Abstract
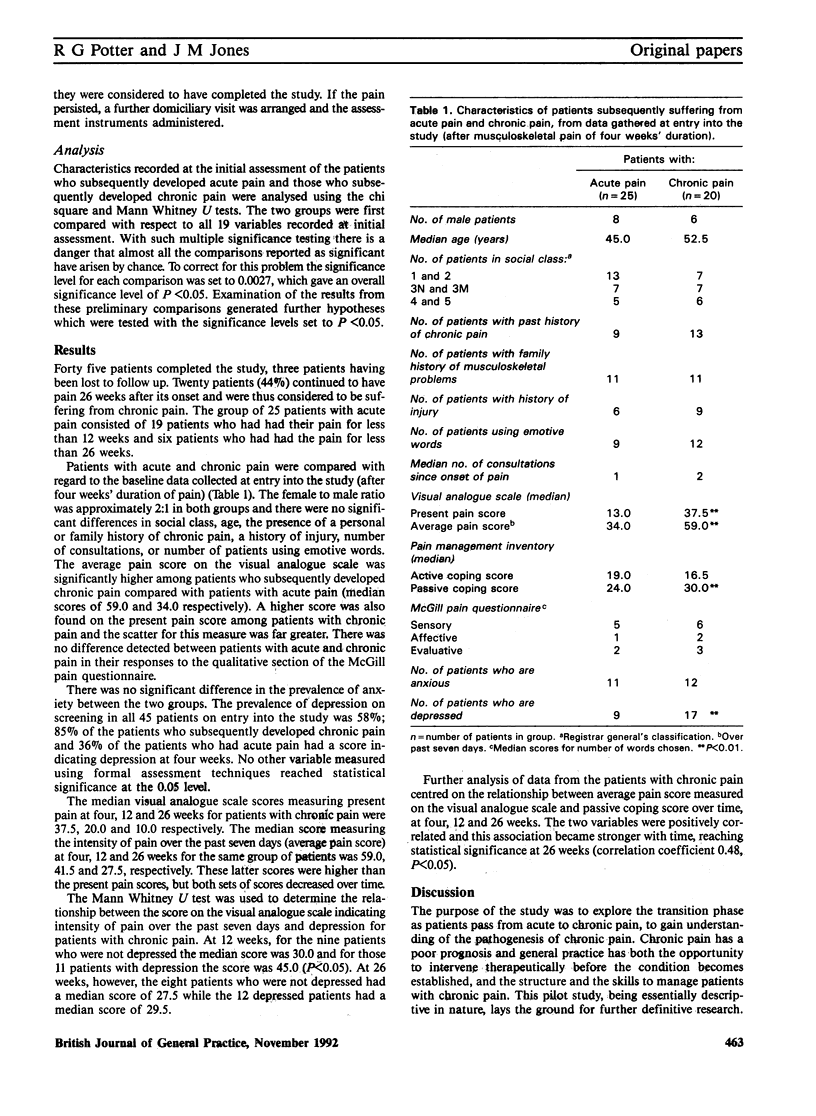
Little is known about the evolution of chronic pain in primary care. Forty five patients with a four week history of musculoskeletal pain were assessed and followed up over 26 weeks by a research nurse using a structured interview and formal assessment instruments. Patients aged 18 to 65 years were recruited on presentation at two semirural Cheshire general practices and subsequently interviewed on a domiciliary visit. Twenty patients (44%) continued to have pain at 26 weeks and these patients were considered to have chronic pain. Nineteen patients had no pain after 12 weeks and a further six had no pain after 26 weeks; these patients together formed the group with acute pain. Comparing the two groups at entry into the study (pain of four weeks' duration) demonstrated significantly higher visual analogue scale scores for intensity of pain (P < 0.01) and a higher incidence of depression (P < 0.01) in the group which subsequently developed chronic pain. In this group, the presence of depression at 12 weeks was associated with higher visual analogue scale scores (P < 0.05) but at 26 weeks scores were similar in depressed and non-depressed patients. The correlation between visual analogue scale score for intensity of pain and the use of passive coping strategies to cope with pain appeared more strongly positive with duration of pain (P < 0.05 at 26 weeks). It is suggested that high pain intensity scores, the presence of depression, and the increasing use of passive coping strategies may be identifiable associations with the development of chronic pain. Areas for further research are identified.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bridges K. W., Goldberg D. P. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29(6):563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- Brown G. K., Nicassio P. M. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987 Oct;31(1):53–64. doi: 10.1016/0304-3959(87)90006-6. [DOI] [PubMed] [Google Scholar]
- Frølund F., Frølund C. Pain in general practice. Pain as a cause of patient-doctor contact. Scand J Prim Health Care. 1986 May;4(2):97–100. doi: 10.3109/02813438609014810. [DOI] [PubMed] [Google Scholar]
- Goldberg D., Bridges K., Duncan-Jones P., Grayson D. Detecting anxiety and depression in general medical settings. BMJ. 1988 Oct 8;297(6653):897–899. doi: 10.1136/bmj.297.6653.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975 Sep;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- Philips H. C. Avoidance behaviour and its role in sustaining chronic pain. Behav Res Ther. 1987;25(4):273–279. doi: 10.1016/0005-7967(87)90005-2. [DOI] [PubMed] [Google Scholar]
- Potter R. G. Chronic non-malignant pain: time to take on the challenge. J R Coll Gen Pract. 1989 Dec;39(329):486–487. [PMC free article] [PubMed] [Google Scholar]
- Scott J., Huskisson E. C. Graphic representation of pain. Pain. 1976 Jun;2(2):175–184. [PubMed] [Google Scholar]


