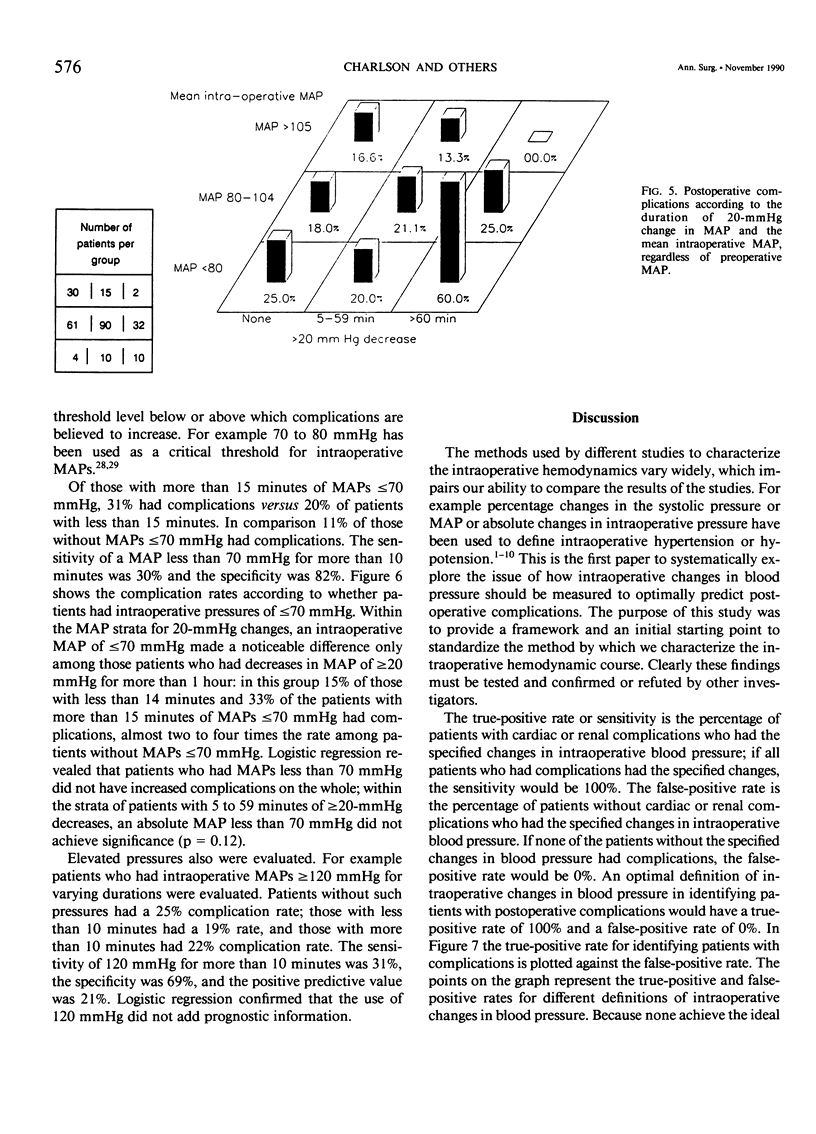
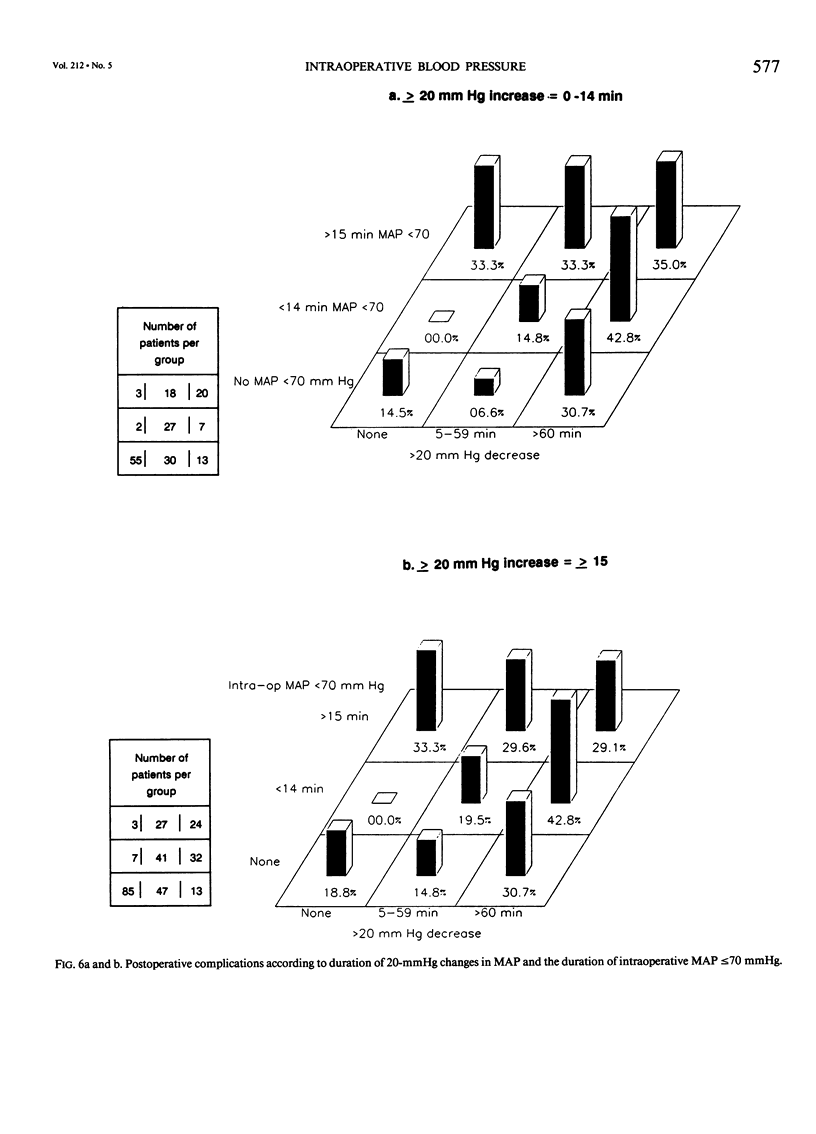
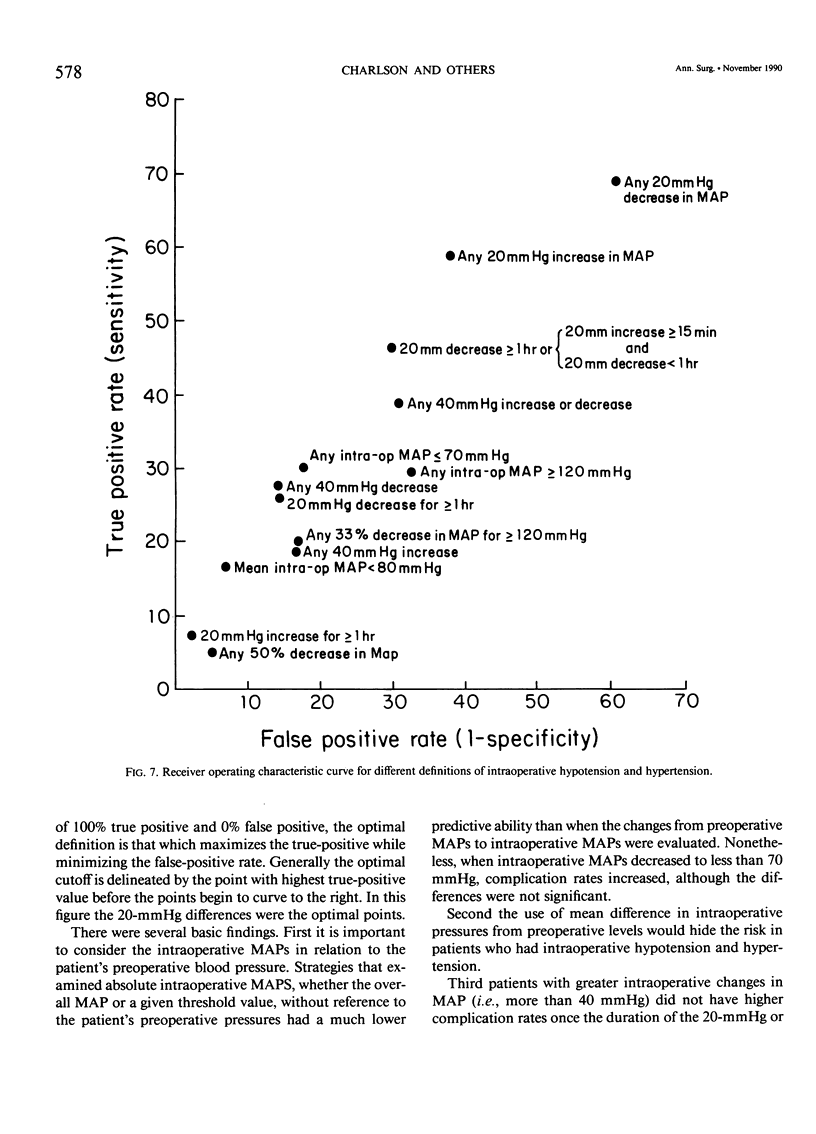
While monitoring blood pressure is a routine part of intraoperative management, several methods have been proposed to characterize intraoperative hemodynamic patterns as predictors of postoperative complications. In this prospective study of a high-risk population of hypertensive and diabetic patients undergoing elective noncardiac surgery, one objective was to compare different approaches to the assessment of intraoperative hemodynamic patterns to identify those patterns most likely to be associated with postoperative complications. Twenty-one per cent of the 254 patients sustained cardiac or renal complications after operation. Patients with more than 1 hour of greater than or equal to 20-mmHg decreases in mean arterial pressure (MAP) or patients with less than 1 hour of greater than or equal to 20-mmHg decreases and more than 15 minutes of greater than or equal to 20-mmHg increases were at highest risk for postoperative complications. Together these two patterns had a 46% sensitivity rate and a 70% specificity rate in predicting postoperative complications. Using 20% change in intraoperative MAP produced results nearly identical to 20-mmHg changes. When the duration of 20-mmHg changes was accounted for, changes of a greater magnitude (e.g., 40 mmHg) were not significant independent predictors of complications. The use of the mean difference from preoperative MAP was misleading because patients who experienced both high and low MAPs tended to have nearly normal mean MAPs, but high complication rates. The absolute magnitude of intraoperative MAPs, regardless of the preoperative levels, also was evaluated. The overall mean intraoperative MAP was not a significant predictor of complications. Specific intraoperative MAPs (e.g., less than 70 mmHg and more than 120 mmHg) also were evaluated. While neither was a significant predictor, there was a trend for increased complications among patients whose MAPs decreased to less than 70 mmHg. Intraoperative blood pressure should be analyzed in relation to the patient's preoperative blood pressure. Prolonged changes of more than 20 mmHg or 20% in relation to preoperative levels were significantly related to complications.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barash P. G., Kopriva C. J. The rate-pressure product in clinical anesthesia: boon or bane? Anesth Analg. 1980 Apr;59(4):229–231. [PubMed] [Google Scholar]
- Brazier J., Cooper N., Buckberg G. The adequacy of subendocardial oxygen delivery: the interaction of determinants of flow, arterial oxygen content and myocardial oxygen need. Circulation. 1974 May;49(5):968–977. doi: 10.1161/01.cir.49.5.968. [DOI] [PubMed] [Google Scholar]
- CHAMBERLAIN D. A., EDMONDS-SEAL J. EFFECTS OF SURGERY UNDER GENERAL ANAESTHESIA ON THE ELECTROCARDIOGRAM IN ISCHAEMIC HEART DISEASE AND HYPERTENSION. Br Med J. 1964 Sep 26;2(5412):784–787. doi: 10.1136/bmj.2.5412.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson M. E., Horwitz R. I. Applying results of randomised trials to clinical practice: impact of losses before randomisation. Br Med J (Clin Res Ed) 1984 Nov 10;289(6454):1281–1284. doi: 10.1136/bmj.289.6454.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson M. E., MacKenzie C. R., Ales K. L., Gold J. P., Fairclough G. F., Jr, Shires G. T. The post-operative electrocardiogram and creatine kinase: implications for diagnosis of myocardial infarction after non-cardiac surgery. J Clin Epidemiol. 1989;42(1):25–34. doi: 10.1016/0895-4356(89)90022-x. [DOI] [PubMed] [Google Scholar]
- Charlson M. E., MacKenzie C. R., Gold J. P., Ales K. L., Shires G. T. Postoperative renal dysfunction can be predicted. Surg Gynecol Obstet. 1989 Oct;169(4):303–309. [PubMed] [Google Scholar]
- Charlson M. E., MacKenzie C. R., Gold J. P., Ales K. L., Topkins M., Fairclough G. P., Jr, Shires G. T. The preoperative and intraoperative hemodynamic predictors of postoperative myocardial infarction or ischemia in patients undergoing noncardiac surgery. Ann Surg. 1989 Nov;210(5):637–648. doi: 10.1097/00000658-198911000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson M. E., MacKenzie C. R., Gold J. P., Shires G. T. Postoperative changes in serum creatinine. When do they occur and how much is important? Ann Surg. 1989 Mar;209(3):328–333. doi: 10.1097/00000658-198903000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coriat P., Harari A., Daloz M., Viars P. Clinical predictors of intraoperative myocardial ischemia in patients with coronary artery disease undergoing non-cardiac surgery. Acta Anaesthesiol Scand. 1982 Aug;26(4):287–290. doi: 10.1111/j.1399-6576.1982.tb01768.x. [DOI] [PubMed] [Google Scholar]
- Goldman L., Caldera D. L. Risks of general anesthesia and elective operation in the hypertensive patient. Anesthesiology. 1979 Apr;50(4):285–292. doi: 10.1097/00000542-197904000-00002. [DOI] [PubMed] [Google Scholar]
- Goldman L., Caldera D. L., Southwick F. S., Nussbaum S. R., Murray B., O'Malley T. A., Goroll A. H., Caplan C. H., Nolan J., Burke D. S. Cardiac risk factors and complications in non-cardiac surgery. Medicine (Baltimore) 1978 Jul;57(4):357–370. doi: 10.1097/00005792-197807000-00006. [DOI] [PubMed] [Google Scholar]
- Hammon J. W., Jr, Wood A. J., Prager R. L., Wood M., Muirhead J., Bender H. W., Jr Perioperative beta blockade with propranolol: reduction in myocardial oxygen demands and incidence of atrial and ventricular arrhythmias. Ann Thorac Surg. 1984 Oct;38(4):363–367. doi: 10.1016/s0003-4975(10)62287-4. [DOI] [PubMed] [Google Scholar]
- Hoffman J. I. Determinants and prediction of transmural myocardial perfusion. Circulation. 1978 Sep;58(3 Pt 1):381–391. doi: 10.1161/01.cir.58.3.381. [DOI] [PubMed] [Google Scholar]
- Kissin I., Reves J. G., Mardis M. Is the rate-pressure product a misleading guide? Anesthesiology. 1980 Apr;52(4):373–374. doi: 10.1097/00000542-198004000-00024. [DOI] [PubMed] [Google Scholar]
- Langfitt T. W. Cerebral circulation and metabolism. Summary of International Symposium, June 6-10, 1973. J Neurosurg. 1974 May;40(5):561–576. doi: 10.3171/jns.1974.40.5.0561. [DOI] [PubMed] [Google Scholar]
- Larson C. P., Jr, Mazze R. I., Cooperman L. H., Wollman H. Effects of anesthetics on cerebral, renal, and splanchnic circulations: recent developments. Anesthesiology. 1974 Aug;41(2):169–181. doi: 10.1097/00000542-197408000-00007. [DOI] [PubMed] [Google Scholar]
- Mauney F. M., Jr, Ebert P. A., Sabiston D. C., Jr Postoperative myocardial infarction: a study of predisposing factors, diagnosis and mortality in a high risk group of surgical patients. Ann Surg. 1970 Sep;172(3):497–503. doi: 10.1097/00000658-197009000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NACHLAS M. M., ABRAMS S. J., GOLDBERG M. M. The influence of arteriosclerotic heart disease on surgical risk. Am J Surg. 1961 Apr;101:447–455. doi: 10.1016/0002-9610(61)90296-3. [DOI] [PubMed] [Google Scholar]
- O'Callaghan W. G., Fitzgerald D. J., O'Malley K., O'Brien E. Accuracy of indirect blood pressure measurement in the elderly. Br Med J (Clin Res Ed) 1983 May 14;286(6377):1545–1546. doi: 10.1136/bmj.286.6377.1545-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prys-Roberts C., Foëx P., Greene L. T., Waterhouse T. D. Studies of anaesthesia in relation to hypertension. IV. The effects of artificial ventilation on the circulation and pulmonary gas exchanges. Br J Anaesth. 1972 Apr;44(4):335–349. doi: 10.1093/bja/44.4.335. [DOI] [PubMed] [Google Scholar]
- Rao T. L., Jacobs K. H., El-Etr A. A. Reinfarction following anesthesia in patients with myocardial infarction. Anesthesiology. 1983 Dec;59(6):499–505. doi: 10.1097/00000542-198312000-00003. [DOI] [PubMed] [Google Scholar]
- Roy W. L., Edelist G., Gilbert B. Myocardial ischemia during non-cardiac surgical procedures in patients with coronary-artery disease. Anesthesiology. 1979 Nov;51(5):393–397. doi: 10.1097/00000542-197911000-00005. [DOI] [PubMed] [Google Scholar]
- SHIPLEY R. E., STUDY R. S. Changes in renal blood flow, extraction of inulin, glomerular filtration rate, tissue pressure and urine flow with acute alterations of renal artery blood pressure. Am J Physiol. 1951 Dec;167(3):676–688. doi: 10.1152/ajplegacy.1951.167.3.676. [DOI] [PubMed] [Google Scholar]
- Sechzer P. H., Wachtel J., Keats A. S. Circulatory lability and myocardial stress in patients undergoing cardiovascular surgery. Am J Surg. 1968 Nov;116(5):686–692. doi: 10.1016/0002-9610(68)90348-6. [DOI] [PubMed] [Google Scholar]
- Slogoff S., Keats A. S. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology. 1985 Feb;62(2):107–114. doi: 10.1097/00000542-198502000-00002. [DOI] [PubMed] [Google Scholar]
- Slogoff S., Keats A. S. Randomized trial of primary anesthetic agents on outcome of coronary artery bypass operations. Anesthesiology. 1989 Feb;70(2):179–188. doi: 10.1097/00000542-198902000-00002. [DOI] [PubMed] [Google Scholar]
- Steen P. A., Tinker J. H., Tarhan S. Myocardial reinfarction after anesthesia and surgery. JAMA. 1978 Jun 16;239(24):2566–2570. doi: 10.1001/jama.239.24.2566. [DOI] [PubMed] [Google Scholar]
- THURAU K. RENAL HEMODYNAMICS. Am J Med. 1964 May;36:698–719. doi: 10.1016/0002-9343(64)90181-0. [DOI] [PubMed] [Google Scholar]
- Thomson I. R., Mutch W. A., Culligan J. D. Failure of intravenous nitroglycerin to prevent intraoperative myocardial ischemia during fentanyl-pancuronium anesthesia. Anesthesiology. 1984 Oct;61(4):385–393. doi: 10.1097/00000542-198410000-00005. [DOI] [PubMed] [Google Scholar]
- von Knorring J. Postoperative myocardial infarction: a prospective study in a risk group of surgical patients. Surgery. 1981 Jul;90(1):55–60. [PubMed] [Google Scholar]


