Figure 1. Development of atherosclerosis.
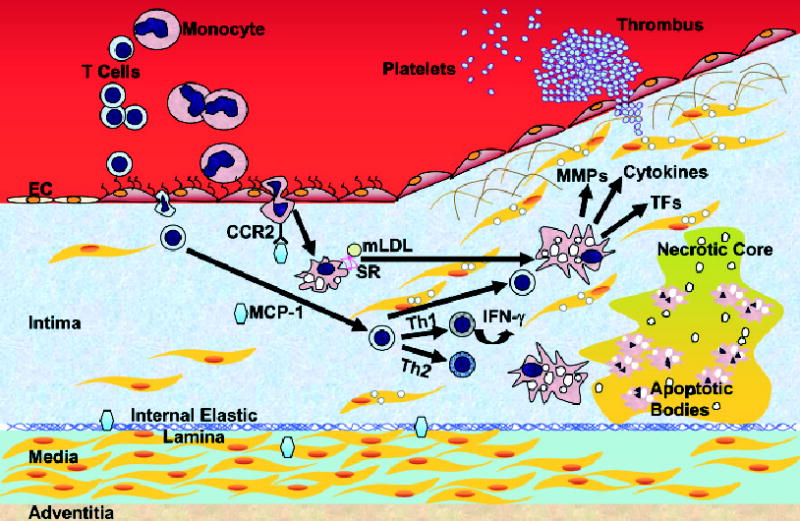
Monocytes and T-leukocytes do not adhere to ECs under normal conditions. 1. Adhesion. When ECs undergo inflammatory activation they express adhesion molecules, and leukocytes are trapped by ECs. 2. Transmigration. Once adherent, leukocytes migrate into the intima. 3. Foam cell formation. In the intima, monocytes differentiate into macrophages and take up lipids. 4. Progression. T cells are activated and further stimulate macrophages. SMCs of the media migrate to the top of the intima to form a fibrous cap over the lipid core. Further activation of macrophages produces MMPs that degrade the extracellular matrix and weaken the fibrous cap. 5. Plaque rupture. When the plaque ruptures, it allows the blood to contact to the procoagulant protein, tissue factor, and activate the coagulant cascade. Macrophages eventually die in a central core by apoptosis or necrosis, which forms a necrotic core in the lesion. IFN-γ, interferon-γ; MCP-1, monocyte chemoattractant protein-1; mLDL, modified LDL; MMP, matrix metalloproteinase; SR, scavenger receptors; TF, tissue factor. Note: Mast cells play an important role in atherogenesis. The interaction of the chemokine receptor CCR3 on the surface of mast cells and eotaxin, a chemoattractant, may facilitate the trans-migration of these cells. In the intima, they undergo degranulation and release factors that contribute to atherogenesis. Mast cells are not indicated.
