Figure 2. Evolution of atheroma.
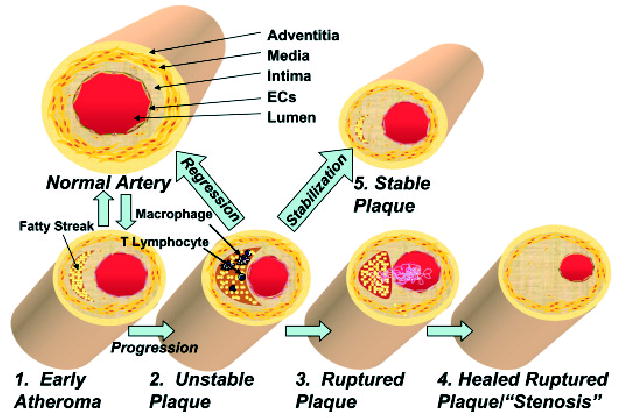
The normal human coronary artery has a trilaminar structure. 1. Early atherosclerotic lesions. In early atherogenesis, migration of immune cells and the accumulation of lipids in macrophages lead to the formation of fatty streaks. These early lesions frequently regress spontaneously. 2. Vulnerable plaque. If inflammatory conditions persist, the lipid core grows. Further activation of macrophages secretes matrix degrading enzymes and weakens the fibrous cap, which leads to vulnerable plaques prone to rupture. 3. Plaque rupture. Disruption of the fibrous cap causes the direct contact of blood components to tissue factor and initiates coagulation. This leads to the formation of the thrombus. 4. Stenosis. A wound healing response stimulates smooth muscle cell migration and collagen synthesis. This process results in a thick fibrous cap and expansion of the intima, which constricts the lumen. 5. Stabilization. Drug treatment or gene therapy for dyslipidemia remodels the nature of the vulnerable plaques, which reduces the incidence of acute coronary events. 6. Regression. Advanced atherosclerotic lesions could be regressed under aggressive lipid lowering or drug treatments.
