Abstract
1. The effect on coronary vascular resistance of selective stimulation of the Aδ, B and sC fibre groups of the post-ganglionic cardiac sympathetic nerves was studied. The main left coronary artery was perfused at constant flow. The oxygen saturation of coronary sinus blood was measured continuously.
2. Stimulation of the peripheral ends of the cut Aδ afferent fibres, normally excited by myocardial ischaemia, had no effect on coronary vascular resistance; these fibres do not evoke an axon reflex in the heart.
3. Stimulation of the preganglionic B fibres that run without synapse through the stellate ganglion also had no measurable effect on coronary resistance.
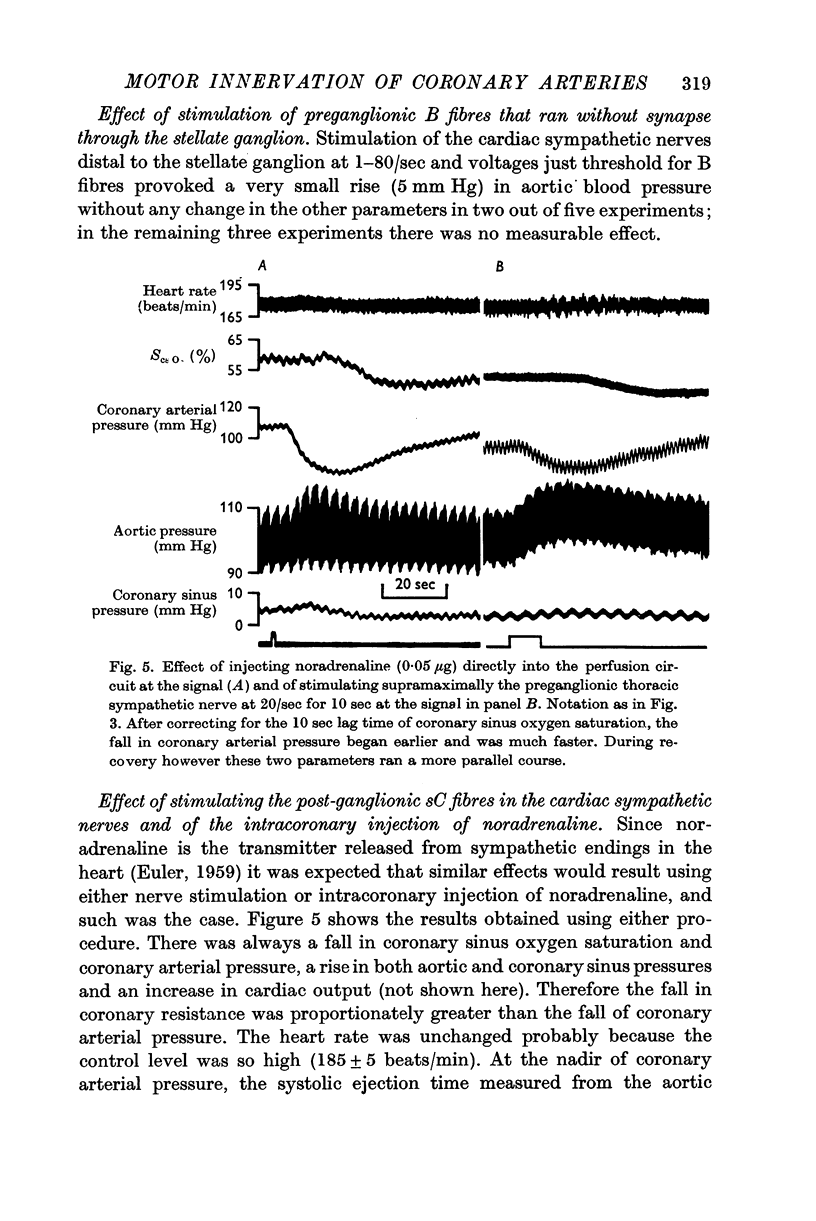
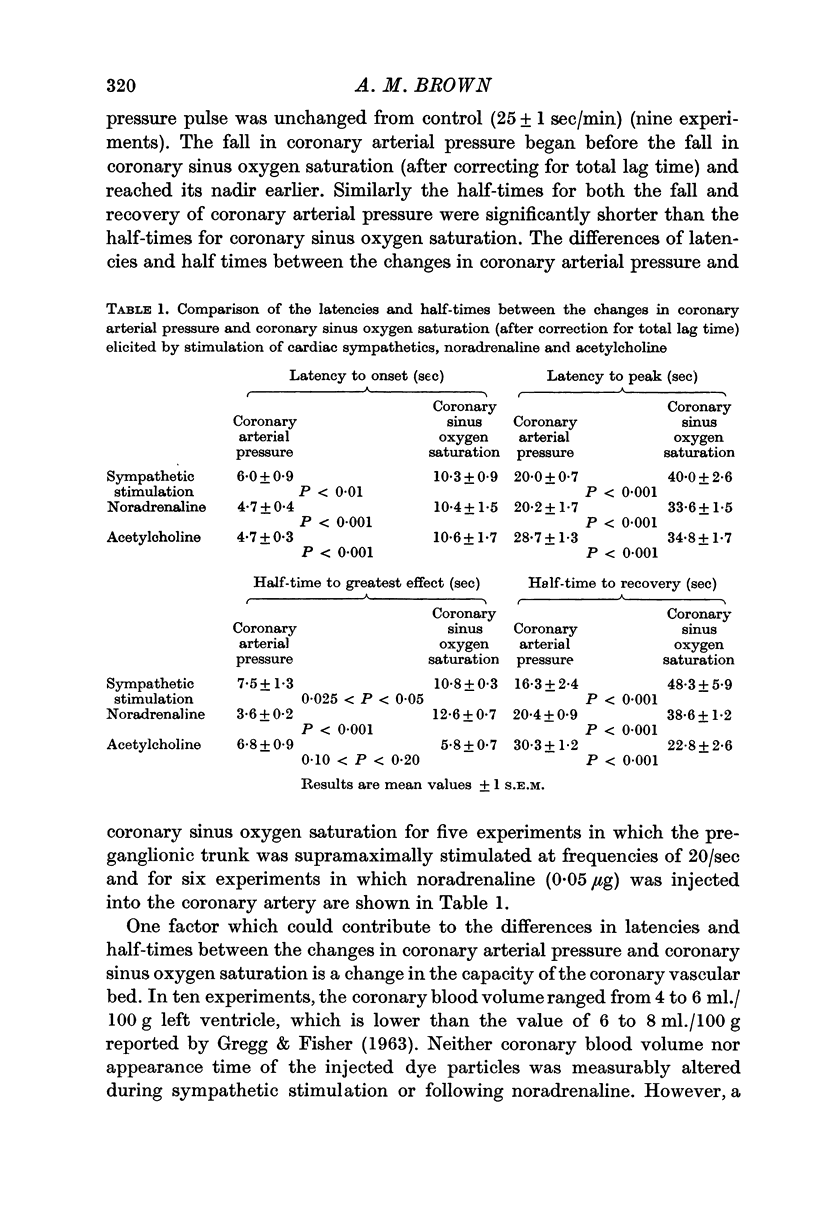
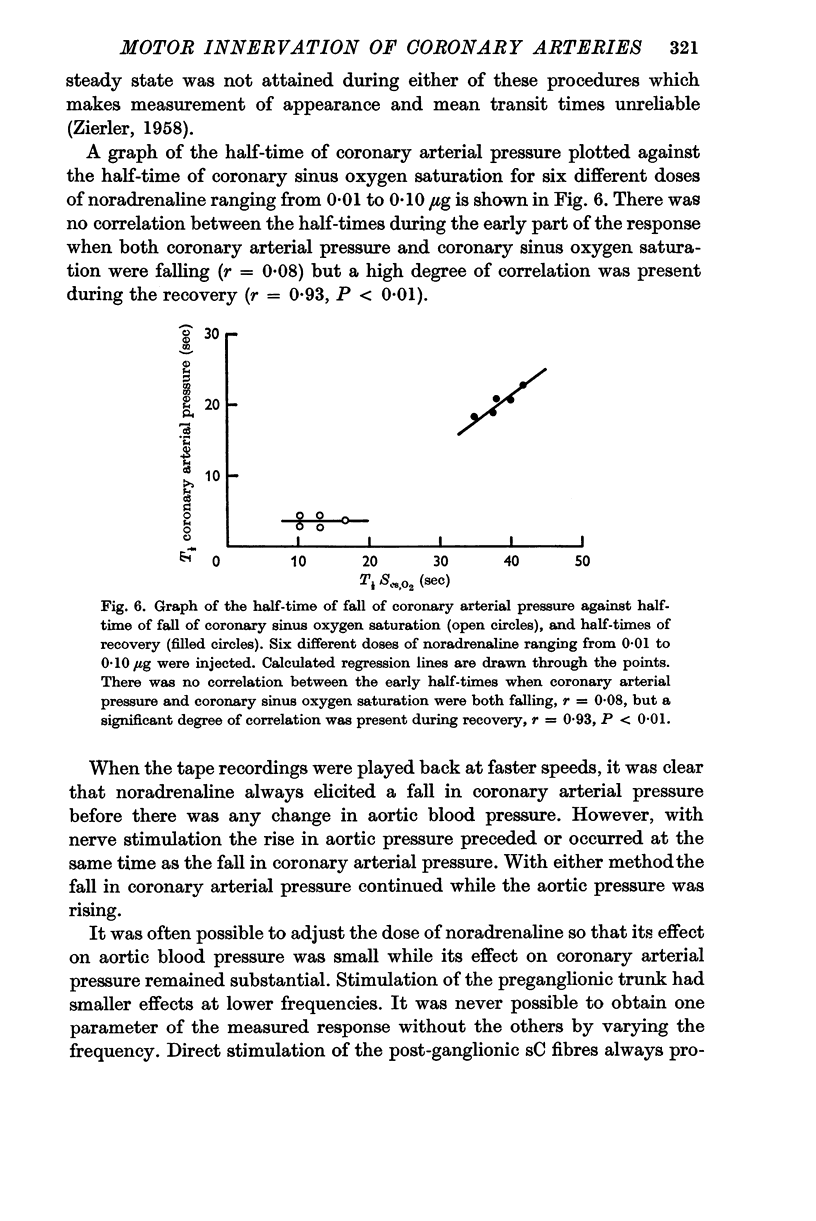
4. Stimulation of the post-ganglionic sC fibres of the cardiac sympathetic nerves caused coronary vasodilatation which occurred earlier than, and was initially independent of the decrease in coronary sinus oxygen saturation.
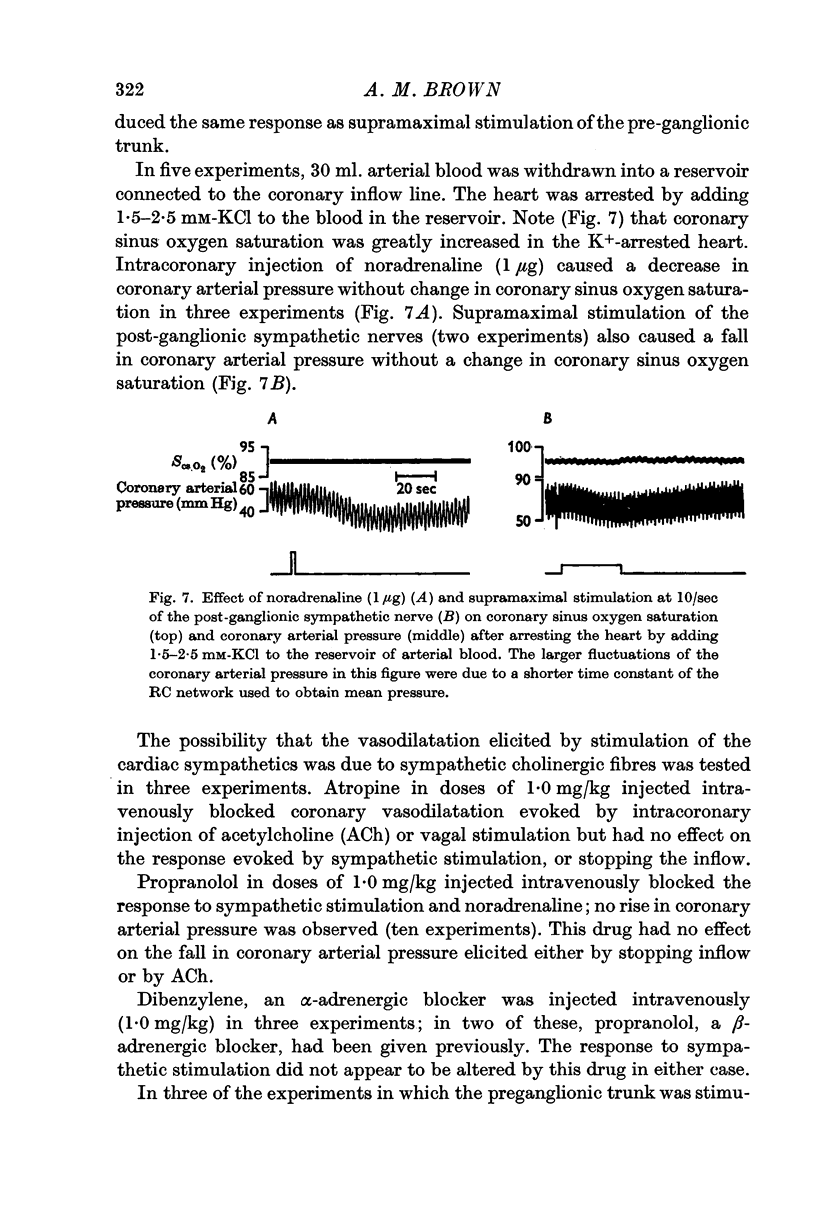
5. The injection of noradrenaline into the perfusion system had the same effect as stimulation of the sC fibres. In the K+-arrested heart, both noradrenaline and stimulation of the post-ganglionic nerves elicited coronary vasodilatation without changing the oxygen saturation of coronary sinus blood.
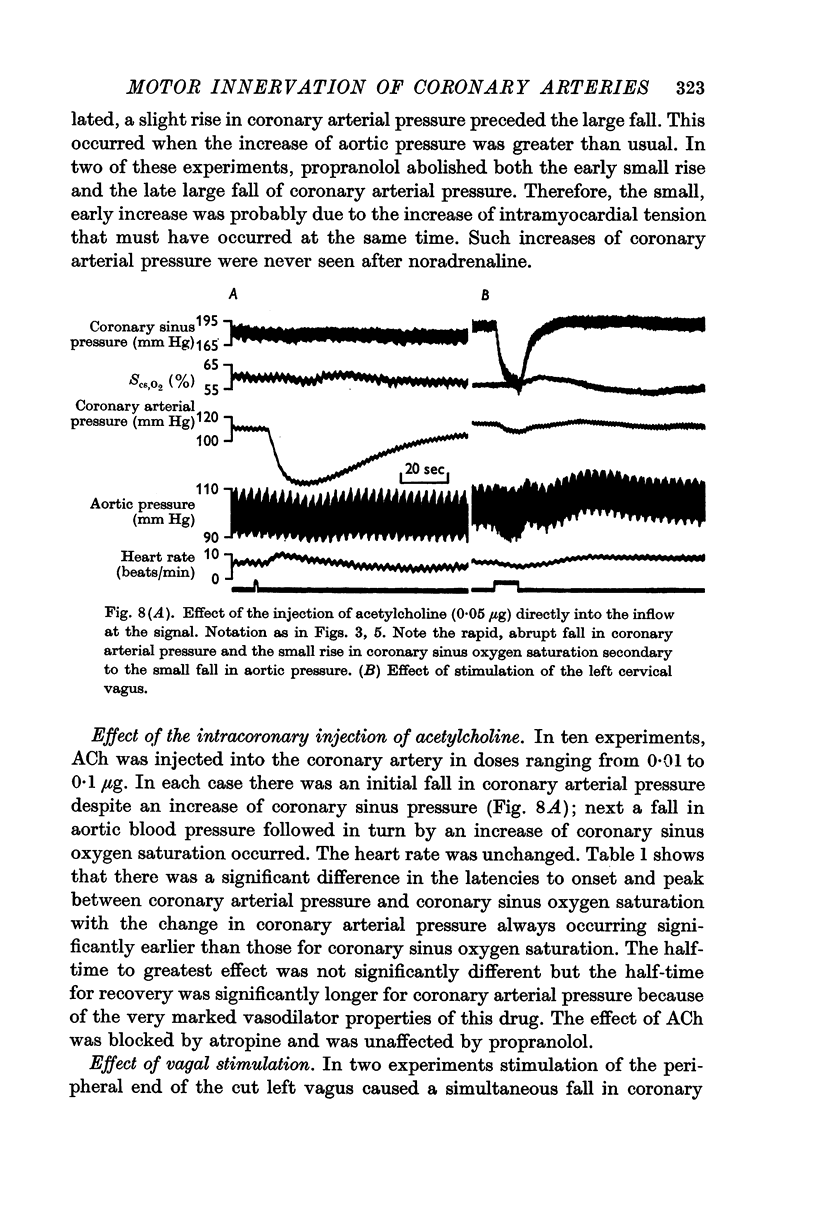
6. The intracoronary injection of acetylcholine caused coronary vasodilatation followed by an increase of coronary sinus oxygen saturation.
7. Vagal stimulation caused brady cardia and a fall in coronary resistance.
8. Propranolol blocked coronary vasodilatation elicited by sympathetic stimulation or noradrenaline without affecting the vasodilatation due to myocardial ischaemia or acetylcholine. Atropine blocked coronary vasodilatation evoked by acetylcholine without affecting that due to ischaemia or noradrenaline. Therefore smooth muscle of the coronary arteries has at least three different receptor sites from which vasodilatation can be elicited.
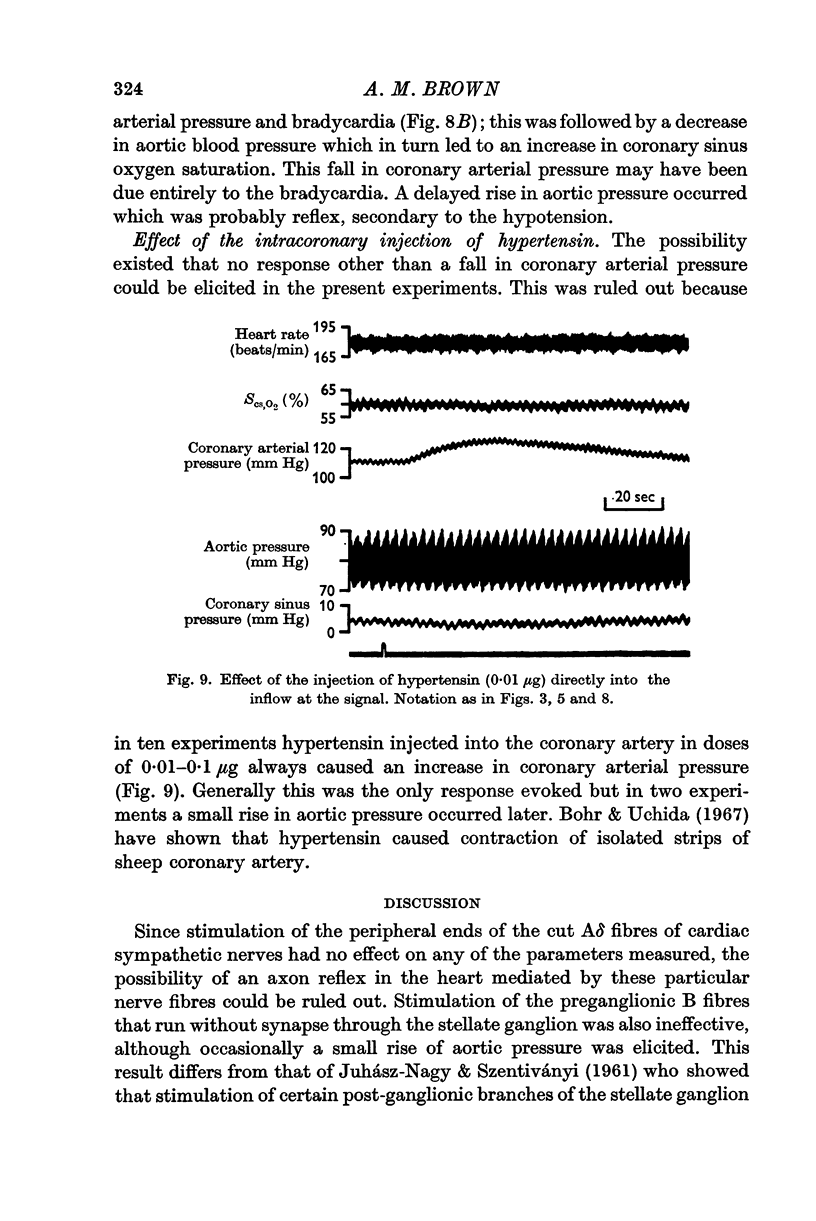
9. Hypertensin caused coronary vasoconstriction.
10. The presence of sympathetic cholinergic vasodilator fibres innervating the coronary arteries could not be demonstrated.
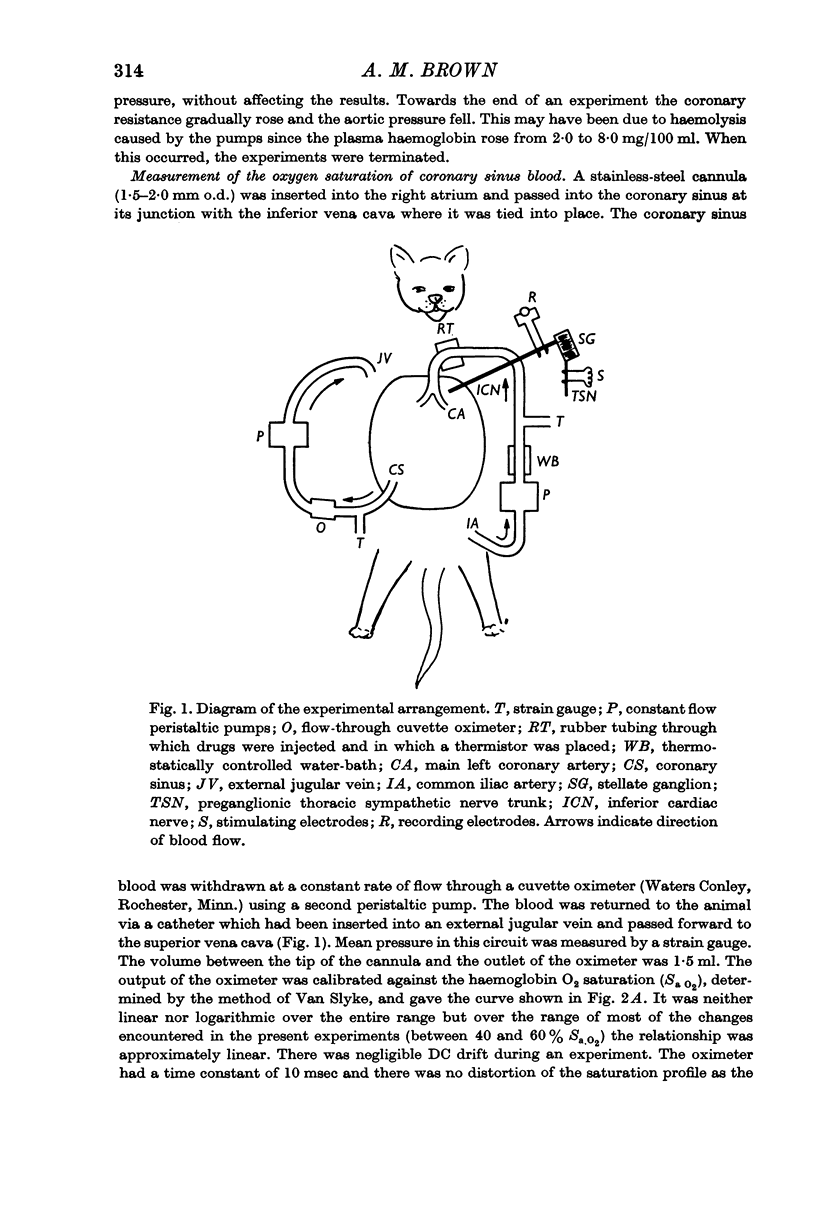
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson F. L., Brown A. M. Pulmonary vasoconstriction elicited by stimulation of the hypothalamic integrative area for the defense reaction. Circ Res. 1967 Nov;21(5):747–756. doi: 10.1161/01.res.21.5.747. [DOI] [PubMed] [Google Scholar]
- BERNE R. M. Effect of epinephrine and norepinephrine on coronary circulation. Circ Res. 1958 Sep;6(5):644–655. doi: 10.1161/01.res.6.5.644. [DOI] [PubMed] [Google Scholar]
- BERNE R. M. REGULATION OF CORONARY BLOOD FLOW. Physiol Rev. 1964 Jan;44:1–29. doi: 10.1152/physrev.1964.44.1.1. [DOI] [PubMed] [Google Scholar]
- BROWN A. M. MECHANORECEPTORS IN OR NEAR THE CORONARY ARTERIES. J Physiol. 1965 Mar;177:203–214. doi: 10.1113/jphysiol.1965.sp007586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohr D. F., Uchida E. Individualities of vascular smooth muscles in response to angiotensin. Circ Res. 1967 Jul;21(1 Suppl):135+–135+. [PubMed] [Google Scholar]
- Brown A. M. Cardiac sympathetic adrenergic pathways in which synaptic transmission is blocked by atropine sulfate. J Physiol. 1967 Jul;191(2):271–288. doi: 10.1113/jphysiol.1967.sp008250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A. M. Excitation of afferent cardiac sympathetic nerve fibres during myocardial ischaemia. J Physiol. 1967 May;190(1):35–53. doi: 10.1113/jphysiol.1967.sp008191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A. M. The depressor reflex arising from the left coronary artery of the cat. J Physiol. 1966 Jun;184(4):825–836. doi: 10.1113/jphysiol.1966.sp007950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ELIASSON S., FOLKOW B., LINDGREN P., UVNAS B. Activation of sympathetic vasodilator nerves to the skeletal muscles in the cat by hypothalamic stimulation. Acta Physiol Scand. 1951 Sep 21;23(4):333–351. doi: 10.1111/j.1748-1716.1951.tb00819.x. [DOI] [PubMed] [Google Scholar]
- Feigl E. O. Sympathetic control of coronary circulation. Circ Res. 1967 Feb;20(2):262–271. doi: 10.1161/01.res.20.2.262. [DOI] [PubMed] [Google Scholar]
- Gaal P. G., Kattus A. A., Kolin A., Ross G. Effects of adrenaline and noradrenaline on coronary blood flow before and after beta-adrenergic blockade. Br J Pharmacol Chemother. 1966 Mar;26(3):713–722. doi: 10.1111/j.1476-5381.1966.tb01851.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton R., Eichholtz F. The influence of chemical factors on the coronary circulation. J Physiol. 1925 Mar 31;59(6):413–425. doi: 10.1113/jphysiol.1925.sp002200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JUHASZ-NAGY A., SZENTIVANYI M. Separation of cardioaccelerator and coronary vasomotor fibers in the dog. Am J Physiol. 1961 Jan;200:125–129. doi: 10.1152/ajplegacy.1961.200.1.125. [DOI] [PubMed] [Google Scholar]
- KISS E., SZENTIVANYI M. Uber den segmentalen Ursprung der durch das Ganglion stellatum verlaufenden präganglionáren sympathischen Fasern. Acta Physiol Acad Sci Hung. 1957;11(3-4):339–345. [PubMed] [Google Scholar]
- NAPOLITANO L. M., WILLMAN V. L., HANLON C. R., COOPER T. INTRINSIC INNERVATION OF THE HEART. Am J Physiol. 1965 Mar;208:455–458. doi: 10.1152/ajplegacy.1965.208.3.455. [DOI] [PubMed] [Google Scholar]
- ZIERLER K. L. A simplified explanation of the theory of indicator-dilution for measurement of fluid flow and volume and other distributive phenomena. Bull Johns Hopkins Hosp. 1958 Oct;103(4):199–217. [PubMed] [Google Scholar]


