Abstract
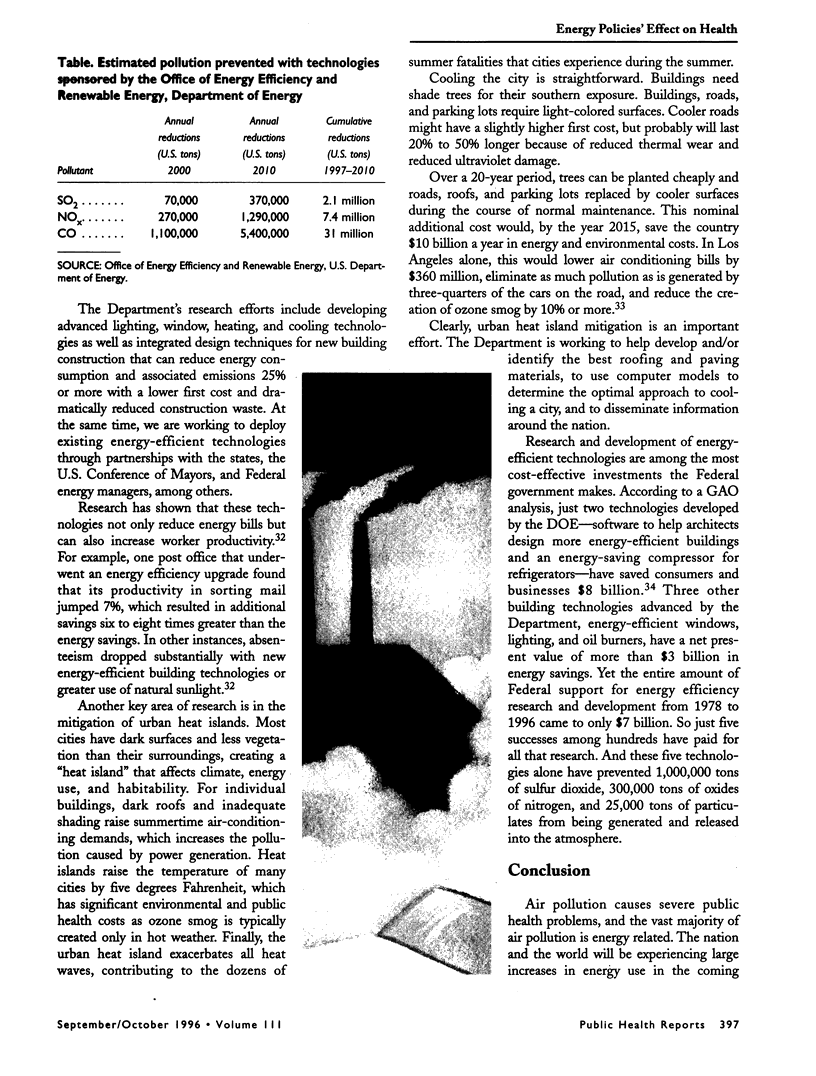
The connection between energy policy and increased levels of respiratory and cardiopulmonary disease has become clearer in the past few years. People living in cities with high levels of pollution have a higher risk of mortality than those living in less polluted cities. The pollutants most directly linked to increased morbidity and mortality include ozone, particulates, carbon monoxide, sulfur dioxide, volatile organic compounds, and oxides of nitrogen. Energy-related emissions generate the vast majority of these polluting chemicals. Technologies to prevent pollution in the transportation, manufacturing, building, and utility sectors can significantly reduce these emissions while reducing the energy bills of consumers and businesses. In short, clean energy technologies represent a very cost-effective investment in public health. Some 72% of the Federal government's investment in the research, development, and demonstration of pollution prevention technologies is made by the Department of Energy, with the largest share provided by the Office of Energy Efficiency and Renewable Energy. This article will examine the connections between air pollution and health problems and will discuss what the Department of Energy is doing to prevent air pollution now and in the future.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abbey D. E., Petersen F., Mills P. K., Beeson W. L. Long-term ambient concentrations of total suspended particulates, ozone, and sulfur dioxide and respiratory symptoms in a nonsmoking population. Arch Environ Health. 1993 Jan-Feb;48(1):33–46. doi: 10.1080/00039896.1993.9938391. [DOI] [PubMed] [Google Scholar]
- Dockery D. W., Pope C. A., 3rd, Xu X., Spengler J. D., Ware J. H., Fay M. E., Ferris B. G., Jr, Speizer F. E. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993 Dec 9;329(24):1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- Hall J. V., Winer A. M., Kleinman M. T., Lurmann F. W., Brajer V., Colome S. D. Valuing the health benefits of clean air. Science. 1992 Feb 14;255(5046):812–817. doi: 10.1126/science.1536006. [DOI] [PubMed] [Google Scholar]
- Hazucha M. J., Folinsbee L. J., Seal E., Bromberg P. A. Lung function response of healthy women after sequential exposures to NO2 and O3. Am J Respir Crit Care Med. 1994 Sep;150(3):642–647. doi: 10.1164/ajrccm.150.3.8087332. [DOI] [PubMed] [Google Scholar]
- Molfino N. A., Wright S. C., Katz I., Tarlo S., Silverman F., McClean P. A., Szalai J. P., Raizenne M., Slutsky A. S., Zamel N. Effect of low concentrations of ozone on inhaled allergen responses in asthmatic subjects. Lancet. 1991 Jul 27;338(8761):199–203. doi: 10.1016/0140-6736(91)90346-q. [DOI] [PubMed] [Google Scholar]
- Neas L. M., Dockery D. W., Ware J. H., Spengler J. D., Speizer F. E., Ferris B. G., Jr Association of indoor nitrogen dioxide with respiratory symptoms and pulmonary function in children. Am J Epidemiol. 1991 Jul 15;134(2):204–219. doi: 10.1093/oxfordjournals.aje.a116073. [DOI] [PubMed] [Google Scholar]
- Neas L. M., Dockery D. W., Ware J. H., Spengler J. D., Speizer F. E., Ferris B. G., Jr Association of indoor nitrogen dioxide with respiratory symptoms and pulmonary function in children. Am J Epidemiol. 1991 Jul 15;134(2):204–219. doi: 10.1093/oxfordjournals.aje.a116073. [DOI] [PubMed] [Google Scholar]
- Pope C. A., 3rd, Thun M. J., Namboodiri M. M., Dockery D. W., Evans J. S., Speizer F. E., Heath C. W., Jr Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med. 1995 Mar;151(3 Pt 1):669–674. doi: 10.1164/ajrccm/151.3_Pt_1.669. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for the elderly in Birmingham, Alabama. Am J Epidemiol. 1994 Mar 15;139(6):589–598. doi: 10.1093/oxfordjournals.aje.a117048. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for the elderly in Detroit, Michigan. Am J Respir Crit Care Med. 1994 Sep;150(3):648–655. doi: 10.1164/ajrccm.150.3.8087333. [DOI] [PubMed] [Google Scholar]
- Schwartz J. PM10, ozone, and hospital admissions for the elderly in Minneapolis-St. Paul, Minnesota. Arch Environ Health. 1994 Sep-Oct;49(5):366–374. doi: 10.1080/00039896.1994.9954989. [DOI] [PubMed] [Google Scholar]
- Schwartz J. What are people dying of on high air pollution days? Environ Res. 1994 Jan;64(1):26–35. doi: 10.1006/enrs.1994.1004. [DOI] [PubMed] [Google Scholar]
- Sheppard D., Wong W. S., Uehara C. F., Nadel J. A., Boushey H. A. Lower threshold and greater bronchomotor responsiveness of asthmatic subjects to sulfur dioxide. Am Rev Respir Dis. 1980 Dec;122(6):873–878. doi: 10.1164/arrd.1980.122.6.873. [DOI] [PubMed] [Google Scholar]
- Weiss K. B., Gergen P. J., Hodgson T. A. An economic evaluation of asthma in the United States. N Engl J Med. 1992 Mar 26;326(13):862–866. doi: 10.1056/NEJM199203263261304. [DOI] [PubMed] [Google Scholar]