Abstract
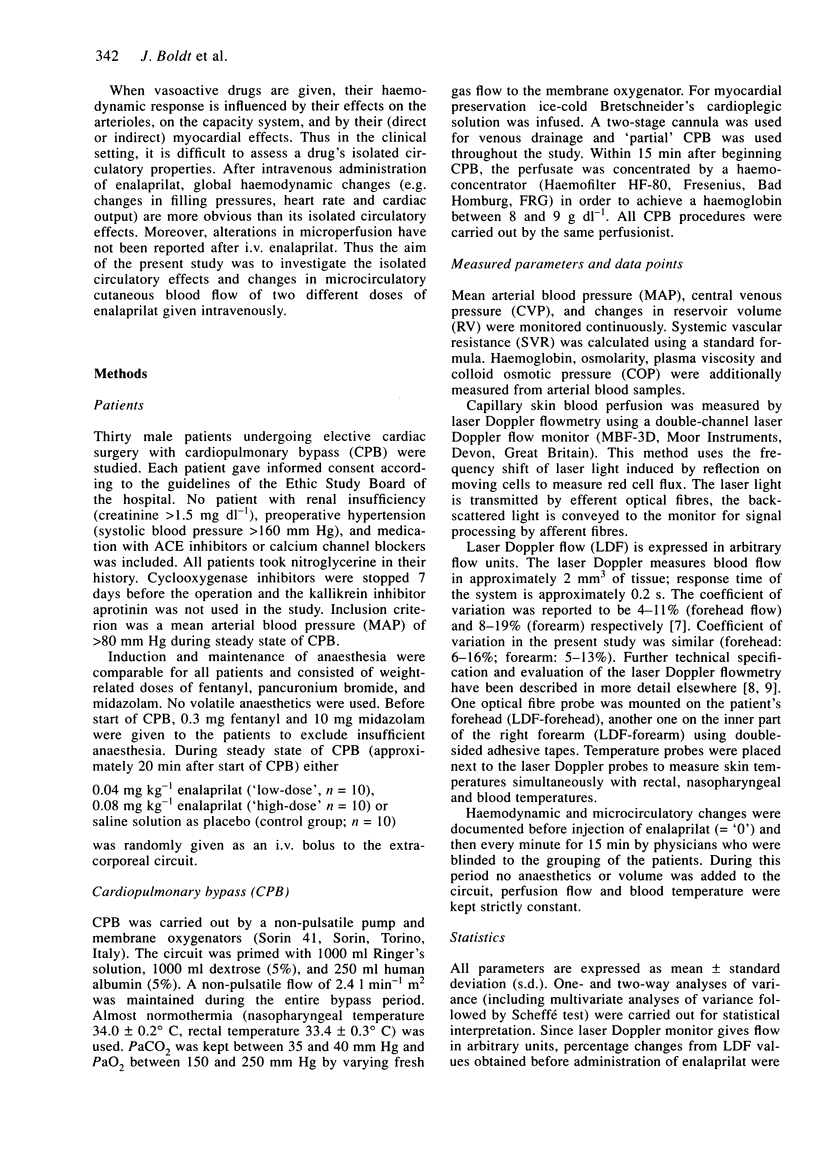
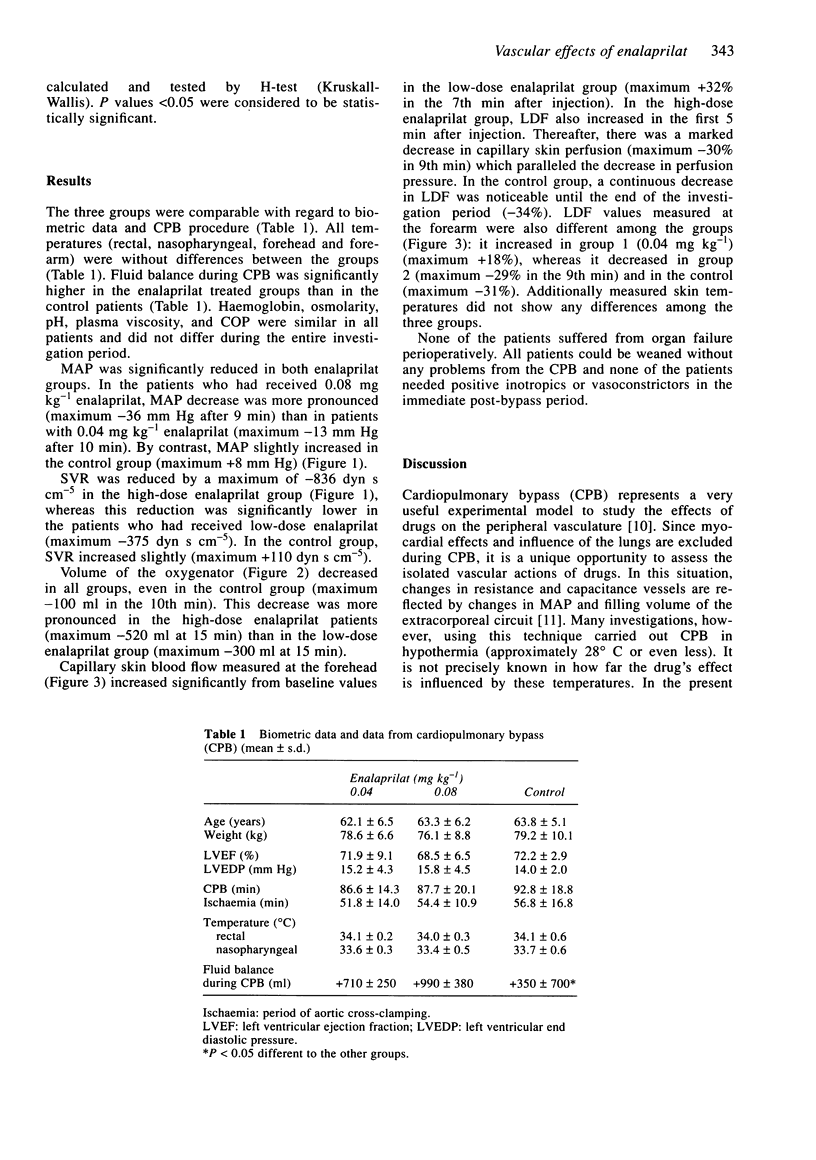
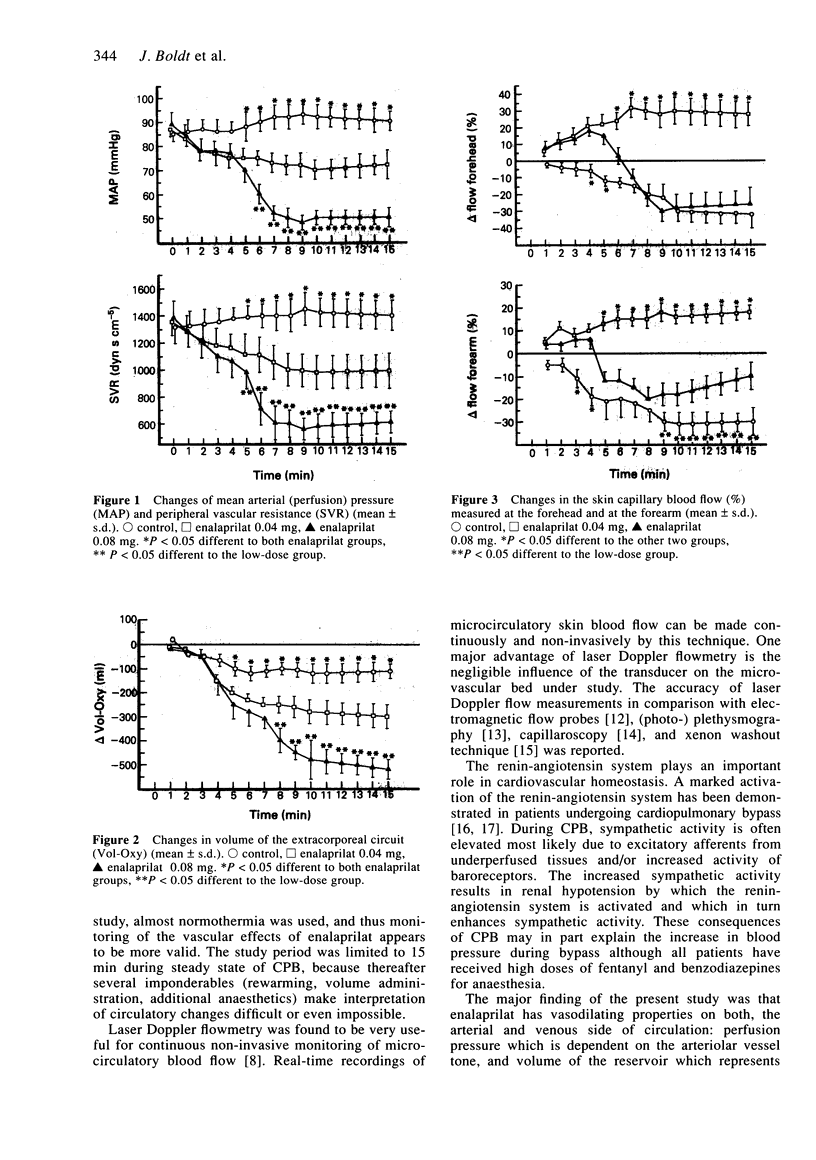
The isolated vascular effects of intravenous administration of the angiotensin converting enzyme (ACE) inhibitor enalaprilat were investigated. Thirty male patients undergoing cardiopulmonary bypass (CPB) were studied. According to a randomized sequence, 0.04 mg kg-1 enalaprilat (low-dose, n = 10), 0.08 mg kg-1 (high-dose, n = 10) enalaprilat or saline solution as placebo (control group, n = 10) was given as an i.v. bolus during CPB. Changes in mean arterial pressure (MAP) and venous reservoir (RV) of the extracorporeal circulation were studied as indices of arterial resistance and venous capacitance. Mean arterial blood pressure (MAP) and peripheral vascular resistance (SVR) were significantly more reduced in the high-dose enalaprilat group (MAP: -36 mm Hg after 9 min; SVR: -836 dyn s cm-5) than in the low-dose group (MAP: -13 mm Hg after 10 min). Volume of the reservoir (RV) decreased in both enalaprilat treated groups indicating additional (dose-dependent) venous pooling effects of the substance (low-dose: -300 ml; high-dose: -520 ml; control group: -100 ml). Skin capillary blood flow measured by laser Doppler flowmetry (LDF) increased after injection of 0.04 mg kg-1 enalaprilat, whereas it decreased significantly when MAP fell markedly in patients treated with high-dose enalaprilat. I.v. enalaprilat had dose-dependent vasodilating properties in the arterial and venous vessel system indicating reduction in pre- and afterload. Microcirculation in both enalaprilat treated groups improved as long as reduction in blood pressure was not limited.
Full text
PDF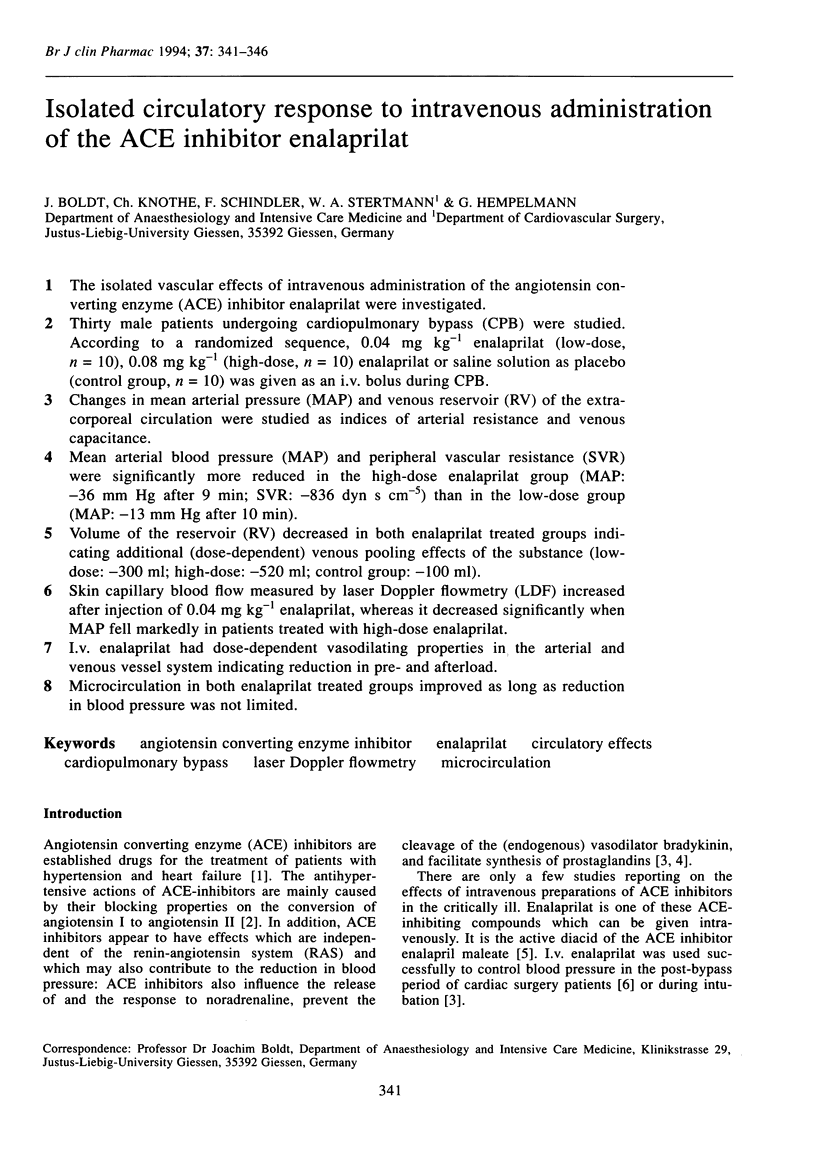
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baraka A., Haroun S., Baroody M., Nawfal M., Sibai A. Action of adrenergic agonists on resistance v capacitance vessels during cardiopulmonary bypass. J Cardiothorac Anesth. 1989 Apr;3(2):193–195. doi: 10.1016/s0888-6296(89)92738-5. [DOI] [PubMed] [Google Scholar]
- Boggett D., Blond J., Rolfe P. Laser Doppler measurements of blood flow in skin tissue. J Biomed Eng. 1985 Jul;7(3):225–232. doi: 10.1016/0141-5425(85)90023-8. [DOI] [PubMed] [Google Scholar]
- Chatterjee K., De Marco T. Systemic and coronary haemodynamics and pharmacodynamics of enalapril and enalaprilat in congestive heart failure. Drugs. 1990;39 (Suppl 4):29–42. doi: 10.2165/00003495-199000394-00007. [DOI] [PubMed] [Google Scholar]
- Creager M. A., Halperin J. L., Bernard D. B., Faxon D. P., Melidossian C. D., Gavras H., Ryan T. J. Acute regional circulatory and renal hemodynamic effects of converting-enzyme inhibition in patients with congestive heart failure. Circulation. 1981 Sep;64(3):483–489. doi: 10.1161/01.cir.64.3.483. [DOI] [PubMed] [Google Scholar]
- Dickstein K., Aarsland T., Tjelta K., Cirillo V. J., Gomez H. J. A comparison of hypotensive responses after oral and intravenous administration of enalapril and lisinopril in chronic heart failure. J Cardiovasc Pharmacol. 1987 Jun;9(6):705–710. doi: 10.1097/00005344-198706000-00011. [DOI] [PubMed] [Google Scholar]
- Dickstein K., Till A. E., Aarsland T., Tjelta K., Abrahamsen A. M., Kristianson K., Gomez H. J., Gregg H., Hichens M. The pharmacokinetics of enalapril in hospitalized patients with congestive heart failure. Br J Clin Pharmacol. 1987 Apr;23(4):403–410. doi: 10.1111/j.1365-2125.1987.tb03069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards C. R., Padfield P. L. Angiotensin-converting enzyme inhibitors: past, present, and bright future. Lancet. 1985 Jan 5;1(8419):30–34. doi: 10.1016/s0140-6736(85)90975-4. [DOI] [PubMed] [Google Scholar]
- Galvao M. Role of angiotensin-converting enzyme inhibitors in congestive heart failure. Heart Lung. 1990 Sep;19(5 Pt 1):505–511. [PubMed] [Google Scholar]
- Kubo S. H., Cody R. J., Laragh J. H., Prida X. E., Atlas S. A., Yuan Z., Sealey J. E. Immediate converting-enzyme inhibition with intravenous enalapril in chronic congestive heart failure. Am J Cardiol. 1985 Jan 1;55(1):122–126. doi: 10.1016/0002-9149(85)90312-1. [DOI] [PubMed] [Google Scholar]
- Levy J. H., Hug C. C., Jr Use of cardiopulmonary bypass in studies of the circulation. Br J Anaesth. 1988;60(8 Suppl 1):35S–37S. doi: 10.1093/bja/60.suppl_1.35s. [DOI] [PubMed] [Google Scholar]
- Micheels J., Alsbjorn B., Sorensen B. Laser doppler flowmetry. A new non-invasive measurement of microcirculation in intensive care? Resuscitation. 1984 May;12(1):31–39. doi: 10.1016/0300-9572(84)90056-x. [DOI] [PubMed] [Google Scholar]
- Murphy J. D., Vaughan R. S., Rosen M. Intravenous enalaprilat and autonomic reflexes. The effects of enalaprilat on the cardiovascular responses to postural changes and tracheal intubation. Anaesthesia. 1989 Oct;44(10):816–821. doi: 10.1111/j.1365-2044.1989.tb09098.x. [DOI] [PubMed] [Google Scholar]
- Neutel J. M., Luther R. R., Boger R. S., Weber M. A. Immediate blood pressure effects of the renin inhibitor enalkiren and the angiotensin-converting enzyme inhibitor enalaprilat. Am Heart J. 1991 Oct;122(4 Pt 1):1094–1100. doi: 10.1016/0002-8703(91)90477-y. [DOI] [PubMed] [Google Scholar]
- Rutledge J., Ayers C., Davidson R., DiPette D., Guthrie G., Fisher M., Schwartz S., Rucinska E. Effect of intravenous enalaprilat in moderate and severe systemic hypertension. Am J Cardiol. 1988 Nov 15;62(16):1062–1067. doi: 10.1016/0002-9149(88)90549-8. [DOI] [PubMed] [Google Scholar]
- Stern M. D., Bowen P. D., Parma R., Osgood R. W., Bowman R. L., Stein J. H. Measurement of renal cortical and medullary blood flow by laser-Doppler spectroscopy in the rat. Am J Physiol. 1979 Jan;236(1):F80–F87. doi: 10.1152/ajprenal.1979.236.1.F80. [DOI] [PubMed] [Google Scholar]
- Stern M. D., Lappe D. L., Bowen P. D., Chimosky J. E., Holloway G. A., Jr, Keiser H. R., Bowman R. L. Continuous measurement of tissue blood flow by laser-Doppler spectroscopy. Am J Physiol. 1977 Apr;232(4):H441–H448. doi: 10.1152/ajpheart.1977.232.4.H441. [DOI] [PubMed] [Google Scholar]
- Taylor K. M., Bain W. H., Morton J. J. The role of angiotensin II in the development of peripheral vasoconstriction during open-heart surgery. Am Heart J. 1980 Dec;100(6 Pt 1):935–937. doi: 10.1016/0002-8703(80)90081-2. [DOI] [PubMed] [Google Scholar]
- Taylor K. M., Morton I. J., Brown J. J., Bain W. H., Caves P. K. Hypertension and the renin-angiotensin system following open-heart surgery. J Thorac Cardiovasc Surg. 1977 Dec;74(6):840–845. [PubMed] [Google Scholar]
- Tenland T., Salerud E. G., Nilsson G. E., Oberg P. A. Spatial and temporal variations in human skin blood flow. Int J Microcirc Clin Exp. 1983;2(2):81–90. [PubMed] [Google Scholar]
- Tooke J. E., Ostergren J., Fagrell B. Synchronous assessment of human skin microcirculation by laser Doppler flowmetry and dynamic capillaroscopy. Int J Microcirc Clin Exp. 1983;2(4):277–284. [PubMed] [Google Scholar]
- Waxman K., Formosa P., Soliman H., Tominaga G., Police A., Hyatt J. Laser Doppler velocimetry in critically ill patients. Crit Care Med. 1987 Aug;15(8):780–783. doi: 10.1097/00003246-198708000-00015. [DOI] [PubMed] [Google Scholar]


